A paediatric intensive care unit (PICU) is a separate physical facility or unit specifically designed for the treatment of paediatric patients who, because of the severity of illness or other life-threatening conditions, require comprehensive and continuous intensive care by a medical team with special skills in paediatric intensive care medicine. Timely and personal intervention in intensive care reduces mortality, reduces length of stay, and decreases cost of care. With the aim of defending the right of the child to receive the highest attainable standard of health and the facilities for the treatment of illness and rehabilitation, as well as ensuring the quality of care and the safety of critically ill paediatric patients, the Spanish Association of Paediatrics (AEP), Spanish Society of Paediatric Intensive Care (SECIP) and Spanish Society of Critical Care (SEMICYUC) have approved the guidelines for the admission, discharge and triage for Spanish PICUs. By using these guidelines, the performance of Spanish paediatric intensive care units can be optimised and paediatric patients can receive the appropriate level of care for their clinical condition.
La unidad de cuidados intensivos pediátricos (UCIP) es una unidad física asistencial hospitalaria independiente especialmente diseñada para el tratamiento de pacientes pediátricos quienes debido su gravedad o condiciones potencialmente letales requieren observación y asistencia médica intensiva integral y continua por un equipo médico que haya obtenido competencia especial en medicina intensiva pediátrica. La aplicación oportuna de terapia intensiva a los pacientes críticos reduce la mortalidad, el tiempo de estancia y los costes asistenciales. Con los objetivos de respetar el derecho del niño al disfrute del más alto nivel posible de salud y a servicios para el tratamiento de las enfermedades y la rehabilitación de la salud y de garantizar la calidad asistencial y la seguridad de los pacientes pediátricos críticos, la Asociación Española de Pediatría (AEP), la Sociedad Española de Cuidados Intensivos Pediátricos (SECIP) y la Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias (SEMICYUC) han desarrollado y aprobado las guías de ingreso, alta y triage para las UCIP en España. Mediante la aplicación de estas guías se puede optimizar el uso de las UCIP españolas de forma que los pacientes pediátricos reciban el nivel de cuidados médicos más apropiado para su situación clínica.
Clinical practice in paediatric intensive care has improved drastically in the past 4 decades thanks to a growing understanding of the pathophysiology of life-threatening processes, technological advances in the monitoring, diagnosis and treatment of critically ill paediatric patients and the specialised training of the health care staff that manages critically ill paediatric patients.
The paediatric intensive care unit (PICU) was defined in 1983 in the Guidelines for Paediatric Intensive Care1 (updated in 20042) as “a hospital unit that provides treatment to children with a wide variety of illnesses of a life-threatening nature, including children with highly unstable conditions and those requiring sophisticated medical and surgical intervention.” Randolph et al.3 expanded this definition: “A PICU is a separate physical facility or unit specifically designated for the treatment of paediatric patients who, because of shock, trauma, or other life-threatening conditions, require intensified, comprehensive observation and care.”
At the beginning of the new millennium, the board of directors of the European Union of Medical Specialists (UEMS) approved the definition of intensive care medicine for the European Union proposed by the Multidisciplinary Joint Committee of Intensive Care Medicine (MJCICM)4: “Intensive care medicine [e.g. paediatric intensive care] combines physicians, nurses and allied health professionals in the coordinated and collaborative management of patients with life-threatening single or multiple organ system failure, including stabilisation after severe surgical interventions. It is a continuous (i.e. 24h) management including monitoring, diagnostics, support of failing vital functions as well as the treatment of the underlying diseases.”
The MJCICM4 also underscored that “patient care should be provided continuously over a 24h period, by staff members (physicians) who have obtained special competence in intensive care medicine” (e.g. paediatric intensive care). Indeed, adequate training of physicians and nurses is essential to ensure the quality of intensive care and the safety of the patient in the PICU.4–7
Early diagnosis and treatment are essential to the survival of critically ill patients, especially those with neurologic decompensation, haemodynamic instability or signs of tissue hypoxia and organ dysfunction. Although these signs can be detected with clinical observation, advanced monitoring at the ICU may facilitate faster decision-making.8 Furthermore, delays in PICU admission may increase the risk of death,9,10 while implementation of early intensive treatment in critically ill patients or patients that are quickly deteriorating outside the PICU is associated with decreased mortality.11–13
The Spanish Constitution recognises the right to health in Spain. The World Health Organization affirms that the right to health includes “access to timely, acceptable, and affordable health care of appropriate quality.”
In 1990, the Spanish government approved and ratified the Convention on the Rights of the Child adopted by the United Nations General Assembly,14 and article 24 of this instrument states “1. States Parties recognize the right of the child to the enjoyment of the highest attainable standard of health and to facilities for the treatment of illness and the rehabilitation of health. States Parties shall strive to ensure that no child is deprived of his or her right of access to such health care services. 2. States Parties shall pursue full implementation of this right and, in particular, shall take appropriate measures: … (b) To ensure the provision of necessary medical assistance and health care to all children …” Furthermore, the European Charter for Children in Hospital15 establishes, among others, the fundamental rights of children and adolescents to receive “the best possible medical treatment … to be cared for throughout their hospital stay by appropriately trained staff, fully aware of the physical and emotional needs of each age group … [and] to be cared for in hospital with other children, avoiding as far as possible admission to adult wards.”
Therefore, we must remain aware that critically ill children with potentially life-threatening single or multiple organ or system impairment or failure, including the need of stabilisation after severe surgical intervention, should be, wherever possible, placed in units dedicated exclusively to children,2 managed by staff specifically accredited in paediatric critical care capable of providing integral, comprehensive and continuous care, carrying out the specialised interventions required by severe organ or system dysfunction in children and adolescents, and implementing the specific care protocols required for monitoring, diagnosis, support of failing vital functions and treatment of underlying disases.4,6,16
With the aim of upholding the right of children to enjoy the highest attainable standard of health and services for the treatment of illness and the rehabilitation of health and guaranteeing the quality of care and the safety of paediatric critical patients, the boards of directors of the Asociación Española de Pediatría (Spanish Association of Paediatrics [AEP]), the Sociedad Española de Cuidados Intensivos Pediátricos (Spanish Society of Paediatric Intensive Care [SECIP]) and the Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias (Spanish Society of Intensive and Critical Care Medicine and Coronary Units [SEMICYUC]) created paediatric intensive care standards committees in their respective societies, which in turn developed and approved the guidelines for Spanish PICUs presented in this article. The members of the standards committees were selected by their respective societies based on their clinical practice and management expertise and their education among recognised experts in paediatrics and paediatric critical care (AEP, SECIP) and intensive medicine (SEMICYUC) in Spain, while seeking adequate representation of the involved societies and other institutions associated with the pertinent medical specialties.
