To present the preliminary results of a non-heart beating donor (NHBD) program in a city of under 500,000 inhabitants.
DesignA prospective observational study was conducted between 2010 and 2011.
SettingVirgen de las Nieves Hospital and metropolitan area of Granada (Spain).
PopulationNHBD and brain dead donors (BDD) in the province of Granada during 2010 and 2011.
Study variablesCharacteristics of NHBD, out- and in-hospital times, family and legal refusals, preservation methods, and family information procedure. Organs: reasons for organ non-validness, and harvested and transplanted organs. Recipients: hemodialysis sessions and creatinine at discharge. BDD: number of real donors (RD) and of kidney transplants.
ResultsAmong the BDD there were 102 RD and 104 kidney transplants were carried out. In asystole, 22 potential donors, 21 eligible donors, 20 RD and 13 used donors were registered. The mean age among the RD was 50 years (range 33–62) (16 males and 4 females). Twenty-one kidney and two liver transplants from NHBD were performed. There were a number of reasons for organ non-validness. The mean number of post-transplantation hemodialysis sessions was 1.4 (range 0–6). The mean hospital stay was 25 days (range 14–41), and the mean creatinine concentration at discharge was 3.4mg/dl (range 1.5–6.4). There was one family rejection and no legal (court-ruled) rejections. The preservation methods and family information procedure are described.
ConclusionsThe preliminary results support the development of NHBD programs in cities with under 500,000 inhabitants. In 2011, NHBD accounted for 20.19% of the kidney transplants and 19.60% of the global organ donations in the province of Granada.
Presentar resultados iniciales de un programa de donación en asistolia (DA) en una ciudad de menos de 500.000 habitantes.
DiseñoEstudio observacional prospectivo durante 2010 y 2011.
ÁmbitoHospital Virgen de las Nieves y Área Metropolitana de Granada.
PoblaciónDA y donantes en muerte encefálica (DME) de la provincia de Granada en 2010 y 2011.
Variables de interésCaracterísticas de los DA, tiempos extrahospitalarios e intrahospitalarios, negativas familiares y judiciales, métodos de preservación, procedimiento de información a familiares. Órganos: causas de no validez, extraídos y transplantados. Receptores: sesiones de hemodiálisis y creatinina al alta. DME: número de donantes reales (DR) y de trasplantes renales.
ResultadosEn ME hubo 102 DR y se realizaron 104 trasplantes renales. Se han registrado en asistolia 22 donantes potenciales (DP), 21 donantes elegibles (DE), 20 DR y 13 donantes utilizados (DU). Edad media de los DR: 50 años (rango 33–62), 16 hombres y 4 mujeres. Se han realizado 21 trasplantes renales y 2 hepáticos de DA. Las causas de no validez son múltiples. Número medio de sesiones de hemodiálisis postrasplante: 1,4 (rango 0–6). Estancia hospitalaria media: 25 días (rango 14–41). Creatinina media al alta: 3,4mg/dL (rango 1,5–6,4). Ninguna negativa judicial y una negativa familiar. Se describen los métodos de preservación y el procedimiento de información a familiares.
ConclusionesLos resultados iniciales apoyan el desarrollo de programas de DA en ciudades de menos de 500.000 habitantes. La DA ha supuesto en 2011 el 20,19% de los trasplantes renales y el 19,6% de los donantes de órganos de la provincia de Granada.
In Spain, with a total population of 47.2 million inhabitants in 2011, there are 179 hospital centers authorized to detect, diagnose and maintain dead brain donors, and 43 hospital authorized to perform transplants. Up until 1 January 2012, a total of 51,909 kidney transplants have been performed in these centers, together with 19,399 liver transplants, 6528 heart transplants, 2709 lung transplants, 1342 pancreatic transplants and 89 intestinal transplants. Globally, 81,909 organ transplants have been performed in Spain.
In addition, the donor rate in Spain remains the highest in the world,1 with 35.3 donors per million of population (pmp), followed at a distance by the United States, with 25 donors pmp, and the European Union, with 18.4 donors pmp.
