A study is made of the influence of alcohol and/or drug abuse upon recurrence of trauma, with an analysis of the influence of such abuse upon the time to appearance of first injury in patients without antecedents of trauma.
DesignA prospective observational study was made.
SettingTrauma patients admitted to the Intensive Care Unit (ICU) of a University Hospital.
PatientsTrauma patients admitted to the ICU.
InterventionNone.
Main measurementsTrauma recurrence was defined by a history of previous trauma requiring medical care. The presence of alcohol and other drugs of abuse were determined upon admission after severe trauma.
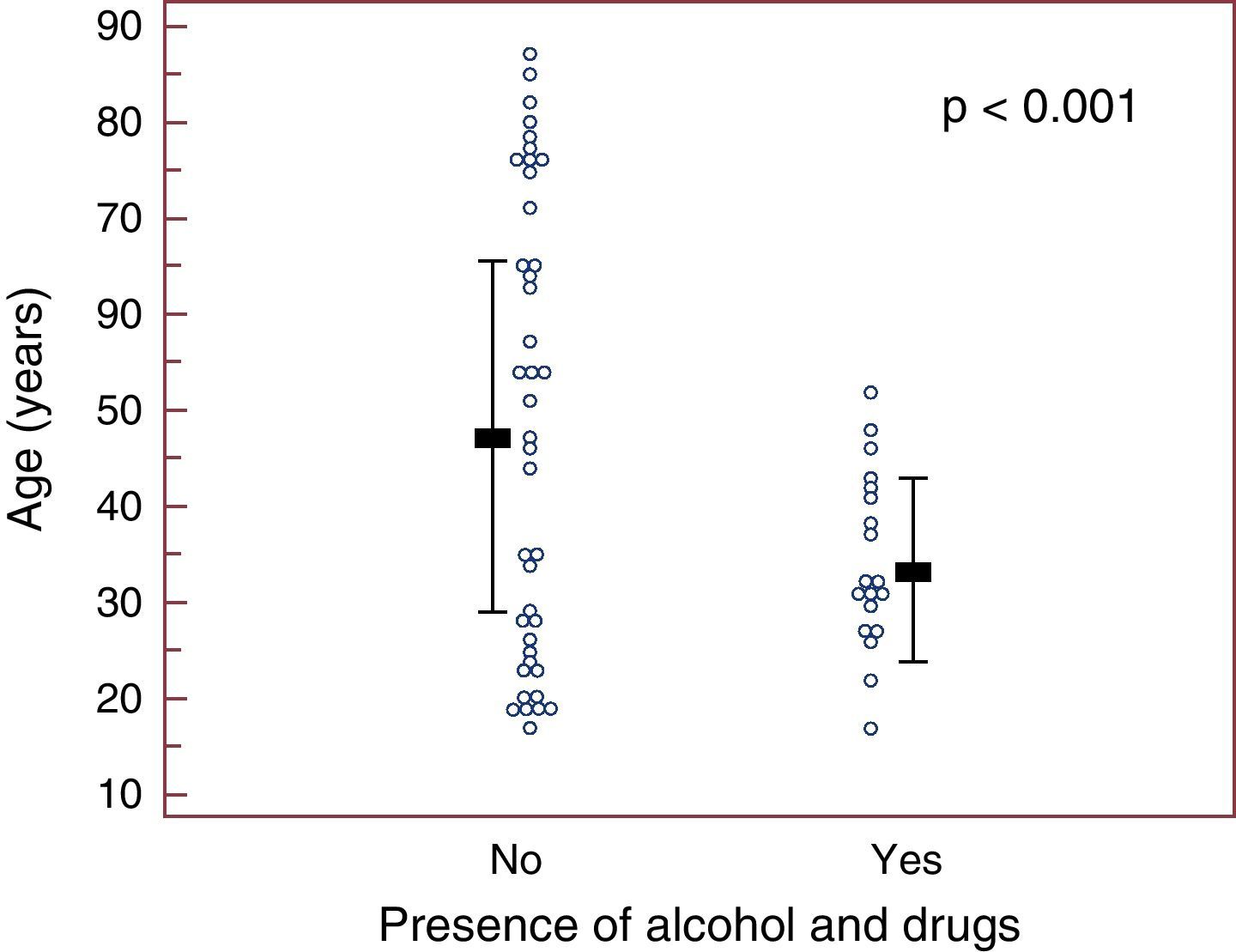
ResultsOut of the 166 trauma patients admitted to the ICU during the study period, 102 (87 males) were included in the study. Some substance was detected in 51 patients (50%), most frequently in the males (48/87, p<0.02). The most frequently detected substance was alcohol (39%), followed by cannabis (12%) and cocaine (7%), while more than one substance was found in 10 patients (9.8%). Of the 102 patients, 42 were recurrent trauma cases, and 32 (76%) of them were substance-positive, while only 10 were substance-negative (p<0.001). Of the 60 patients without antecedents of trauma, 19 (32%) were substance-positive, and these were significantly younger (34.3±9 years) than the 41 subjects who were substance-negative (48±23 years) (p<0.001).