We have developed these guidelines on the basis of the guidelines published in 1999 by the Society of Critical Care Medicine in collaboration with the American College of Critical Care Medicine and the Committee on Hospital Care of the American Academy of Pediatrics,16 which we completed and updated with information obtained through a literature search in MEDLINE (Ovid), Embase and PubMed for articles published between January 1999 and April 2017 with the search terms pediatric intensive care units, pediatric critical care, admission, triage, discharge, pediatric intensive care/critical care outreach programs, benefit, futility, rationing, quality assurance/quality improvement, timely and guidelines, guidelines published by scientific associations17–25 and updated editions of internationally known reference books on clinical practice in paediatric intensive care.26,27 The guidelines also include general criteria to guide PICU triage based on the recommendations published by the ICU Admission Discharge and Triage (ADT) Task Force8 and the Task Force of the World Federation of Societies of Intensive and Critical Care Medicine.13 We were unable to establish levels of scientific evidence due to the scarcity of data in the paediatric age group.
These guidelines are meant as a reference for practice and may facilitate decision-making regarding admission, discharge and triage of critically ill paediatric patients in Spanish PICUs, guiding the classification of patients into the most appropriate level of care based on the need for intensive care/monitoring and how likely they are to benefit or not from intensive care.8 Due to the ongoing advances in paediatric intensive care, we recommend that these guidelines be updated at regular intervals.
This document is not meant to replace the use of clinical judgement in individual cases. Paediatric intensivists may request admission to the PICU for patients at risk of deterioration, with clinical manifestations of severe illness or with intensive monitoring or observation needs not included in these guidelines. Whatever the circumstances, any decision regarding admission, discharge and triage and its justification must be documented in the health records of the patient.
Criteria for admission to the paediatric intensive care unitIt is essential to weigh the potential risks and benefits of intensive care in patients considered for PICU admission. Ideally, admission to the PICU should be granted to all patients with reversible disease whose risk of death would decrease with the use of advanced technologies and delivery of medical care by a team with specialised training in paediatric critical care.8 However, intensive treatment and monitoring may increase morbidity, so extremely ill patients with a low probability of survival may not ultimately benefit from admission to the PICU, while patients that only require monitoring for preventive purposes and who are not severely ill are unlikely to benefit from transfer to this level of care.
Admission to the PICU must always be considered in patients that may benefit from intensive care. Decisions regarding the admission to the PICU of terminal patients with a low probability of survival or with irreversible diseases should be based on qualitative criteria regarding the potential benefit or lack thereof of intensive care.8 We recommend using the term “potentially inappropriate” as opposed to “futile” to refer to treatment at the PICU level that has some chance to achieve the effect sought by the patient or family but which the intensivists or other professionals in charge of the patient are opposed to implementing on account of ethical considerations.28,29 In certain situations, the PICU may be the most appropriate setting to perform treatments and procedures aimed to prolong survival or improve quality of life in terminally ill patients with appropriate comfort, and there are also situations where the PICU may be the ideal setting for specially-trained physicians and nurses to provide appropriate end-of-life palliative care to terminally ill children and adolescents.
Generally speaking, admission to the PICU should be granted to any paediatric patient—especially cancer patients or bone marrow transplant recipients—at risk of severe acute deterioration, neurologic decompensation, haemodynamic instability or failure or life-threatening dysfunction of at least one vital organ or system30,31 or multiple organ or system failure, requiring stabilisation following severe surgical intervention or with pre- or post-operative conditions potentially associated with severe or life-threatening dysfunction of at least one organ or system, or who due to the severity or potential severity of their condition require invasive and/or continuous monitoring, diagnosis and support of failing vital functions or treatment of underlying diseases by a team specifically trained in paediatric intensive care.
We proceed to specify the conditions that require admission to PICU related to multiple organ involvement and with the organs or systems that are most frequently involved (Tables 1–8).
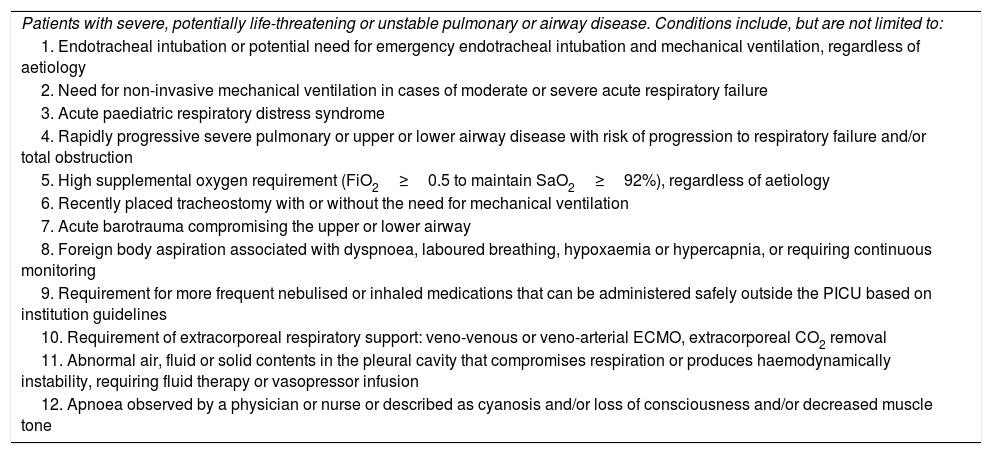
PICU admission criteria related to the respiratory system.