Despite all the efforts made in this country, there has been a tendency toward stabilization of transplantation activity in recent years.2 The number of donors is not enough to satisfy the transplant demands of the population. The number of patients on the transplant waiting list grows year by year, and 7–9% of them die before receiving a transplant. Likewise, a similar percentage of patients are excluded from the waiting list, often because of a worsening of their clinical condition.
In order to adapt to this situation, the Spanish National Transplant Organization (Organización Nacional de Trasplantes, ONT) has developed a National Strategic Plan for the improvement of organ donation and transplantation in Spain3: the Plan Donación 40. The aims of the plan are to increase organ availability, with the definition of five intervention areas: optimization of brain dead donors (BDD); increase in the utilization of organs from expanded criteria donors; the use of special surgical techniques; increased consideration of live kidney donors; and the encouragement of non-heart beating donation (NHBD). Although in the year 1995 only 3.3% of all donors in Spain were NHBD,4 by 2010 this percentage had increased to 8.7%.
The number of organs transplanted from NHBD is smaller than in the case of BDD. In kidney transplantation the results with NHBD are similar to those obtained with BDD, though with a greater incidence of delayed kidney function and primary non-functioning grafts.5,6 In the case of liver transplantation, only limited information is available on the results obtained with the use of livers from non-heart beating donors following unsuccessful cardiorespiratory arrest resuscitation measures.7–10 Lastly, lung transplantation from NHBD is still in an earlier phase of development.11–15
At present, only Spain and France have NHBD programs involving donors who die as a result of out-hospital cardiorespiratory arrest.16 Up until two years ago, this activity fundamentally took place in four hospitals: Complejo Hospitalario in A Coruña, Hospital Clínico San Carlos in Madrid, the Hospital Clínic in Barcelona, and Hospital Doce de Octubre in Madrid. The three centers with the greatest activity are all located in large cities (over 3,200,000 inhabitants in the case of Madrid and over 1,600,000 inhabitants in Barcelona, without counting their respective metropolitan areas). Organizational difficulties and the rapid response requirements explain why few hospitals apply this type of program.
Recently, two new programs, that of Hospital Universitario Virgen de las Nieves in Granada and that of Hospital de San Juan in Alicante, have started their NHBD activities involving donors who die as a result of out-hospital cardiorespiratory arrest.
The potential of the NHBD programs in Spain has not been fully established.5,17 The experience of Hospital Clínico San Carlos, with very strict screening criteria, shows that the current number of donors (real donor from which at least one organ has been transplanted) in the context of the NHBD program can be estimated as 15–16 donors pmp. The Hospital Clínic in Barcelona yields similar figures, in the order of 13 actual donors pmp. The data are practically all referred to NHBD in the context of out-hospital cardiorespiratory arrest.
The city of Granada has over 239,000 inhabitants, and if we include its metropolitan area the figure reaches over 516,000 inhabitants. According to expert opinion,17 this is the minimum population needed in order for an out-hospital NHBD program to be viable. With the above figures, 7–8 real donors could be expected a year in this population.
The present study describes the initial results of a NHBD program in a city of less than 500,000 inhabitants.
Materials and methodsInstead of the term “valid donor”, it is preferable to use the classification based on the phase of the donation process in which the individual with cessation of cardiorespiratory function happens to be. This classification recently has been published as a result of the Third Global Consultation of the World Health Organization (WHO): striving to achieve self-sufficiency in donation and transplantation18,19:
Possible donor: a patient with serious brain damage, or a patient with circulatory arrest and without apparent medical contraindications to organ donation.
Potential donor (PD):
- A.
Individuals in which the circulatory and respiratory functions have ceased and in which resuscitation maneuvers either will not be started or will not be continued.
- B.
Individuals in which the circulatory and respiratory functions are expected to cease within a time interval allowing organ harvesting for transplantation.
- •
Eligible donor (ED): An individual without medical contraindications to donation, with confirmed death secondary to irreversible cessation of circulatory and respiratory function, as specified by applicable legislation, and within a time interval allowing organ harvesting for transplantation.
- •
Real donor (RD): An eligible donor in which consent to donation has been obtained:
- A.
Subjected to incision with the purpose of harvesting organs for transplantation.
- B.
From which at least one organ has been harvested for transplantation.
Used donor (UD): A real donor from which at least one organ has been transplanted.
