To explore contributing factors (CFs) associated to related critical patients safety incidents.
DesignSYREC study post hoc analysis.
SettingA total of 79 Intensive Care Departments were involved.
PatientsThe study sample consisted of 1.017 patients; 591 were affected by one or more incidents.
Main variablesThe CFs were categorized according to a proposed model by the National Patient Safety Agency from United Kingdom that was modified. Type, class and severity of the incidents were analyzed.
ResultsA total 2965 CFs were reported (1729 were associated to near miss and 1236 to adverse events). The CFs group more frequently reported were related patients factors. Individual factors were reported more frequently in near miss and task related CFs in adverse events. CFs were reported in all classes of incidents. The majority of CFs were reported in the incidents classified such as less serious, even though CFs patients factors were associated to serious incidents. Individual factors were considered as avoidable and patients factors as unavoidable.
ConclusionsThe CFs group more frequently reported were patient factors and were associated to more severe and unavoidable incidents. By contrast, individual factors were associated to less severe and avoidable incidents. In general, CFs most frequently reported were associated to near miss.
Analizar los factores contribuyentes (FC) que intervienen en la aparición de incidentes relacionados con la seguridad del paciente crítico.
DiseñoAnálisis post hoc del estudio SYREC.
ÁmbitoUn total de 79 servicios de Medicina Intensiva.
PacientesUn total de 1.017 pacientes, de los que se incluyeron 591 en los que se notificó al menos un incidente.
Variables de interés principalesFC categorizados según una adaptación del modelo propuesto por la National Patient Safety Agency del Reino Unido. Tipo, clase y gravedad de los incidentes relacionados con la seguridad del paciente.
ResultadosSe notificaron 2.965 FC (1.729 se comunicaron en incidentes sin daño y 1.236 en eventos adversos). El grupo de FC más frecuente fue el relacionado con el paciente. Los FC relacionados con el profesional se notificaron más en los incidentes sin daño. En cambio, los relacionados con la tarea se comunicaron más en los eventos adversos. Se declararon FC en todas las clases de incidentes. La mayoría de FC se notificaron en los incidentes menos graves aunque los FC relacionados con el paciente se asociaron a incidentes de mayor gravedad. Los incidentes que se asociaron a los FC relacionados con el profesional se consideraron evitables y los FC relacionados con el paciente, inevitables.
ConclusionesLos FC relacionados con el paciente fueron los más frecuentes y se relacionaron con los incidentes más graves y considerados inevitables. Los relacionados con el profesional se notificaron en las categorías menos graves y se consideraron evitables. La identificación de FC fue más frecuente en los incidentes sin daño.
The critical patient care environment is extremely complex. In Departments of Intensive Care Medicine (DICMs), factors such as the seriousness of the patient condition, the communication barriers, the invasive therapeutic and diagnostic procedures used,1 and the volume of information managed all contribute to the appearance of incidents related to patient safety.2
Although not all healthcare related incidents that occur in the DICM actually affect the patients, some of them can cause temporary damage requiring additional observation and care, prolonging hospital stay and–in some cases–causing permanent damage or even death.3
Two aspects must be underscored in this regard. Firstly, most incidents detected in the DICM are avoidable.4 Secondly, although errors can occur in all areas of the hospital, patients admitted to the DICM are more vulnerable, and the consequences are more serious.5,6
In the patient safety context, it is admitted that most incidents related to medical care are a consequence of active error on the part of the professionals, favored by factors latent within the system. The analysis of these factors, applied to clinical safety, has been carried out based on the results of safety analyses in other fields such as aviation.7
A modern approach by those institutions that aim to effectively address patient safety with the purpose of reducing the number of incidents related to medical care inevitably includes knowledge of the causes underlying such incidents and their contributing factors (CFs).8 Furthermore, in-depth knowledge of these factors makes it possible to distinguish between those that influence an isolated incident and those which are common to incidents within a certain institution or Department.9
The systematic classification of CFs and their analysis should allow the development of strategies for improving the defenses and failures of the system. In Spain there is no exhaustive information on incidents related to medical care in the critical care setting, and the lack of data is even more manifest when considering the factors related to the appearance of such incidents.10 For this reason, a collaborative agreement was established between the Spanish Ministry of Health and the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC) to conduct the multicenter Safety and Risk in the Critical Patient (Seguridad y Riesgo en el Enfermo Crítico, SYREC) study–the main objective of which was to estimate the incidence of adverse events (AEs) and near-miss incidents (NMIs) in the Intensive Care setting, classify them, and assess their impact and avoidability.11 The results of this study have recently been published.4
The present study analyzes the factors that contribute to the appearance of NMIs and AEs in the critical patient, and explores their relation to the class, severity and avoidability of incidents related to medical care, based on the results of the SYREC study.