| Patients with severe, potentially life-threatening or unstable pulmonary or airway disease. Conditions include, but are not limited to: |
| 1. Endotracheal intubation or potential need for emergency endotracheal intubation and mechanical ventilation, regardless of aetiology |
| 2. Need for non-invasive mechanical ventilation in cases of moderate or severe acute respiratory failure |
| 3. Acute paediatric respiratory distress syndrome |
| 4. Rapidly progressive severe pulmonary or upper or lower airway disease with risk of progression to respiratory failure and/or total obstruction |
| 5. High supplemental oxygen requirement (FiO2≥0.5 to maintain SaO2≥92%), regardless of aetiology |
| 6. Recently placed tracheostomy with or without the need for mechanical ventilation |
| 7. Acute barotrauma compromising the upper or lower airway |
| 8. Foreign body aspiration associated with dyspnoea, laboured breathing, hypoxaemia or hypercapnia, or requiring continuous monitoring |
| 9. Requirement for more frequent nebulised or inhaled medications that can be administered safely outside the PICU based on institution guidelines |
| 10. Requirement of extracorporeal respiratory support: veno-venous or veno-arterial ECMO, extracorporeal CO2 removal |
| 11. Abnormal air, fluid or solid contents in the pleural cavity that compromises respiration or produces haemodynamically instability, requiring fluid therapy or vasopressor infusion |
| 12. Apnoea observed by a physician or nurse or described as cyanosis and/or loss of consciousness and/or decreased muscle tone |
CO2, carbon dioxide; ECMO, extracorporeal membrane oxygenation; FiO2, fraction of inspired oxygen; PICU, paediatric intensive care unit; SaO2, arterial oxygen saturation.
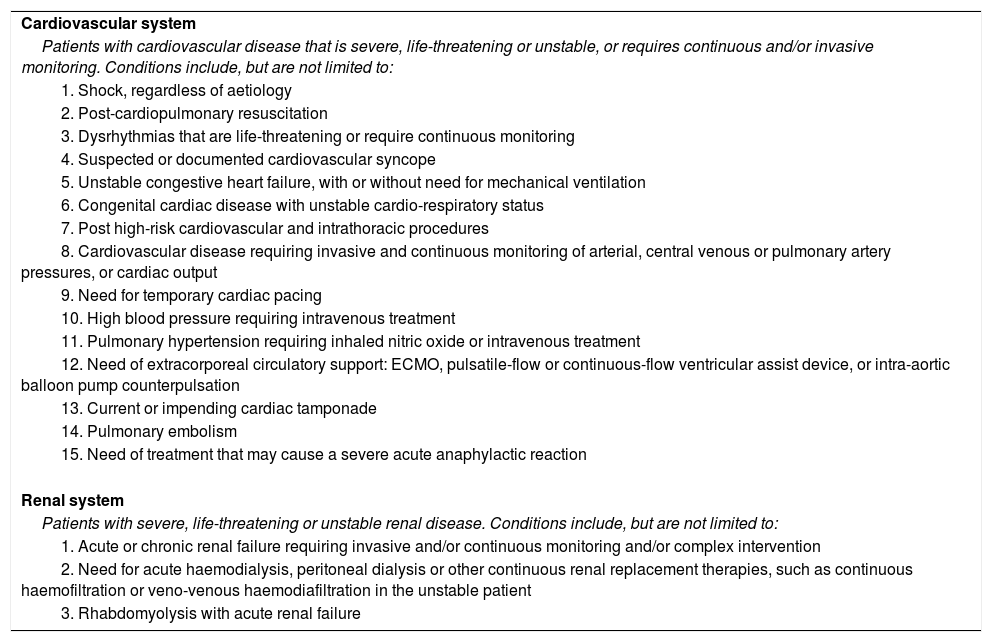
PICU admission criteria related to the cardiovascular and renal systems.
| Cardiovascular system |
| Patients with cardiovascular disease that is severe, life-threatening or unstable, or requires continuous and/or invasive monitoring. Conditions include, but are not limited to: |
| 1. Shock, regardless of aetiology |
| 2. Post-cardiopulmonary resuscitation |
| 3. Dysrhythmias that are life-threatening or require continuous monitoring |
| 4. Suspected or documented cardiovascular syncope |
| 5. Unstable congestive heart failure, with or without need for mechanical ventilation |
| 6. Congenital cardiac disease with unstable cardio-respiratory status |
| 7. Post high-risk cardiovascular and intrathoracic procedures |
| 8. Cardiovascular disease requiring invasive and continuous monitoring of arterial, central venous or pulmonary artery pressures, or cardiac output |
| 9. Need for temporary cardiac pacing |
| 10. High blood pressure requiring intravenous treatment |
| 11. Pulmonary hypertension requiring inhaled nitric oxide or intravenous treatment |
| 12. Need of extracorporeal circulatory support: ECMO, pulsatile-flow or continuous-flow ventricular assist device, or intra-aortic balloon pump counterpulsation |
| 13. Current or impending cardiac tamponade |
| 14. Pulmonary embolism |
| 15. Need of treatment that may cause a severe acute anaphylactic reaction |
| Renal system |
| Patients with severe, life-threatening or unstable renal disease. Conditions include, but are not limited to: |
| 1. Acute or chronic renal failure requiring invasive and/or continuous monitoring and/or complex intervention |
| 2. Need for acute haemodialysis, peritoneal dialysis or other continuous renal replacement therapies, such as continuous haemofiltration or veno-venous haemodiafiltration in the unstable patient |
| 3. Rhabdomyolysis with acute renal failure |
ECMO, extracorporeal membrane oxygenation; PICU, paediatric intensive care unit.