ConclusionAlcohol and/or drug abuse increases the likelihood of recurrent trauma and may shorten the mean trauma-free period among patients without a history of trauma by almost 15 years.
Nuestro objetivo ha sido determinar la influencia del consumo de alcohol y/o drogas en la reincidencia de pacientes traumatizados y, en pacientes no reincidentes, analizar el papel de estas sustancias en el tiempo de aparición del primer episodio de traumatismo.
DiseñoEstudio observacional prospectivo.
ÁmbitoUnidad de cuidados intensivos (UCI) de un hospital terciario.
PacientesPacientes traumatizados ingresados en UCI.
IntervenciónNinguna.
Variables principalesLa reincidencia en el traumatismo se definió por antecedentes de traumatismo previo que requiriera atención médica. Se ha determinado la presencia de alcohol y otras drogas de abuso al ingreso tras un traumatismo grave.
ResultadosDe los 166 pacientes con traumatismo ingresados en la UCI durante el período de estudio, se incluyeron 102 (87 hombres). Se detectó alguna sustancia en 51 pacientes (50%), alcohol (39%), cannabis (12%) y cocaína (7%). De los 102 pacientes, 42 eran reincidentes, de los cuales 32 (76%) dieron positivo a alguna sustancia y solo en 10 se obtuvieron resultados negativos (p<0,001). De los 60 pacientes no reincidentes, 19 (32%) dieron resultados positivos a alguna sustancia, estos últimos eran significativamente más jóvenes (34,3±9 años) que los 41 con resultados negativos (48±23 años) (p<0,001).
ConclusiónEl consumo de alcohol y/o drogas aumenta la probabilidad de reincidencia en el traumatismo y adelanta en casi 15 años la presentación del primer traumatismo.
Situations of alcohol and drug abuse are known risk factors for traumatisms1–4 and for the repetition or recurrence of trauma.5–8 Such recurrence is of great concern and has important social and healthcare consequences. The available data referred to the incidence of trauma recurrence vary greatly from 0.38%6 to almost 90%.7 There may be a number of explanations for this great variability, including differences in study design and in the type of population evaluated. The highest recurrence rates are observed among assault victims (knife attacks, firearms, etc.) and patients subjected to treatment due to psychotropic substance abuse.7,8 In a prospective cohort study of the general population involving a mean follow-up period of 28 months, Rivara et al.5 recorded a recurrence of 1.3 cases per 1000 patients. In this context, patients with trauma related to alcohol abuse at first admission were seen to have a 2.5-fold greater risk of suffering trauma recurrence. The authors recommended the identification of these patients with a view to adopting strategies designed to avoid recurrence. In a posterior study, this same group found a brief motivational intervention to significantly decrease trauma recurrence among these individuals.9
Since injury can occur at a distance from the place of residence of the patient, a prospective analysis of trauma recurrence requires the availability of national registries, or at least of regional registries of trauma cases, in order to detect hospital admissions outside the area of residence. Many countries, including Spain, lack such registries–a situation that complicates correct evaluation of the recurrence rates. On the other hand, recurrence can also be evaluated on the basis of antecedents of previous traumatisms.
The present study was designed to determine the percentage of trauma patients who can be regarded as recurrent cases on the basis of their history of trauma, and to analyze the correlation to alcohol or drug abuse at the time of injury. On the other hand, an evaluation has been made of whether such substance abuse among the “non-recurrent” cases conditions the time to first injury.
Materials and methodsA prospective observational study was made of all trauma patients admitted to our Intensive Care Unit (ICU) between September 2008 and May 2009, and between October 2009 and January 2010. The study was approved by the Clinical Research Ethics Committee of our center. Given the design of the study, no informed consent was required.