Material and methodsDesign: A post hoc analysis was made of the SYREC study (a multicenter, prospective cohort observational study with a follow-up duration of 24h, conducted in the DICM).
Inclusion criteria: All patients admitted to the participating DICMs during the observation period. The subjects who were admitted, were discharged, or who died during the study period were included.
Endpoints and measures:
- a)
Primary (reported CFs): we analyzed the frequency, incidence and type of CF. Categorization of the CFs was based on an adaptation of the model proposed by the National Patient Safety Agency (NPSA) of the United Kingdom.12 The CFs were classified into 8 groups: individual factors of the professional, team and social factors, communication factors, task related factors, equipment and resource related factors, working conditions, patient factors, and training and educational factors. Each group of CFs in turn could comprise one or more subfactors. For each reported patient safety related incident (PSRI), the notifier could consider one or more groups of CFs and, within each group, one or more related subfactors.
- b)
Secondary (classes of incidents related to medical care): we included NMIs and AEs occurring, detected and reported during the observation period in the Unit, as well as those occurring outside the Unit but which were the reason for admission to the latter. Near-miss incidents were defined as incidents causing no patient damage, either because they fail to actually reach the patient, or because they produce no consequences even if they do reach the patient. Adverse events in turn were defined as unforeseen and unexpected incidents reported by the professionals and which cause damage, disability or prolongation of stay, or death as a consequence of medical care and which are unrelated to the evolution or possible complications of the patient background disease.
Class of incident (classification adopted by the authors based on the literature): The incidents were divided into in 11 classes: (1) medication; (2) blood and blood product transfusions; (3) airway and mechanical ventilation; (4) vascular accesses, catheters, tubes, drains and sensors; (5) medical equipment and system failure; (6) diagnostic error; (7) diagnostic tests; (8) nursing care; (9) procedures; (10) nosocomial infection; and (11) surgery related incidents.
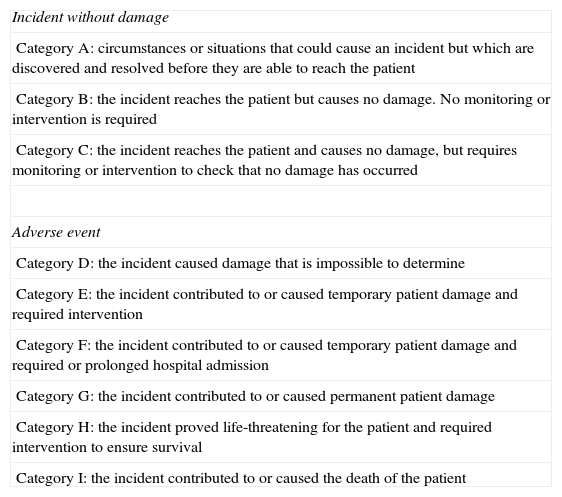
Severity of the incident: This was analyzed based on an adaptation of the classification of medication errors of the Ruiz-Jarabo group.13 The changes affected categories A and B, which were merged. A new category (category D) was added, due to the difficulty in many cases of assessing the consequences of the incident (Table 1).