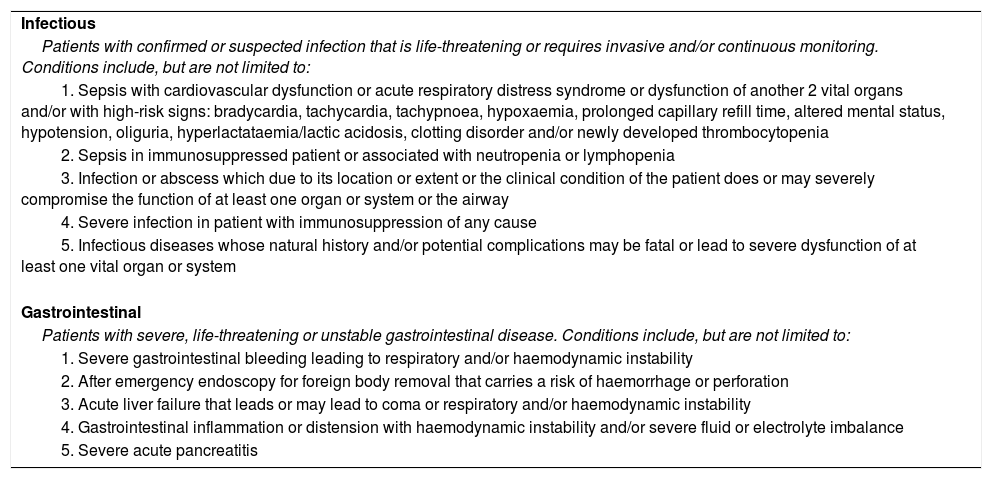
Criteria for PICU admission related to infection and to the gastrointestinal tract.
| Infectious |
| Patients with confirmed or suspected infection that is life-threatening or requires invasive and/or continuous monitoring. Conditions include, but are not limited to: |
| 1. Sepsis with cardiovascular dysfunction or acute respiratory distress syndrome or dysfunction of another 2 vital organs and/or with high-risk signs: bradycardia, tachycardia, tachypnoea, hypoxaemia, prolonged capillary refill time, altered mental status, hypotension, oliguria, hyperlactataemia/lactic acidosis, clotting disorder and/or newly developed thrombocytopenia |
| 2. Sepsis in immunosuppressed patient or associated with neutropenia or lymphopenia |
| 3. Infection or abscess which due to its location or extent or the clinical condition of the patient does or may severely compromise the function of at least one organ or system or the airway |
| 4. Severe infection in patient with immunosuppression of any cause |
| 5. Infectious diseases whose natural history and/or potential complications may be fatal or lead to severe dysfunction of at least one vital organ or system |
| Gastrointestinal |
| Patients with severe, life-threatening or unstable gastrointestinal disease. Conditions include, but are not limited to: |
| 1. Severe gastrointestinal bleeding leading to respiratory and/or haemodynamic instability |
| 2. After emergency endoscopy for foreign body removal that carries a risk of haemorrhage or perforation |
| 3. Acute liver failure that leads or may lead to coma or respiratory and/or haemodynamic instability |
| 4. Gastrointestinal inflammation or distension with haemodynamic instability and/or severe fluid or electrolyte imbalance |
| 5. Severe acute pancreatitis |
PICU, paediatric intensive care unit.
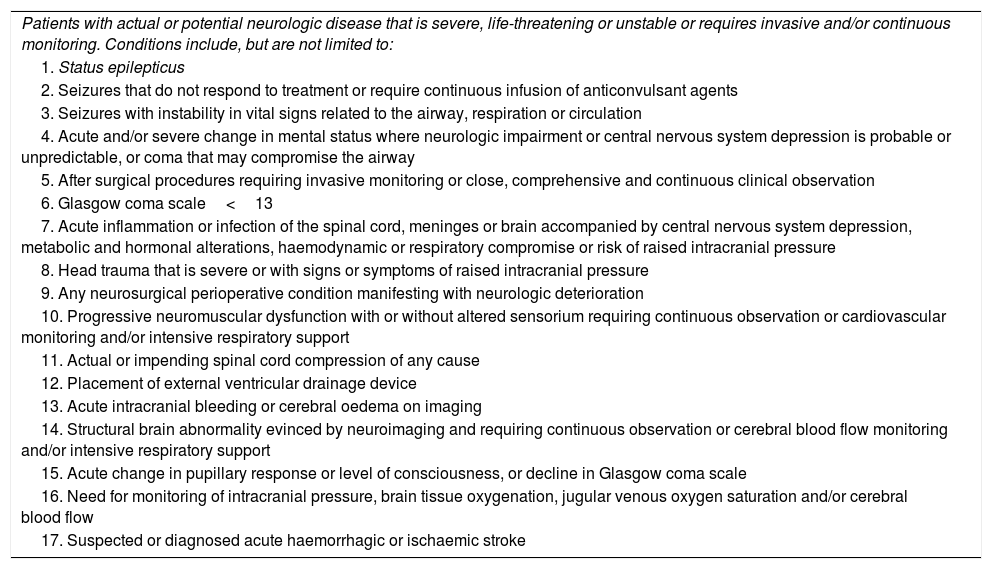
Criteria for PICU admission related to the patient's neurologic condition.
| Patients with actual or potential neurologic disease that is severe, life-threatening or unstable or requires invasive and/or continuous monitoring. Conditions include, but are not limited to: |
| 1. Status epilepticus |
| 2. Seizures that do not respond to treatment or require continuous infusion of anticonvulsant agents |
| 3. Seizures with instability in vital signs related to the airway, respiration or circulation |
| 4. Acute and/or severe change in mental status where neurologic impairment or central nervous system depression is probable or unpredictable, or coma that may compromise the airway |
| 5. After surgical procedures requiring invasive monitoring or close, comprehensive and continuous clinical observation |
| 6. Glasgow coma scale<13 |
| 7. Acute inflammation or infection of the spinal cord, meninges or brain accompanied by central nervous system depression, metabolic and hormonal alterations, haemodynamic or respiratory compromise or risk of raised intracranial pressure |
| 8. Head trauma that is severe or with signs or symptoms of raised intracranial pressure |
| 9. Any neurosurgical perioperative condition manifesting with neurologic deterioration |
| 10. Progressive neuromuscular dysfunction with or without altered sensorium requiring continuous observation or cardiovascular monitoring and/or intensive respiratory support |
| 11. Actual or impending spinal cord compression of any cause |
| 12. Placement of external ventricular drainage device |
| 13. Acute intracranial bleeding or cerebral oedema on imaging |
| 14. Structural brain abnormality evinced by neuroimaging and requiring continuous observation or cerebral blood flow monitoring and/or intensive respiratory support |
| 15. Acute change in pupillary response or level of consciousness, or decline in Glasgow coma scale |
| 16. Need for monitoring of intracranial pressure, brain tissue oxygenation, jugular venous oxygen saturation and/or cerebral blood flow |
| 17. Suspected or diagnosed acute haemorrhagic or ischaemic stroke |
PICU, paediatric intensive care unit.
