We have read the recent histopathological review entitled: “acute respiratory distress” (ARD)1 with interest. However, we found that the publication made no mention of ARD associated to blood transfusion.2 A differential diagnosis must be established among transfusion-related acute respiratory distress (TRD), transfusion-related acute lung injury (TRALI), and cardiogenic lung edema or transfusion-associated circulatory overload (TACO).4
Transfusion-related acute lung injury is defined as “acute dyspnea with hypoxia and bilateral pulmonary infiltrates during or in the 6 hours after transfusion, unrelated to overload or other likely causes”.3 The presence of TRALI is to be suspected in “patients without evidence of acute lung injury prior to transfusion” who develop ARD.3Table 1 describes the diagnostic criteria. Transfusion-related acute lung injury is a clinical syndrome, and the presence of antibodies is not strictly necessary to establish the diagnosis.4
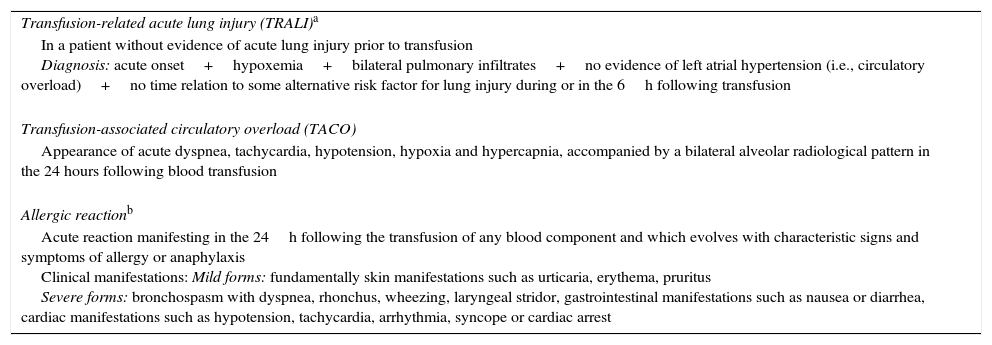
Definitions and diagnosis of transfusion-related acute respiratory distress.
| Transfusion-related acute lung injury (TRALI)a |
| In a patient without evidence of acute lung injury prior to transfusion Diagnosis: acute onset+hypoxemia+bilateral pulmonary infiltrates+no evidence of left atrial hypertension (i.e., circulatory overload)+no time relation to some alternative risk factor for lung injury during or in the 6h following transfusion |
| Transfusion-associated circulatory overload (TACO) |
| Appearance of acute dyspnea, tachycardia, hypotension, hypoxia and hypercapnia, accompanied by a bilateral alveolar radiological pattern in the 24 hours following blood transfusion |
| Allergic reactionb |
| Acute reaction manifesting in the 24h following the transfusion of any blood component and which evolves with characteristic signs and symptoms of allergy or anaphylaxis Clinical manifestations: Mild forms: fundamentally skin manifestations such as urticaria, erythema, pruritus Severe forms: bronchospasm with dyspnea, rhonchus, wheezing, laryngeal stridor, gastrointestinal manifestations such as nausea or diarrhea, cardiac manifestations such as hypotension, tachycardia, arrhythmia, syncope or cardiac arrest |
Source: Adapted from the State Hemovigilance report.4
Transfusion-associated circulatory overload lacks a consensus-based definition. According to the current definition of the International Society of Blood Transfusion (ongoing revision),3 any four of the following conditions must be met within the first 6h after transfusion: acute respiratory failure, tachycardia, increased arterial pressure, acute lung edema or worsening of edema, or evidence of a positive fluid balance. The diagnosis is established on an exclusion basis and requires a high degree of suspicion3: “TACO is to be suspected in the presence of respiratory difficulties that improve with treatment for circulatory overload (diuretics, morphine and nitrates)”, and “it is important to report these cases”. The experts that review these cases find it difficult to classify them–often because the essential data are not available and the transfused patients are frequently elderly (over 70% of the units being administered to patients over 70 years of age) or in critical condition (over 40% in emergency care or in Intensive Care Units), and with considerable comorbidities.5 Furthermore, some patients may have both TRALI and TACO.3
In 2014, a total of 64 cases of TACO and 30 cases of TRALI were reported in Spain, versus 76 and 30 cases, respectively, in 2013. Any blood component can be implicated in TRALI: red cells (15 patient), platelets (5 patients), plasma (7 patients) or multiple components (3 patients).
In Spain, one-half of all transfusion-related deaths were due to ARD. Of the 30 cases associated to transfusion reported since 2007, 10 corresponded to TRALI and 5 to TACO. In the United Kingdom, of the 93 transfusion-related deaths recorded between 2010 and 2015, 55% corresponded to ARD associated to allogenic blood transfusion: 39 cases of TACO, 9 cases of TRALI and three cases of TRD.
In view of the above, and considering the clinical importance, healthcare impact and therapeutic relevance involved, we consider it essential to contemplate episodes of ARD associated to blood transfusion in this document. Likewise, we wish to underscore the obligation to report all cases to the hematological surveillance system, and the fact that “one unit may be enough”.
Conflicts of interestThere are no conflicts of interest in relation to this study.
Dr. García-Erce has given talks and has acted as moderator at congresses and sessions, with grants or funding from Vifor-España, Sandoz, Amgen, Alexion, Braun, GSK, Octapharma, Novartis and Sanofi.
Thanks are due to all those transfusion centers that supply the best and freshest blood components.
Please cite this article as: García Erce JA, Quintana Díaz M. Distrés respiratorio agudo secundario a la transfusión sanguínea. Med Intensiva. 2017;41:444–445.