The activity of the NHBD program of Granada has been recorded from its start in January 2010 until December 2011.
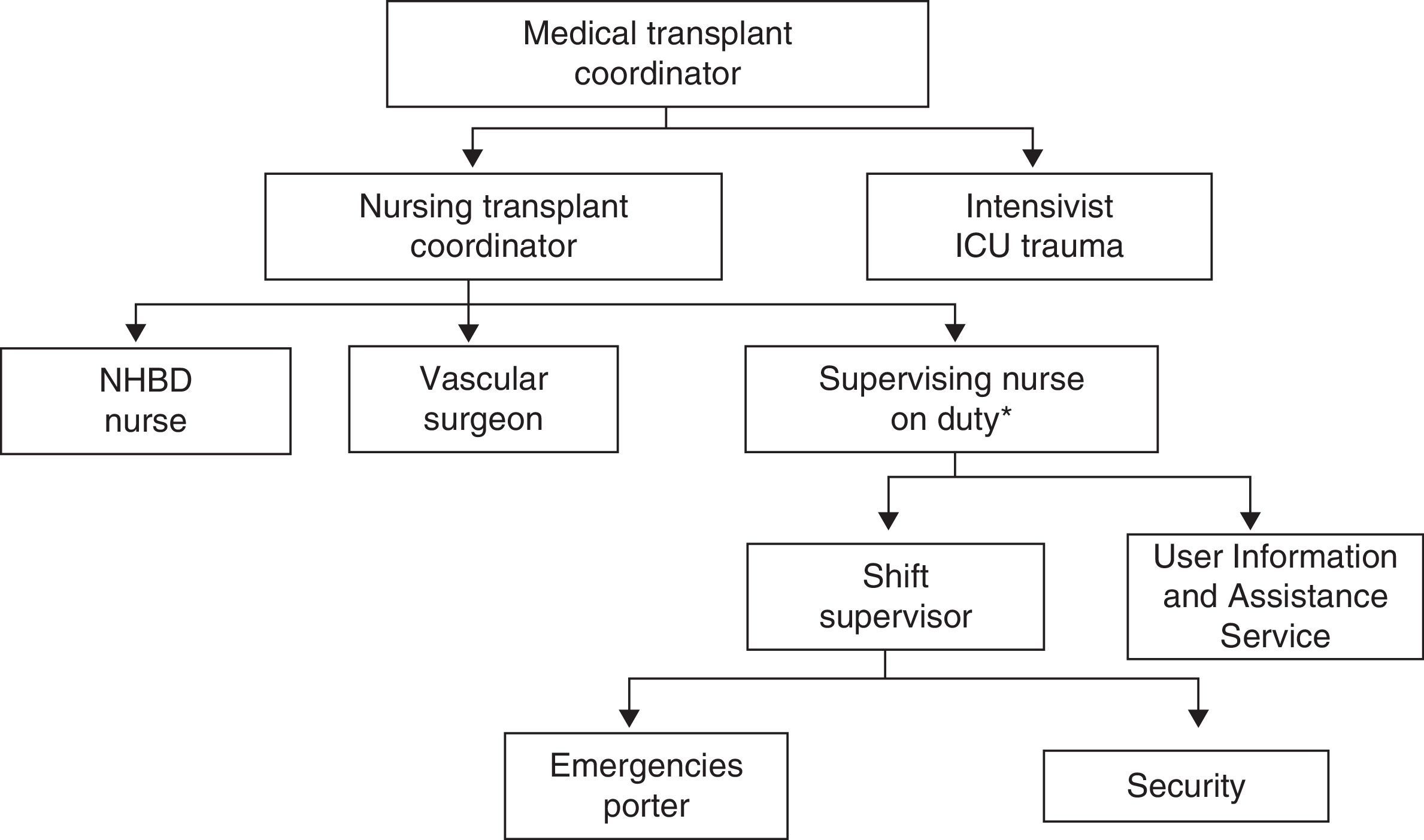
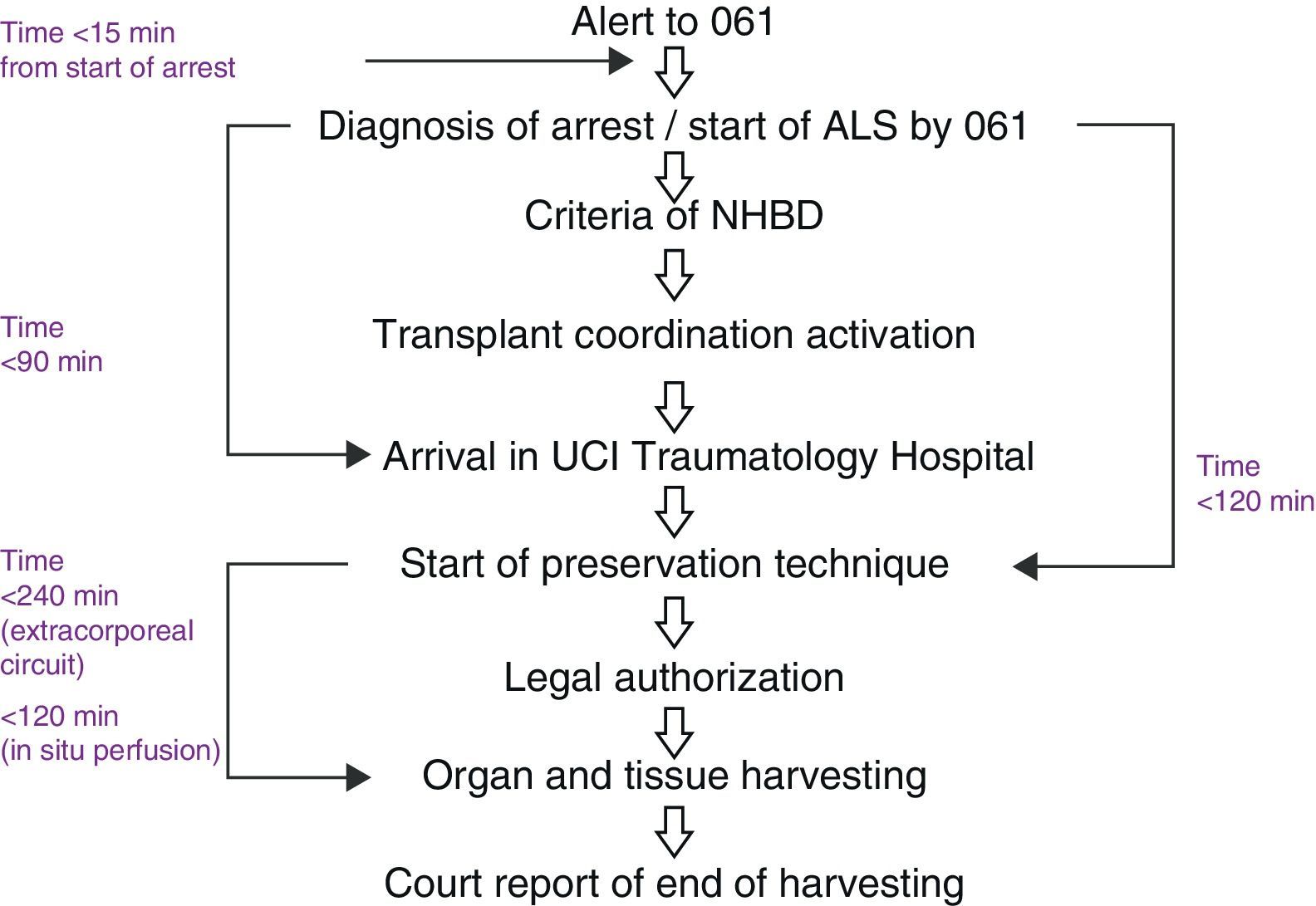
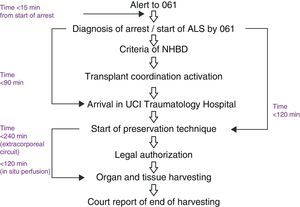
The process is activated from the call of the Out-Hospital Emergency Service 061 assisting a case of cardiorespiratory arrest without heart rhythm recovery after the appropriate period of advanced life support (ALS) maneuvering. This period, as well as the required maneuvers, is adjusted according to age and the circumstances of cardiorespiratory arrest. Less than 15min must have elapsed from the estimated time of arrest to the start of ALS maneuvering by the 061 Service. In Granada, this protocol is referred to as the “Alpha Code”, and comprises a progressive cascade-like activation of healthcare professionals that form part of a rapid response team, schematically represented in Fig. 1.