Trauma recurrence was defined as the existence of antecedents of previous traumatism. Mild cases were regarded as those requiring medical care but no admission to hospital, while serious cases were regarded as those requiring hospitalization. The pertinent information was collected from the hospital records and by interviewing the patient (or a close relative in those cases where direct patient questioning was not possible). We also recorded data on antecedents of psychiatric treatment or psychoactive drug prescription.
Data were collected on a prospective basis referred to patient age, gender, Injury Severity Score (ISS) and the type of accident (vehicles, pedestrians, falls, etc.), among other variables. Upon admission to the ICU, measurements were made of blood alcohol levels via gas chromatography, and the risk of alcoholism was assessed using the Alcohol Use Disorders Identification (AUDIT),10 comprising interviews of the patient or close relatives. The patients were regarded as positive for alcohol abuse in the case of blood alcohol concentration > 0.3g/l, or when the AUDIT score revealed a moderate/high risk of alcoholism. The AUDIT test is generally used as an alternative for the identification of alcohol abuse in determining the relationship between alcohol and traumatism.9 A urine fluorescence immunoassay (Triage®) was used to detect the presence of cannabis, cocaine, amphetamines, methadone, benzodiazepines and opiates. Positive results for opiates and benzodiazepines were not taken into account, since these drugs are frequently administered to serious trauma victims in the out-hospital emergency care setting, and are therefore present in practically all the patients.
The exclusion criteria were: (a) impossibility of confirming the history of trauma for any reason (lack of patient cooperation, absence of members of the family, or language problems), and (b) non-availability of data referred to the presence of alcohol or drugs at current admission.
Statistical analysisQualitative variables were reported as absolute and relative (%) frequencies, while quantitative variables were expressed as the mean±standard deviation (SD) in the event of a normal distribution as determined by the Kolmogorov–Smirnov test, and as the median and interquartile range in the presence of a non-uniform distribution. The chi-squared test was used for evaluating correlations between qualitative variables and the presence/absence of substances, while the Student t-test and Mann–Whitney U-test were used for comparing quantitative variables in the presence of a normal and non-normal distribution, respectively. The SPSS version 15.0 statistical package for MS Windows (SPSS, Chicago, IL, USA) was used throughout. Statistical significance was considered for p<0.05.
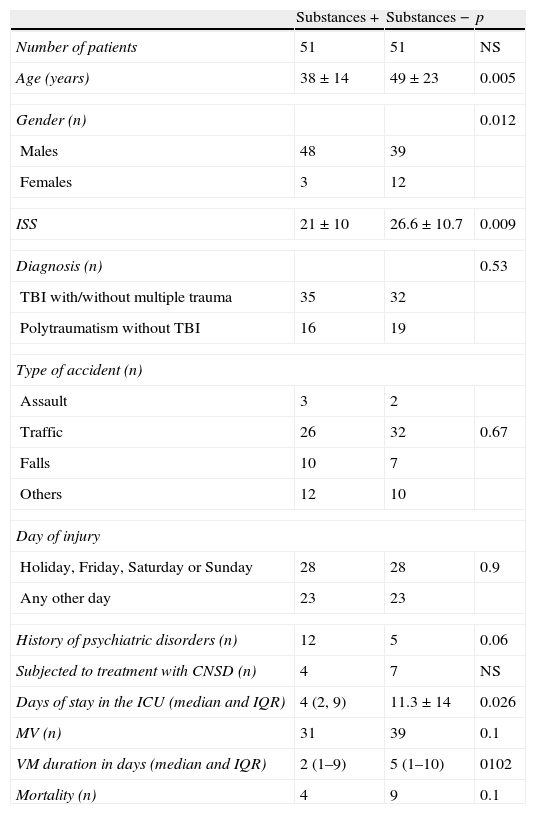
ResultsGlobal analysisOf the 166 trauma patients admitted during the two study intervals, analysis of blood alcohol and/or AUDIT scoring and urine testing were carried out in 102 subjects (87 males and 15 females). The remaining 64 patients were excluded from the study due to the following reasons: lack of sample availability due to admission of the patient from some other center several days after the accident (n=29), language difficulties (n=12), lack of collaboration on the part of the patient or relatives (n=12), or other reasons (n=11). Some of the study substances were detected in 51 of the 102 included patients (50%)–this proportion being significantly greater (p<0.02) in males (48/87; 55%) than in females (3/15; 20%) (Table 1). Eight patients admitted addiction to at least one of the study substances. The ISS score was significantly greater (p<0.009) in patients with negative results referred to the study substances (26.6±10.7) than in those with positive results (21±10). In turn, the duration of stay in the ICU was longer in patients with negative results than in those with positive test findings, with a median (interquartile range) of 82.11 days versus 42.9 days, respectively (p<0.026). No relationship was found between antecedents of previous trauma and the consumption of central nervous system (CNS) depressors or a history of psychiatric disorders (Table 1).