Severity categories of the incidents according to their classification.
| Incident without damage |
| Category A: circumstances or situations that could cause an incident but which are discovered and resolved before they are able to reach the patient |
| Category B: the incident reaches the patient but causes no damage. No monitoring or intervention is required |
| Category C: the incident reaches the patient and causes no damage, but requires monitoring or intervention to check that no damage has occurred |
| Adverse event |
| Category D: the incident caused damage that is impossible to determine |
| Category E: the incident contributed to or caused temporary patient damage and required intervention |
| Category F: the incident contributed to or caused temporary patient damage and required or prolonged hospital admission |
| Category G: the incident contributed to or caused permanent patient damage |
| Category H: the incident proved life-threatening for the patient and required intervention to ensure survival |
| Category I: the incident contributed to or caused the death of the patient |
Source: Adapted from the classification of medication error of the Ruiz-Jarabo group. Otero-López et al.13
Avoidability of the incident: The NMIs and AEs were classified as follows according to the criterion of the observer: undoubtedly avoidable, possibly avoidable, possibly unavoidable or unavoidable.
Procedure: All the DICMs in Spain (a total of 220) were invited to participate through the SEMICYUC website, e-mail or conventional mail. A total of 79 DICMs finally agreed to participate. After confirming acceptance, each Unit assigned two coordinators (a physician and a nurse), who in turn received a document describing the study design and providing instructions to standardize the inclusion criteria and data collection. Supportive and training material was also made available to all the professionals in the Units, before the start of the study.
A questionnaire distributed in paper format was used for data collection. On the day of the study, all the physicians, nurses and assistant personnel completed the corresponding questionnaires on a voluntary and anonymous basis. The coordinators in each center checked correct completion of the questionnaires, entered the data in an electronic format and forwarded them by e-mail to the principal investigators of the study.
Data collection quality control: All the reported incidents were individually reviewed by the principal investigators of the study. A consensus meeting was subsequently held to examine the discrepancies and decide whether to include or exclude them, and to reclassify those incidents which were considered to be incorrectly classified.
Statistical analysis: A descriptive analysis was made of all the variables included in the study. Qualitative variables were reported as frequency distributions, while quantitative variables were presented using the mean and standard deviation (SD) as dispersion measures, or the median and interquartile range (IQR) in the event of an asymmetric distribution. In the bivariate analysis, the possible association between quantitative variables was evaluated using the chi-squared test. The comparison of means for two independent samples in turn was carried out using the Student t-test for independent samples, with analysis of variance (ANOVA) in the case of more than two means–in both cases considering a symmetric (normal) sample distribution as established by the homogeneity of variance analysis. In the case of an asymmetric distribution, we used the median test for the contrasting of hypotheses. The data were entered in a MS Access database, followed by statistical processing with the SPSS version 19.0 statistical package.
Confidentiality and ethical considerations: Since this was an observational study involving no interventions of any kind, the obtainment of informed consent was not considered necessary. The study was approved by the Clinical Research Ethics Committee (CREC) of Aragon. Each DICM agreed to obtain the required permissions at local level. In accordance with Act 15/1999 referring to the protection of personal data,14 and with Act 41/2002, of 14 November, regulating patient autonomy and rights and obligations in relation to clinical documentation and information,15 the anonymity of the patients and of the personnel involved in the incidents was ensured in the collected and submitted data. The results of this study were not directly binding for either the professionals or the patients, and the decision was made to publish both the positive and the negative findings.
ResultsA total of 79 DICMs belonging to 76 hospitals participated in the study, with the inclusion of 1017 patients. At least one incident was reported in 591 of these patients (58%). During the study period a total of 1424 patient safety related incidents (PSRIs) were reported: 943 NMIs (66%) and 481 AEs (44%). One or more contributing factors (CFs) were reported in 1247 PSRIs (87.57%).
Reported contributing factorsA total of 2965 CFs were documented, of which 1729 (58.31%) were reported in relation to 943 NMIs and 1236 (41.69%) in relation to 481 AEs–this representing a median of one CF per NMI (IQR 1–2) and of two CFs per AE (IQR 1–3)(p < 0.001). No CFs was reported in 12.7% of the NMIs and in 11.9% of the AEs.