In this protocol, the PD is taken directly by the Out-Hospital Emergency Service 061 to the Intensive Care Unit (ICU) of Hospital Universitario Virgen de las Nieves. This ICU has two beds without healthcare personnel available in cases of emergencies. The PD is attended by located personnel that report to the unit for this concrete activity.
From the out-hospital logistics perspective, the out-hospital time is regarded as the time from the start of ALS by the Out-Hospital Emergency Service 061 to arrival in the ICU.
The following activities are carried out during the stay of the PD in the ICU: confirmation of cardiac death (according to Spanish Royal Decree 2070/1999), evidencing the absence of pulse and breathing for 5min; examination and evaluation of the PD; catheterization of the subclavian or right jugular vein for the collection of samples; the obtainment of chest X-rays; nasogastric and bladder catheterization; and the sending of a fax to obtain legal court authorization for starting the preservation maneuvers. The central vascular access allows us to obtain samples for blood tests without risking the complications associated with percutaneous vascular puncture in a donor to be subjected to anticoagulation, since the peripheral vascular access established by the 061 Service is not enough to obtain blood for study as a potential donor.
The Department of Laboratory Analyses and Microbiology provides results in under 120min. A microbiologist is on duty in the hospital.
Once cardiac death has been confirmed, after definitive acceptance as an eligible donor, and in the absence of a court ruling rejecting the procedure (or in the absence of a court reply within 15min after sending the request for permission by fax), the donor is heparinized and moved to the operating room. This period of time is under 30min. If no operating room is available in that moment, preservation maneuvering is started in the ICU. In this short period of time, the family of the donor generally has not reached the hospital; as a result, notification of the death, and posteriorly the request for consent to donation, are made with the ED in the operating room.
From the in-hospital logistics perspective, the following in-hospital times are considered: mean stay in the ICU until transfer to the operating room; mean time from arrival in the operating room to the start of the preservation techniques; and time from the start of the preservation techniques to completion of the donor biochemical and microbiological study and the obtainment of family consent and legal court authorization.
The screening criteria and time limits are shown in Table 1 and in Fig. 2.
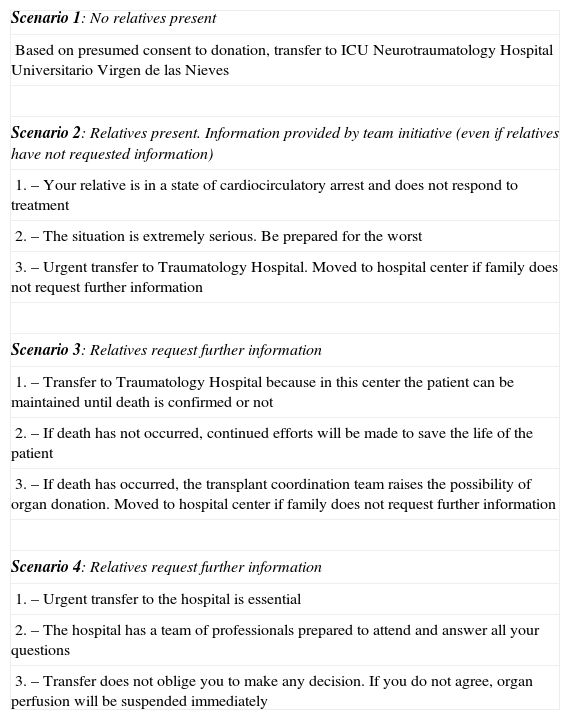
Out-hospital emergencies team protocol for informing relatives for non-beating heart donation.