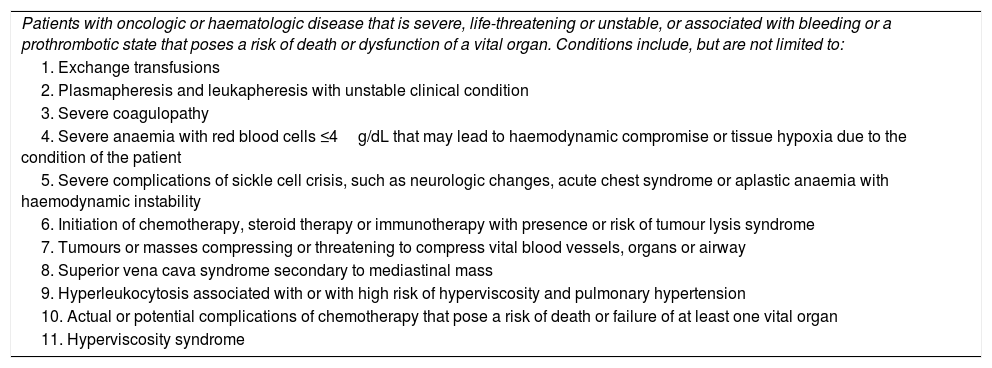
Criteria for PICU admission in haematology/oncology patients.
| Patients with oncologic or haematologic disease that is severe, life-threatening or unstable, or associated with bleeding or a prothrombotic state that poses a risk of death or dysfunction of a vital organ. Conditions include, but are not limited to: |
| 1. Exchange transfusions |
| 2. Plasmapheresis and leukapheresis with unstable clinical condition |
| 3. Severe coagulopathy |
| 4. Severe anaemia with red blood cells ≤4g/dL that may lead to haemodynamic compromise or tissue hypoxia due to the condition of the patient |
| 5. Severe complications of sickle cell crisis, such as neurologic changes, acute chest syndrome or aplastic anaemia with haemodynamic instability |
| 6. Initiation of chemotherapy, steroid therapy or immunotherapy with presence or risk of tumour lysis syndrome |
| 7. Tumours or masses compressing or threatening to compress vital blood vessels, organs or airway |
| 8. Superior vena cava syndrome secondary to mediastinal mass |
| 9. Hyperleukocytosis associated with or with high risk of hyperviscosity and pulmonary hypertension |
| 10. Actual or potential complications of chemotherapy that pose a risk of death or failure of at least one vital organ |
| 11. Hyperviscosity syndrome |
PICU, paediatric intensive care unit.
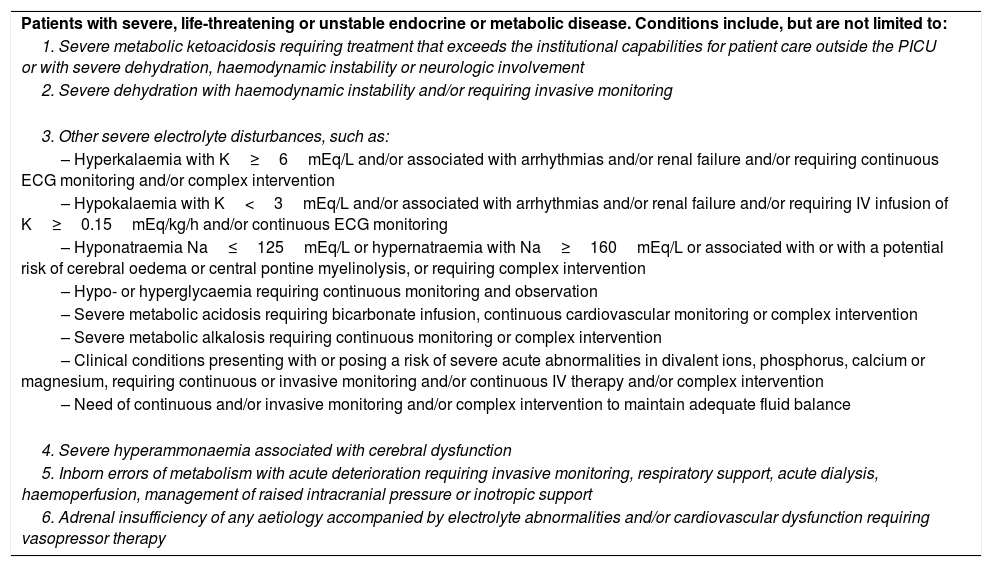
Criteria for PICU admission related to endocrine or metabolic conditions.
| Patients with severe, life-threatening or unstable endocrine or metabolic disease. Conditions include, but are not limited to: |
| 1. Severe metabolic ketoacidosis requiring treatment that exceeds the institutional capabilities for patient care outside the PICU or with severe dehydration, haemodynamic instability or neurologic involvement |
| 2. Severe dehydration with haemodynamic instability and/or requiring invasive monitoring |
| 3. Other severe electrolyte disturbances, such as: |
| – Hyperkalaemia with K≥6mEq/L and/or associated with arrhythmias and/or renal failure and/or requiring continuous ECG monitoring and/or complex intervention |
| – Hypokalaemia with K<3mEq/L and/or associated with arrhythmias and/or renal failure and/or requiring IV infusion of K≥0.15mEq/kg/h and/or continuous ECG monitoring |
| – Hyponatraemia Na≤125mEq/L or hypernatraemia with Na≥160mEq/L or associated with or with a potential risk of cerebral oedema or central pontine myelinolysis, or requiring complex intervention |
| – Hypo- or hyperglycaemia requiring continuous monitoring and observation |
| – Severe metabolic acidosis requiring bicarbonate infusion, continuous cardiovascular monitoring or complex intervention |
| – Severe metabolic alkalosis requiring continuous monitoring or complex intervention |
| – Clinical conditions presenting with or posing a risk of severe acute abnormalities in divalent ions, phosphorus, calcium or magnesium, requiring continuous or invasive monitoring and/or continuous IV therapy and/or complex intervention |
| – Need of continuous and/or invasive monitoring and/or complex intervention to maintain adequate fluid balance |
| 4. Severe hyperammonaemia associated with cerebral dysfunction |
| 5. Inborn errors of metabolism with acute deterioration requiring invasive monitoring, respiratory support, acute dialysis, haemoperfusion, management of raised intracranial pressure or inotropic support |
| 6. Adrenal insufficiency of any aetiology accompanied by electrolyte abnormalities and/or cardiovascular dysfunction requiring vasopressor therapy |
ECG, electrocardiogram; IV, intravenous; Na, sodium; K, potassium; PICU, paediatric intensive care unit.