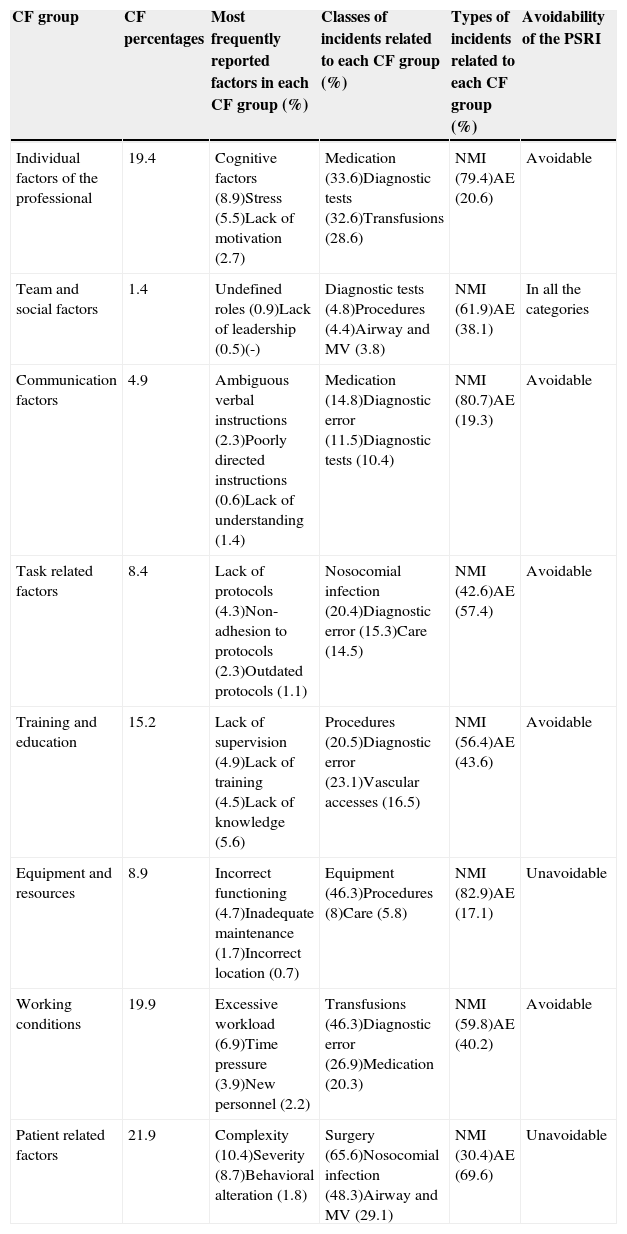
The most frequently reported CFs corresponded to patient related factors (21.9%), followed by the working conditions (19.9%), and individual factors of the professional (19.4%). Table 2 describes the frequencies with which the different groups of CFs were reported. The table also describes the most common subfactors cited in each group of CFs and their main characteristics. It should be noted that complexity and severity were the factors most often cited in the group of patient related factors.
Characteristics of the contributing factors distributed by groups.
| CF group | CF percentages | Most frequently reported factors in each CF group (%) | Classes of incidents related to each CF group (%) | Types of incidents related to each CF group (%) | Avoidability of the PSRI |
|---|---|---|---|---|---|
| Individual factors of the professional | 19.4 | Cognitive factors (8.9)Stress (5.5)Lack of motivation (2.7) | Medication (33.6)Diagnostic tests (32.6)Transfusions (28.6) | NMI (79.4)AE (20.6) | Avoidable |
| Team and social factors | 1.4 | Undefined roles (0.9)Lack of leadership (0.5)(-) | Diagnostic tests (4.8)Procedures (4.4)Airway and MV (3.8) | NMI (61.9)AE (38.1) | In all the categories |
| Communication factors | 4.9 | Ambiguous verbal instructions (2.3)Poorly directed instructions (0.6)Lack of understanding (1.4) | Medication (14.8)Diagnostic error (11.5)Diagnostic tests (10.4) | NMI (80.7)AE (19.3) | Avoidable |
| Task related factors | 8.4 | Lack of protocols (4.3)Non-adhesion to protocols (2.3)Outdated protocols (1.1) | Nosocomial infection (20.4)Diagnostic error (15.3)Care (14.5) | NMI (42.6)AE (57.4) | Avoidable |
| Training and education | 15.2 | Lack of supervision (4.9)Lack of training (4.5)Lack of knowledge (5.6) | Procedures (20.5)Diagnostic error (23.1)Vascular accesses (16.5) | NMI (56.4)AE (43.6) | Avoidable |
| Equipment and resources | 8.9 | Incorrect functioning (4.7)Inadequate maintenance (1.7)Incorrect location (0.7) | Equipment (46.3)Procedures (8)Care (5.8) | NMI (82.9)AE (17.1) | Unavoidable |
| Working conditions | 19.9 | Excessive workload (6.9)Time pressure (3.9)New personnel (2.2) | Transfusions (46.3)Diagnostic error (26.9)Medication (20.3) | NMI (59.8)AE (40.2) | Avoidable |
| Patient related factors | 21.9 | Complexity (10.4)Severity (8.7)Behavioral alteration (1.8) | Surgery (65.6)Nosocomial infection (48.3)Airway and MV (29.1) | NMI (30.4)AE (69.6) | Unavoidable |
AE: adverse event; CF: contributing factor; PSRI: patient safety related incident; NMI: near-miss incident; MV: mechanical ventilation.