| Scenario 1: No relatives present |
| Based on presumed consent to donation, transfer to ICU Neurotraumatology Hospital Universitario Virgen de las Nieves |
| Scenario 2: Relatives present. Information provided by team initiative (even if relatives have not requested information) |
| 1. – Your relative is in a state of cardiocirculatory arrest and does not respond to treatment |
| 2. – The situation is extremely serious. Be prepared for the worst |
| 3. – Urgent transfer to Traumatology Hospital. Moved to hospital center if family does not request further information |
| Scenario 3: Relatives request further information |
| 1. – Transfer to Traumatology Hospital because in this center the patient can be maintained until death is confirmed or not |
| 2. – If death has not occurred, continued efforts will be made to save the life of the patient |
| 3. – If death has occurred, the transplant coordination team raises the possibility of organ donation. Moved to hospital center if family does not request further information |
| Scenario 4: Relatives request further information |
| 1. – Urgent transfer to the hospital is essential |
| 2. – The hospital has a team of professionals prepared to attend and answer all your questions |
| 3. – Transfer does not oblige you to make any decision. If you do not agree, organ perfusion will be suspended immediately |
We have recorded the activity of this program during 24 months (from January 2010 to December 2011), including the number of PD, ED, RD and UD, the characteristics of the donors and transplanted organs and tissues, the out- and in-hospital times, preservation methods, and post-transplantation results, as well as family and court rejections.
ResultsA total of 22 PD were recorded from the start of the program in January 2010 until December 2011. Of these 22 PD, with transfer to the hospital, one recovered effective heart beat upon arrival in the ICU. As a result, post-resuscitation care was started, with hypothermia, emergency coronariography and the implantation of a stent in the anterior descending artery, though the patient finally died of cardiogenic shock. Thus, a total of 21 ED were moved to the operating room with the performance of preservation techniques. Family rejection of donation only occurred in one of these 21 cases; as a result, the study analysis includes the 20 remaining RD.
The donation acceptance rate was 96%, with only one rejection out of 21 interviews. There have been no negative court rulings since the start of the program.
Of the 21 ED, extracorporeal circulation under normothermal conditions was chosen as preservation technique in 13 cases (62%). In four cases (19%) cold renal perfusion was used as preservation technique. Lastly, in four cases (19%) conversion of the preservation technique was decided in the presence of problems of blood return to the extracorporeal circulation machine–switching from extracorporeal circulation under normothermal conditions to cold renal perfusion. This avoided the loss of 8 kidneys for transplantation (these organs would have been lost due to impossibility of preservation with extracorporeal circulation under normothermal conditions).
The mean age of these 20 RD was 50 years (range 33–62) (16 men and 4 women).
Of the 20 RD, 12 were UD and 8 were considered not valid. The causes of non-validness were diverse. One case had a medical contraindication due to positive testing for antibodies against hepatitis C virus (in all cases the laboratory response time was under 120min). Two donors were discarded during surgery: one because of severe arteriosclerosis, and the other due to the detection of cholangiocarcinoma. Other causes of non-validness were the identification of infrarenal aortic dissection in one subject and renal biopsy rejection in another. In addition, there were surgical technical problems with the impossibility of organ preservation in three cases.
The out-hospital time from the start of ALS by the Out-Hospital Emergency Service 061 to arrival in the ICU was 56min (range 35–75).
As regards the in-hospital times, the mean stay in the ICU until transfer to the operating room was 26min (range 15–50); the mean time from arrival in the operating room to the start of the preservation techniques was 27min (range 15–40); and an average of 118min (range 70–170) elapsed from the start of preservation to completion of the donor biochemical and microbiological study and the obtainment of family consent and legal court authorization.
Five renal transplants corresponding to 9 RD were performed in 2010, while 16 renal transplants corresponding to 11 RD were performed in 2011. Overall, 21 renal transplants were carried out, with a good course on the part of both the recipient and graft to date.
Two liver transplants were also performed in 2011: one operation presented acute rejection problems, though without the need for retransplantation to date, while the second liver graft resulted in recipient death due to cardiac arrest during reperfusion. The rest of the donors were discarded because of initial AST-ALT transaminase elevations >3–4 times the upper limit of normal and final AST-ALT elevations >4–5 times the upper limit of normal, or based on the macroscopic appearance of the organ as evaluated by the surgeon. The livers of 10 donors were evaluated, though only the two organs considered valid for transplantation were harvested.
The number of donors used and the number of organs produced per donor have gradually improved, the average being 1.15 valid organs per real donor. Sixty-two percent were moreover tissue donors.