Data referred to the patients with positive and negative substance test results.
| Substances + | Substances − | p | |
| Number of patients | 51 | 51 | NS |
| Age (years) | 38±14 | 49±23 | 0.005 |
| Gender (n) | 0.012 | ||
| Males | 48 | 39 | |
| Females | 3 | 12 | |
| ISS | 21±10 | 26.6±10.7 | 0.009 |
| Diagnosis (n) | 0.53 | ||
| TBI with/without multiple trauma | 35 | 32 | |
| Polytraumatism without TBI | 16 | 19 | |
| Type of accident (n) | |||
| Assault | 3 | 2 | |
| Traffic | 26 | 32 | 0.67 |
| Falls | 10 | 7 | |
| Others | 12 | 10 | |
| Day of injury | |||
| Holiday, Friday, Saturday or Sunday | 28 | 28 | 0.9 |
| Any other day | 23 | 23 | |
| History of psychiatric disorders (n) | 12 | 5 | 0.06 |
| Subjected to treatment with CNSD (n) | 4 | 7 | NS |
| Days of stay in the ICU (median and IQR) | 4 (2, 9) | 11.3±14 | 0.026 |
| MV (n) | 31 | 39 | 0.1 |
| VM duration in days (median and IQR) | 2 (1–9) | 5 (1–10) | 0102 |
| Mortality (n) | 4 | 9 | 0.1 |
CNSD: central nervous system depressor; ISS: Injury Severity Score; TBI: traumatic brain injury; IQR: interquartile range; MV: mechanical ventilation.
Alcohol was the most frequently detected substance (39% of the cases), followed by cannabis (12%) and cocaine (7%). More than one substance was detected in 10 patients (9.8%). The mean blood alcohol concentration was 0.89g/l (range: 0.38–2.54g/l).
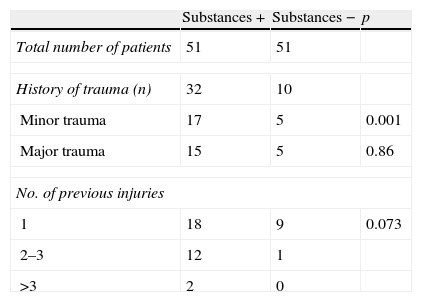
Analysis of recurrenceOf the 102 patients in the study sample, 42 had a history of previous trauma. Thirty-two of these recurrent cases (76%) proved positive for some of the study substances, and only 10 cases (24%) proved negative (p<0.001) (Table 2). There were no differences in the proportion of consumers/non-consumers according to the seriousness of previous injury (Table 2). Of the 60 patients without previous trauma, 41 proved negative (68%) and 19 were positive (32%). In this group of non-recurrent cases, the patients with positive test results were significantly younger (34.3±9 years) than the patients with negative results (48±23 years) (p<0.001) (Fig. 1).
This study confirms that trauma recurrence is closely related to alcohol and/or drug abuse. A novel finding has been the observation that the non-recurrent patients (i.e., those without antecedents of trauma) exposed to alcohol and/or drug abuse suffered their first injury almost 15 years earlier than those patients without substance abuse. In other words, the consumption of these substances reduces what we might call the “life period without accidents” by approximately 15 years.
The recorded percentage of patients with traumatisms related to alcohol and/or drug abuse was similar to that observed in previous studies.3,4,9 However, the figures of the present study are probably underestimated, since neither benzodiazepines nor opiates were taken into account, due to the reasons mentioned above (see Materials and methods). Likewise, some synthetic substances not included in the urine test kit obviously were not detected–a condition that may have further contributed to underestimate the incidence data.
Traumatisms are much more common in males; 87 of the patients in our series were men, and only 15 were women. Furthermore, a very important percentage of these males yielded positive substance test results (55%), versus only 20% of the females (p<0.012)–this reflecting the existence of gender differences in habits that deserve a more detailed investigation.