The groups of CFs corresponding to equipment and resources, communication and individual professional factors were more frequently reported in NMIs (82.9%, 80.7% and 79.4%, respectively). In contrast, the groups of CFs related to patient, task and training and education were more frequently reported in AEs (69.6%, 57.4% and 43.6%, respectively) (Table 2).
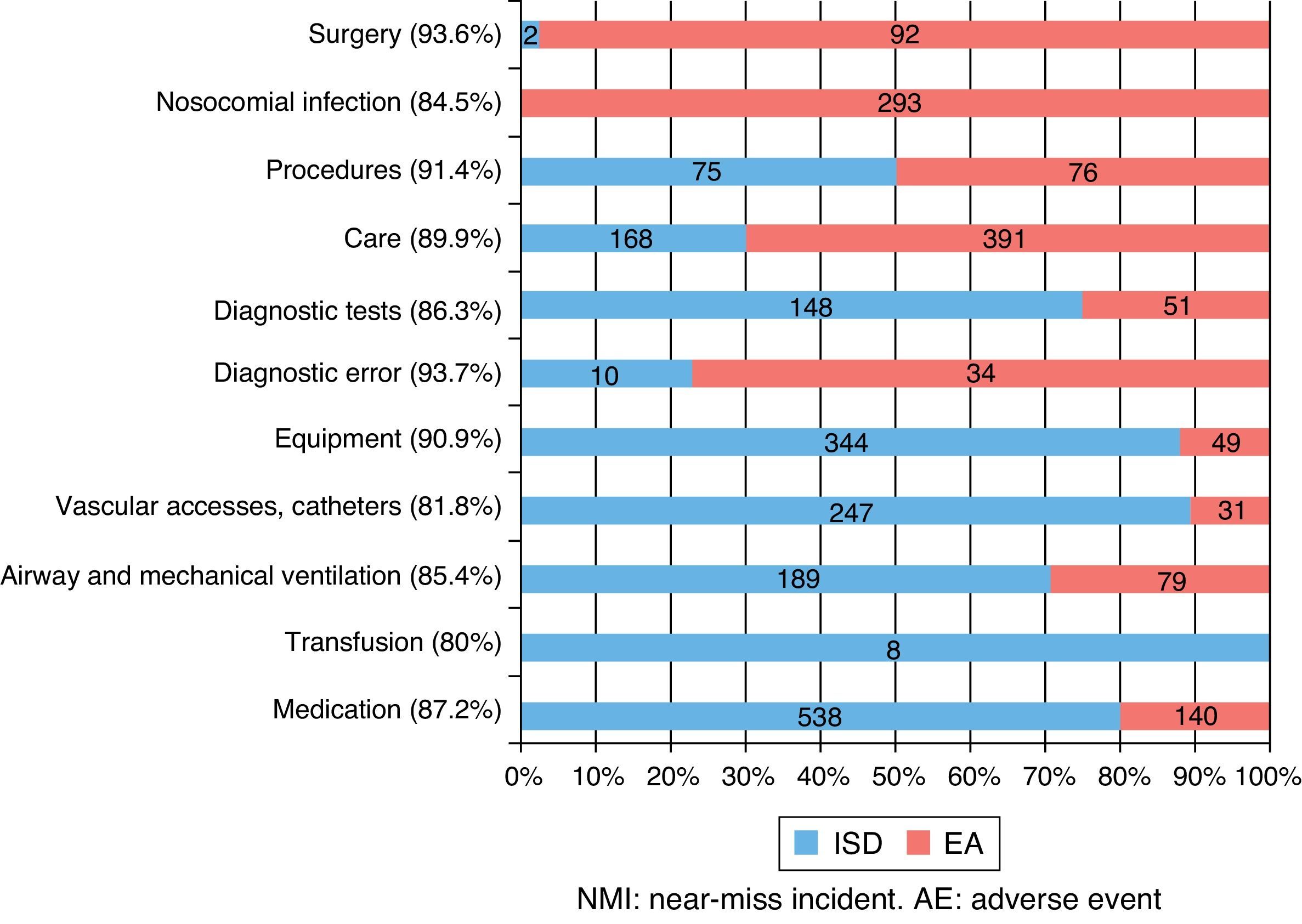
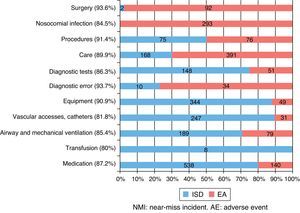
Reported contributing factors according to the classes of patient safety related incidentsIncidents corresponding to all 11 of the considered classes were reported. The class of incidents with the greatest percentage of reported CFs corresponded to diagnostic error (93.7%; 16 incidents related to medical care, and only one incident with no CF) and surgery (93.6%; 47 incidents related to medical care, only 3 incidents with no CF). In contrast, the class of incidents with the lowest percentage of reported CFs corresponded to transfusion (80%). However, it must be noted that only 5 incidents were documented in this class.
Table 2 describes the classes of incidents related to each group of CFs. Within the group of CFs related to the patient, the most common incidents corresponded to surgery. In contrast, the working conditions and individual factors of the professional were more often associated to transfusion and medication incidents.