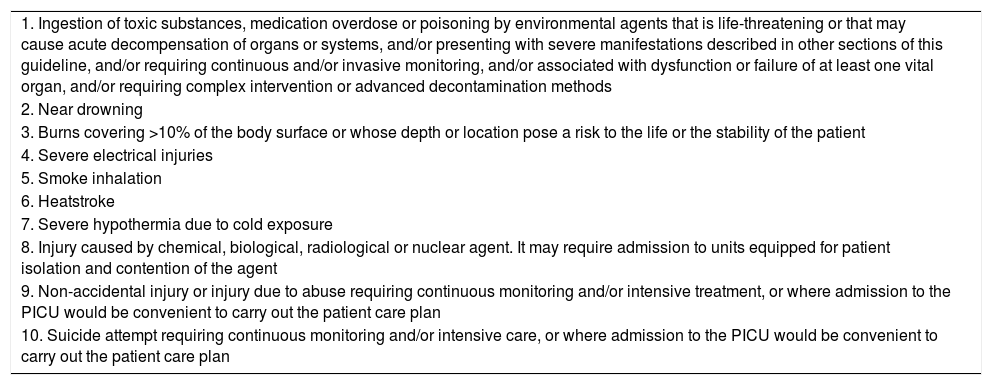
Criteria for PICU admission related to accidental injuries, poisoning and environmental injuries.
| 1. Ingestion of toxic substances, medication overdose or poisoning by environmental agents that is life-threatening or that may cause acute decompensation of organs or systems, and/or presenting with severe manifestations described in other sections of this guideline, and/or requiring continuous and/or invasive monitoring, and/or associated with dysfunction or failure of at least one vital organ, and/or requiring complex intervention or advanced decontamination methods |
| 2. Near drowning |
| 3. Burns covering >10% of the body surface or whose depth or location pose a risk to the life or the stability of the patient |
| 4. Severe electrical injuries |
| 5. Smoke inhalation |
| 6. Heatstroke |
| 7. Severe hypothermia due to cold exposure |
| 8. Injury caused by chemical, biological, radiological or nuclear agent. It may require admission to units equipped for patient isolation and contention of the agent |
| 9. Non-accidental injury or injury due to abuse requiring continuous monitoring and/or intensive treatment, or where admission to the PICU would be convenient to carry out the patient care plan |
| 10. Suicide attempt requiring continuous monitoring and/or intensive care, or where admission to the PICU would be convenient to carry out the patient care plan |
PICU, paediatric intensive care unit.
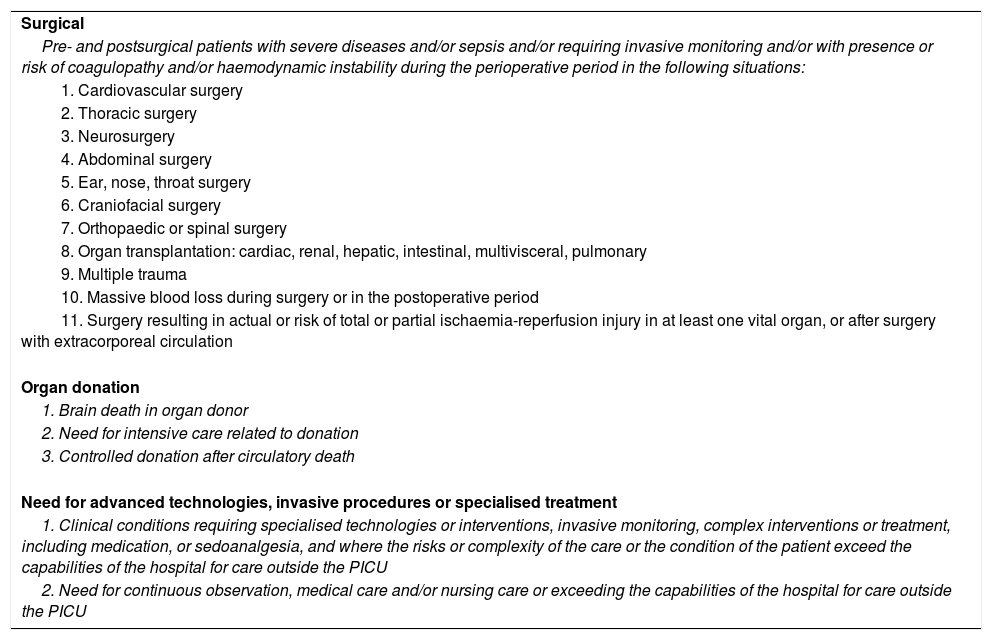
Criteria for PICU admission related to surgery, organ donation and invasive procedures or specialised treatments.
| Surgical |
| Pre- and postsurgical patients with severe diseases and/or sepsis and/or requiring invasive monitoring and/or with presence or risk of coagulopathy and/or haemodynamic instability during the perioperative period in the following situations: |
| 1. Cardiovascular surgery |
| 2. Thoracic surgery |
| 3. Neurosurgery |
| 4. Abdominal surgery |
| 5. Ear, nose, throat surgery |
| 6. Craniofacial surgery |
| 7. Orthopaedic or spinal surgery |
| 8. Organ transplantation: cardiac, renal, hepatic, intestinal, multivisceral, pulmonary |
| 9. Multiple trauma |
| 10. Massive blood loss during surgery or in the postoperative period |
| 11. Surgery resulting in actual or risk of total or partial ischaemia-reperfusion injury in at least one vital organ, or after surgery with extracorporeal circulation |
| Organ donation |
| 1. Brain death in organ donor |
| 2. Need for intensive care related to donation |
| 3. Controlled donation after circulatory death |
| Need for advanced technologies, invasive procedures or specialised treatment |
| 1. Clinical conditions requiring specialised technologies or interventions, invasive monitoring, complex interventions or treatment, including medication, or sedoanalgesia, and where the risks or complexity of the care or the condition of the patient exceed the capabilities of the hospital for care outside the PICU |
| 2. Need for continuous observation, medical care and/or nursing care or exceeding the capabilities of the hospital for care outside the PICU |
PICU, paediatric intensive care unit.