The renal cold ischemia time was 11.5h (range 6–17). The course of the recipients and kidney grafts has been satisfactory: the mean number of post-transplantation hemodialysis sessions was 1.4 (range 0–6), with a mean hospital stay of 25 days (range 14–41), and a mean creatinine concentration at hospital discharge of 3.4mg/dl (range 1.5–6.4).
DiscussionThis study shows the viability of a non-heart beating donor (NHBD) program in a city of under 500,000 inhabitants, and raises the possibility of implementing programs of this kind in other cities of similar size.
The NHBD potential of cities with under 500,000 inhabitants has not been established. Up until barely three years ago, this activity was fundamentally centered on three hospitals in Spain: Hospital Clínico San Carlos in Madrid, the Hospital Clínic in Barcelona, and Hospital Doce de Octubre in Madrid. The initial idea that non-heart beating donation should be limited for reasons of effectiveness to areas with a minimum population of 500,000 inhabitants has come under questioning by the recent initiation of two new programs: one in Hospital de San Joan in Alicante and the other in Hospital Virgen de las Nieves in Granada–with initial results that are becoming consolidated.
Few publications have addressed the efficiency of donation processes.20 In addition, we have found no studies in the literature comparing the costs and benefits of non-heart beating donation. Nevertheless, the investment in terms of materials comprised the acquisition of an automatic cardiac compressor (11,000 euros) and an extracorporeal circulation system equipped with a centrifuge pump and heater (40,000 euros). The cost per donor in terms of expendables is approximately 900 euros (extracorporeal circulation under normothermal conditions) or 100 euros (exsanguination and renal perfusion in hypothermia). From the human resources perspective, both the nursing Transplant Coordination Team and nurses with training in asystolia, and the vascular surgeons, are supported by professionals from Hospital Universitario Virgen de las Nieves and Hospital Universitario San Cecilio.
The program has improved its yield and effectiveness both in terms of the number of PD (increasing from 9 donors in 2010 to 11 donors in 2011) and as regards the number of valid organs per donor (increasing from 0.7 valid organs per donor in 2010 to 1.28 valid organs per donor in 2011). During the study period, there were a total of 102 donors in Granada (brain death plus asystolia), and 104 renal transplants were performed (brain death plus asystolia, excluding live donor renal transplants). Thus, the NHBD program accounted for 19.6% of the donors and 20.19% of the dead donor renal transplants in the province, affording a high donors per million of population rate (44 donors pmp in 2010 versus 63 donors pmp in 2011). It should be mentioned that the initial technical problems with vascular cannulation have been resolved, as a result of which no organ donors were lost because of such problems in the course of 2011.
Regarding the preservation procedures, it is important to note that in this program we have developed a preservation strategy that uses two techniques:17 renal perfusion with preservation solution and hypothermia, and extracorporeal circulation femoro-femoral bypass with membrane oxygenation under normothermal conditions. The first technique (cold renal perfusion) is the method of choice when the donor is a multiple trauma victim, where anticoagulation and the probable visceral and/or vascular injuries can cause return problems if an extracorporeal circuit is used. The second scenario in which cold perfusion is used is when venous return fails in cases where extracorporeal circulation has been the first choice preservation technique.
This cold renal perfusion technique had already been successfully used in Andalusia in the 1990s21,22 by the team led by Dr. Miguel Ángel Frutos. It therefore was programmed as a rescue technique in cases of failed extracorporeal circulation.
For extracorporeal circulation femoro-femoral bypass with membrane oxygenation under normothermal conditions we use a protocol similar to that of Hospital Clínico San Carlos,17 though the program of Hospital Universitario Virgen de las Nieves applies the technique under normothermal conditions in order to allow the consideration of liver harvesting.
For renal perfusion with preservation solution and hypothermia we use a rapid roller infusion pump. In a first phase we administer 150ml/kg of Plasmalyte® at a rate of 500–600ml/min through a multiple perforated double balloon catheter positioned in the aorta (until clear liquid is seen to emerge from the draining catheter placed in the femoral vein). In a second phase we administer 75ml/kg of Wisconsin-type perfusion solution at a rate of 300ml/min and maintain continuous perfusion at a rate of 50ml/min until organ harvesting.