On the other hand, Fig. 1 summarizes the distribution of the reported CFs according to the class and type of incident involved. Of note is the fact that all reported CFs referred to transfusion corresponded to NMIs. In contrast, 97.9% of the CFs reported in the context of surgical incidents corresponded to AEs.
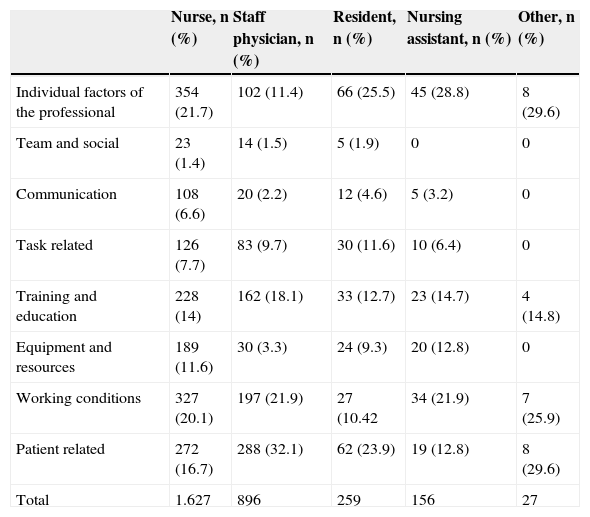
Groups of contributing factors in relation to the reporting professionalOf the 2965 documented CFs, 1627 were reported by nursing personnel, 896 by staff physicians, 259 by residents in training, 156 by nursing assistants, and 27 by other professionals. In general, physicians were the most frequent reporters of patient related factors (32.1%) and, in contrast, the least frequent reporters of individual factors of the professional (11.4%) and factors related to equipment and resources (3.3%). On the other hand, residents in training were the professionals who reported the fewest incidents involving CFs related to working conditions (10.4%). Table 3 shows the number of CFs reported according to groups of factors and the reporting persons.