Patients with severe, life-threatening or unstable multiple organ or system disease. Conditions include, but are not limited to:
- 1.
Multiple organ dysfunction syndrome or failure, regardless of aetiology.
- 2.
Thrombocytopenia associated with multiple organ failure.
- 3.
Severe systemic inflammatory states, such as macrophage activation syndrome or haemophagocytic lymphohistiocytosis associated with shock, coagulopathy or vital organ dysfunction, or requiring intensive treatment and/or invasive and/or continuous monitoring.
- 4.
Post-transplantation lymphoproliferative disease associated with shock, coagulopathy or vital organ dysfunction, or requiring intensive treatment and/or intensive and/or continuous monitoring.
- 5.
Need of immunotherapy that may cause severe cytokine release syndrome.
- 6.
Suspected or documented malignant hyperthermia.
- 7.
Change in body temperature associated with a risk of arrhythmia and/or requiring invasive and/or continuous monitoring and/or complex intervention.
- 8.
Suspected or documented tissue hypoxia, systemic or in at least one vital organ.
- 9.
Intra-abdominal hypertension and abdominal compartment syndrome.
- 10.
Severe toxin-related diseases: toxic shock syndrome, malignant pertussis, tetanus, human botulism, diphtheria.
Patients staying in the PICU will be assessed and considered for discharge when the disease, process or unstable physiological condition that led to their admission has resolved and the patient no longer requires invasive or continuous monitoring or complex interventions exceeding the care capabilities outside the PICU, or when they are no longer benefitting from intensive care.
Patient discharge must be based on the following criteria:
- 1.
Stable haemodynamic parameters.
- 2.
Stable respiratory status in extubated patient with airway patency not requiring respiratory support or requiring non-invasive support that can be provided safely outside the PICU.
- 3.
Minimal oxygen requirements.
- 4.
The patient no longer requires inotropic support, vasodilators and antiarrhythmic drugs or otherwise requires them at low doses that can be safely administered outside the PICU.
- 5.
Cardiac dysrhythmias are controlled.
- 6.
Intracranial pressure monitoring equipment has been removed.
- 7.
The patient is neurologically stable with control of seizures.
- 8.
All haemodynamic monitoring catheters have been removed.
- 9.
Chronically mechanically ventilated patients with invasive (tracheostomy) or non-invasive ventilation that remain stable and whose critical illness has been resolved or reversed and can be transferred to a unit that routinely manages chronically ventilated patients or to home.
- 10.
Patients with routine peritoneal dialysis or haemodialysis with resolution of acute critical illness and who no longer require complex interventions, care or monitoring exceeding the care capabilities outside the PICU.
- 11.
Patients with tracheostomies that no longer require frequent and intensive suctioning.
- 12.
The health care team in charge of the patient and the patient's family, after a careful, joint and coordinated assessment, determine that there is no benefit in keeping the child in the PICU.
Paediatric intensive care is costly and there is a limited number of beds. When there are insufficient beds for severely ill patients that need them, refusal rates can be high and raise ethical dilemmas or lead to potential legal repercussions.13
Triage is essential in the PICU to ensure the optimal and equitable use of resources and to guarantee the safety and early treatment of critical patients in situations where resources become scarce, such as epidemics or natural disasters.8,13 Not admitting patients who are likely to benefit from the PICU, or undertriage, can increase their risk of death or progressive deterioration and multiple organ failure. Admitting patients who are unlikely to benefit from intensive care, or overtriage, may lead to more invasive and potentially harmful interventions as well as inappropriate allocation of resources, diverting care from other patients that need it more.32
Triage in PICUs must take into account the following key aspects13:
- -
Triage requires careful weighing of the multiple benefits and risks involved in PICU admission.
- -
Final triage decisions regarding admission to the PICU must be made by paediatric intensivists with input from nurses, paediatric emergency medicine specialists and hospitalists, surgeons, and allied professionals.
- -
Triage algorithms and protocols can be useful but can never supplant the role of skilled paediatric intensivists basing their decisions on input from multidisciplinary teams.
- -
Infrastructures need to be organised efficiently both within individual hospitals and at the regional level.
The opportune (timely and appropriate) delivery of intensive care to critically ill patients is associated with decreases in mortality, length of stay and health care costs.11,12 Thus, we recommend for each PICU to develop specific policies with explicit criteria regarding admission, discharge and triage tailored to the needs of the patients served in the corresponding hospital and its catchment area. These criteria should be adapted in response to current scientific evidence taking into account ethical and legal aspects. The staff of medical and surgical departments and units serving paediatric patients must be aware of the policies regarding PICU admission and know how to recognise the warning signs of acute and severe deterioration in children and adolescents with high-risk diseases, as do the family members that care for these patients.9 Furthermore, a paediatric rapid response systems (PRRS) or paediatric critical care outreach teams (CCOT) supported by a team of paediatric intensive care consultants can be established to assist paediatric inpatient care or surgical teams in the assessment and management of severely ill patients, facilitate the transition of patients into and out of the PICU, allow the early identification of patients that may benefit from admission and intensive care, prevent unnecessary PICU admission, reduce the rate of unexpected readmission to the PICU and reduce inpatient mortality.33–35
Whenever a patient meets any of the admission criteria specified in these guidelines, the physician in charge of the patient should consult with the PICU team or the paediatric intensivist that serves as a consultant for the PRRS or CCOT to plan the handover to the PICU.36 Paediatric intensivists should be informed of potential PICU admissions at an early stage, as initial intensive treatment may differ significantly from standard treatment.
In order to guarantee patient safety and the quality, timeliness, appropriateness and efficiency of paediatric intensive care, adherence to criteria for PICU admission, discharge and triage should be monitored and assessed periodically by a multidisciplinary team with use of quality indicators37 (including the standardised mortality rate, the severity-adjusted length of stay, and an analysis of unexpected readmissions)38 and with documentation and analysis of patient deaths, cases of cardiopulmonary arrest or shock outside the PICU, cases of denial of admission to the PICU or delayed PICU admission or discharge, cancellation of scheduled surgeries and triage decisions.