Over 70% of the patients with antecedents of trauma in the past showed a positive test result for some of the studied substances on occasion of the present injury episode. This proportion is similar to the values reported by Sims et al.8 and Kaufmann et al.,12 and reflects the extraordinary sociosanitary relevance of the problem. It likewise underscores the need for preventive strategies. In this context, the preventive measures presently regarded as most effective in preventing recurrence are secondary preventive actions in the form of a brief motivational intervention during hospital admission–allowing an almost 50% reduction in the trauma recurrence rate.9 This practice has been obligatory in the United States since 2007,13 but in Spain it is practically inexistent,14 and is often not regarded as a priority issue in the management of trauma patients.11,15
In our opinion, the implementation of secondary preventive programs referred to alcohol and drug abuse is urgently needed, particularly in hospital centers that treat trauma cases, with the collaboration of professionals from different disciplines (physicians, nurses, psychologists, etc.).16
Of the 51 patients that proved positive for some of the study drugs, only 8 admitted addiction to the detected substances, while the remaining 43 claimed to be only sporadic consumers. This proportion coincides with the values obtained in other series,9 and suggests that a good response to motivational intervention can be expected in such individuals. The efficacy of motivational intervention is likely to be greater in sporadic consumers without established addiction–hence the importance of identifying these individuals as candidates for enrollment in these programs. Patients with established addiction may require a different approach, such as rehabilitation therapy in a specialized center.
The relationship between the high incidence of traumatisms among young people and alcohol or drug abuse is well known,17 and several studies have reported that young individuals are more susceptible to the recurrence of trauma8,12 – though the magnitude of this effect has not been determined.18 An important and novel finding in our study has been the observation that alcohol and/or drug abuse shortens the “period without accidents” by almost 15 years, i.e., first injury is suffered by substance abusers nearly 15 years earlier than in the case of non-abusers. Fig. 1 shows the age of the non-recurrent individuals in relation to substance abuse on occasion of their first traumatism. To our knowledge, this is the first published quantification of the mentioned “period without accidents”, and may be of help in enhancing awareness of the sociosanitary impact of the phenomenon. It must be taken into account that younger patients are more susceptible to recurrence, since they have more years ahead to suffer a second injury compared with older adults. A surprising finding has been a significantly higher ISS score in the patients with negative test results for alcohol and drugs versus the patients with positive results. We have no definitive explanation for this observation, though in some cases the action of the studied substances upon patient level of consciousness may have favored admission to Intensive Care. The lesser seriousness of the injuries and the younger age of the patients with positive test results could explain their shorter stay in the ICU. Likewise, we found no greater incidence of trauma cases associated to alcohol and/or drug abuse on weekends and holidays. Such a relationship is observed particularly in the case of traffic accidents, and less so in other injuries (occupational, domestic, etc.) included in our study–a circumstance that may help explain these results.
The effect of alcohol upon post-trauma morbidity and mortality is subject to much controversy. Some authors consider the presence of alcohol to be a negative factor in relation to morbidity,19,20 with a reinforcing effect upon the injuries suffered by drivers.21 In contrast, Jurkovich et al.22 found chronic alcohol abuse but not acute abuse to exert a negative influence upon the outcome. According to other investigators, alcohol either has no effect or exerts a protective effect upon the outcome in patients with traumatism.23,24 On the other hand, alcohol consumption may have a neuroprotective effect in traumatic brain injury, and a therapeutic role has even been suggested24–though the results in this sense remain inconclusive.
The limitations of our study include the non-consideration of benzodiazepines and opiates, which may have caused us to underestimate the number of patients with positive substance test results. Moreover, this was a single-center study including severe trauma patients admitted to the ICU but without taking into account other patients seen in the emergency room but not admitted to the ICU. It is also possible that some patients may have omitted or hidden information in the interview, with imprecision in remembering past episodes, particularly in the case of older patients. However, in one half of the patients this information was obtained from the hospital records, with confirmation upon interviewing the patients or their relatives–thereby affording credibility to the results.
Although there is an undeniable epidemiological association between alcohol and/or drug abuse and the risk of traumatism, no unequivocal cause–effect relationship can be established from the data obtained in our study. Firstly, almost one-half of the patients with positive substance test results were not the driver in the case of traffic accidents, and secondly, the technique used for analyzing drug substances in urine offered qualitative, not quantitative results.
ConclusionAlcohol and/or drug abuse increases the risk of trauma recurrence and can shorten the average time without injuries among non-recurrent trauma patients by almost 15 years.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Cordovilla Guardia S, et al. El consumo de alcohol y/o drogas favorece la reincidencia en el traumatismo y reduce el período sin traumatismos. Med Intensiva. 2012;37:6–11.