An important aspect has been the development of a specific protocol for informing the relatives of potential non-heart beating donors (Table 1). This protocol is used by the Out-Hospital Emergency Service 061 when the Alpha Code is activated. The procedure has been jointly developed by the professionals of the 061 Service and by the Transplant Coordination Team, with the aim of preserving all the values at stake, following a careful pondering process.23 The protocol includes four scenarios that are developed progressively, and strives to establish a balanced combination of the principles of autonomy, good will and fairness–together with other fundamental concepts referred to information rights, such as the right not to know, the avoidance of excessive harshness in informing (which may prove fatal), and tolerable truthfulness (i.e., informing gently, with diplomacy and caring).24 This protocol is continued when the relatives reach the hospital center and are attended by the User Information and Assistance Service (alerted by the supervising nurse on duty). The relatives are taken to the briefing room and receive a protocolized account of the following information: “Your relative is in extremely serious condition. The medical team will inform you as soon as possible”. At the time when the User Information and Assistance Service notifies the Transplant Coordination Team that the family has reached the hospital, a transplant coordinator visits them and informs them of the death of their relative.
The informative setting in all cases is regulated by Act 41/2002, referred to patient autonomy and the rights and obligations related to clinical documentation and information.25 This regulation specifies that the information is to be truthful, conveyed in a comprehensible manner adapted to the needs of the individual, and offering help in decision making with due respect for personal and free will.
The necessary organizational effort, implicating the Out-Hospital Emergency Service 061, in-hospital logistics, and the coordination of both, has been one of the main difficulties in the development of this program. The most relevant aspects of the in- and out-hospital logistics are detailed in the Appendix.
Each hospital, in consistency with its own circumstances, should develop its own NHBD program.26 The program of Hospital Universitario Virgen de las Nieves has a series of characteristics that can explain the results obtained. In effect, the transfer times from the place of cardiorespiratory arrest to the hospital are obviously shorter in a city of smaller size than Madrid or Barcelona, thereby allowing a reduction of the warm ischemia time. Potential non-heart beating donors are only regarded as those in which a unit of the 061 Service has applied ALS maneuvering without success, with evaluation as potential donors and transfer to the hospital–guaranteeing excellence in the initial management of cardiorespiratory arrest and in posterior organ perfusion. In turn, strict time limits were applied: 15min maximum from the time of cardiorespiratory arrest to the start of ALS by the 061 Service, and 120min maximum from the start of ALS by the 061 Service to the start of organ preservation in the operating room. On the other hand, a rapid response team has been established, consisting of two transplant coordinators (physician and nurse), a nurse specifically trained in NHBD, and a vascular surgeon, which ensures a highly efficient response. Another factor contributing to explain the results obtained is the adoption of a specific information protocol for the relatives of potential non-heart beating donors, applied by the emergencies professionals of the 061 Service, together with immediate attendance by the User Information and Assistance Service of the family upon reaching the hospital–which results in a very low donation rejection rate. The transplant coordinators are intensivists who work in the ICU that receives the potential donors. This in turn improves fluidity and affords maximum utilization of the human and technical resources of the Unit, guaranteeing a fast and secure in-hospital circuit between the ICU and the operating room. Lastly, the use of two organ preservation techniques - extracorporeal circulation under normothermal conditions and renal perfusion with preservation solution in hypothermia–optimizes the yield in terms of the number of organs per donor, in both polytraumatized patients and in situations of failed extracorporeal circulation.
In 1993, at the start of the Spanish donation and transplant program, 43% of all organ donations came from deaths secondary to head injuries in traffic accidents. This percentage has since decreased to only 5.1% in the year 2011. This change in donor profile influences the total number of donors in the country. NHBD programs can contribute to ensure that organ donation does not decrease.
ConclusionsThe initial results obtained support the development of NHBD programs in cities of under 500,000 inhabitants.
During the study period, NHBD has represented 20.19% of the renal transplants and 19.6% of all organ donations in the province of Granada, allowing a donation rate of 63 donors pmp in the year 2011.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pérez-Villares J.M., et al. Código alfa. Inicio de un nuevo programa de donación en asistolia. Med Intensiva. 2013;37:224-31.