Conflicts of interestThe authors have no conflicts of interest to declare
These guidelines have been developed by:
The Asociación Española de Pediatría (Spanish Association of Paediatrics [AEP]). Paediatric Intensive Care Standards Committee:
- -
Pedro de la Oliva. Specialist in Paediatrics. Accredited for practice of Paediatric Critical Care. Doctor in Medicine. Chief of the Paediatric Intensive Care Unit, Hospital Universitario Infantil La Paz, Madrid. Associate Professor, Department of Paediatrics, School of Medicine, Universidad Autónoma de Madrid. Member of the Executive Board of the AEP in representation of the Sociedad Española de Cuidados Intensivos Pediátricos (Spanish Society of Paediatric Intensive Care [SECIP]).
- -
Corsino Rey-Galán. Specialist in Paediatrics. Accredited for practice of Paediatric Critical Care. Doctor in Medicine. Chief of the Paediatric Intensive Care Unit, Hospital Universitario Central de Asturias. Chair of the Department of Paediatrics, Universidad de Oviedo. Member of the Executive Board of the AEP in the position of President of the Sociedad de Pediatría de Asturias, Cantabria y Castilla y León (Paediatrics Society of Asturias, Cantabria and Castilla y León).
- -
Juan Carlos de Carlos-Vicente. Specialist in Paediatrics. Accredited for practice of Paediatric Critical Care. Chief of the Paediatric Intensive Care Unit, Hospital Universitario Son Espases, Palma de Mallorca. Member of the Executive Board of the AEP in the position of President of the Sociedad de Pediatría Balear (Paediatrics Society of Balearic Islands).
- -
Francisco Javier Pilar-Orive. Specialist in Paediatrics. Accredited for practice of Paediatric Critical Care. Chief of the Paediatric Intensive Care Unit, Hospital Universitario de Cruces, Bizkaia.
- -
Antonio Rodríguez-Núñez. Specialist in Paediatrics. Accredited for practice of Paediatric Critical Care. Doctor in Medicine. Adjunct physician in the Paediatric Intensive Care and Emergency Department of the Hospital Clínico Universitario, Santiago de Compostela. Chair of the Department of Psychiatry, Radiology, Public Health, Nursing and Medicine, Universidad de Santiago de Compostela. Member of the National Committee on the Specialty of Paediatrics and its Specific Subspecialties.
Sociedad Española de Cuidados Intensivos Pediátricos (Spanish Society of Paediatric Intensive Care [SECIP]). Paediatric Intensive Care Standards Committee:
- -
Francisco José Cambra-Lasaosa. Specialist in Paediatrics. Accredited for practice of Paediatric Critical Care. Doctor in Medicine. Chief of the Paediatric Intensive Care Unit, Hospital Sant Joan de Déu, Barcelona. Associate professor, Universidad de Barcelona. President of the SECIP.
- -
Juan Ignacio Sánchez-Díaz. Specialist in Paediatrics. Accredited for practice of Paediatric Critical Care. Doctor in Medicine. Chief of the Jefe de la Paediatric Intensive Care and Emergency Department of the Hospital Universitario 12 de Octubre, Madrid. Associate professor, Department of Paediatrics, School of Medicine, Universidad Complutense de Madrid.
- -
Ramón Hernández-Rastrollo. Specialist in Paediatrics. Accredited for practice of Paediatric Critical Care. Doctor in Medicine. Chief of the Paediatric Intensive Care Unit of the Hospital Universitario Materno-Infantil, Badajoz. Associate professor of Paediatrics, Department of Biomedical Sciences, School of Medicine, Universidad de Extremadura. Member of the Executive Board of the SECIP.
- -
Esther Ocete-Hita. Specialist in Paediatrics. Accredited for practice of Paediatric Critical Care. Doctor in Medicine. Specialty physician, Paediatric Intensive Care unit, Hospital Virgen de Las Nieves, Granada. Associate professor of Paediatrics, Universidad de Granada. Secretary of the SECIP.
- -
Ana Serrano-González. Specialist in Paediatrics. Accredited for practice of Paediatric Critical Care. Doctor in Medicine. Chief of the Paediatric Intensive Care Unit, Hospital Niño Jesús, Madrid. Associate professor, Department of Paediatrics, School of Medicine, Universidad Autónoma de Madrid.
Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias (Spanish Society of Intensive and Critical Care Medicine and Coronary Units [SEMICYUC]). Paediatric Intensive Care Standards Committee:
- -
Manuel Quintana-Díaz. Specialist in Paediatrics. Doctor in Medicine. Specialist physician, medical staff of the Department of Intensive Care, Hospital Universitario La Paz-Carlos III, Madrid. Associate professor of Health Sciences, Universidad Autónoma de Madrid. Secretary of the SEMICYUC.
- -
María Cruz Martín-Delgado. Specialist in Intensive Care Medicine. Doctor in Medicine. Chief of the Department of Intensive Care, Hospital Universitario de Torrejón. Associate professor, Universidad Francisco de Vitoria. President of the SEMICYUC.
- -
María Soledad Holanda-Peña. Specialist in Intensive Care Medicine. Doctor in Medicine. Coordinator of the Mother's and Children's Intensive Care Unit, Hospital Universitario Marqués de Valdecilla, Santander.
- -
Lluis Blanch. Specialist in Intensive Care Medicine. Doctor in Medicine. Critical Care Centre, Corporació Sanitaria Parc Taulí, Sabadell. Biomedical Research Networking Centre consortium (CIBER) on Respiratory Diseases, Instituto de Salud Carlos III, Madrid. Instituto de Investigación e Innovación Parc Taulí, Sabadell. Former President of the SEMICYUC.
Please cite this article as: de la Oliva P, Cambra-Lasaosa FJ, Quintana-Díaz M, Rey-Galán C, Sánchez-Díaz JI, Martín-Delgado MC, et al. Guias de ingreso, alta y triage para las unidades de cuidados intensivos pediátricos en España. Med Intensiva. 2018;42:235–246.
This article has also been published in the journal Anales de Pediatria, 2017. https://doi.org/10.1016/j.anpedi.2017.10.008