Distribution of the groups of contributing factors according to the reporting professional.
| Nurse, n (%) | Staff physician, n (%) | Resident, n (%) | Nursing assistant, n (%) | Other, n (%) | |
|---|---|---|---|---|---|
| Individual factors of the professional | 354 (21.7) | 102 (11.4) | 66 (25.5) | 45 (28.8) | 8 (29.6) |
| Team and social | 23 (1.4) | 14 (1.5) | 5 (1.9) | 0 | 0 |
| Communication | 108 (6.6) | 20 (2.2) | 12 (4.6) | 5 (3.2) | 0 |
| Task related | 126 (7.7) | 83 (9.7) | 30 (11.6) | 10 (6.4) | 0 |
| Training and education | 228 (14) | 162 (18.1) | 33 (12.7) | 23 (14.7) | 4 (14.8) |
| Equipment and resources | 189 (11.6) | 30 (3.3) | 24 (9.3) | 20 (12.8) | 0 |
| Working conditions | 327 (20.1) | 197 (21.9) | 27 (10.42 | 34 (21.9) | 7 (25.9) |
| Patient related | 272 (16.7) | 288 (32.1) | 62 (23.9) | 19 (12.8) | 8 (29.6) |
| Total | 1.627 | 896 | 259 | 156 | 27 |
CF: contributing factor.
Most of the CFs (2011; 67.8%) corresponded to incidents classified as being less serious (categories A and D), while 954 (32; 2%) corresponded to more serious incidents (categories E-I). The group of CFs related to greatest severity of the PSRIs corresponded to patient related factors.
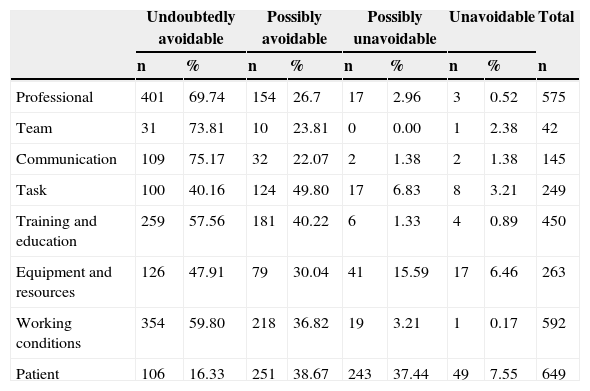
Groups of contributing factors in relation to the avoidability of the incidentA total of 2535 CFs corresponded to 1136 incidents related to patient safety classified as “undoubtedly avoidable” or “possibly avoidable”, while 430 CFs corresponded to 288 incidents classified as “possibly unavoidable” or “unavoidable”. Table 4 shows the distribution of reported CFs by groups and according to the avoidability of the incident. The individual factors of the professional and factors related to the working conditions were associated to avoidable PSRIs. In contrast, the CFs related to the patient and equipment and resources were associated to unavoidable PSRIs.
Distribution of reported contributing factors according to avoidability of the incident.
| Undoubtedly avoidable | Possibly avoidable | Possibly unavoidable | Unavoidable | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | |
| Professional | 401 | 69.74 | 154 | 26.7 | 17 | 2.96 | 3 | 0.52 | 575 |
| Team | 31 | 73.81 | 10 | 23.81 | 0 | 0.00 | 1 | 2.38 | 42 |
| Communication | 109 | 75.17 | 32 | 22.07 | 2 | 1.38 | 2 | 1.38 | 145 |
| Task | 100 | 40.16 | 124 | 49.80 | 17 | 6.83 | 8 | 3.21 | 249 |
| Training and education | 259 | 57.56 | 181 | 40.22 | 6 | 1.33 | 4 | 0.89 | 450 |
| Equipment and resources | 126 | 47.91 | 79 | 30.04 | 41 | 15.59 | 17 | 6.46 | 263 |
| Working conditions | 354 | 59.80 | 218 | 36.82 | 19 | 3.21 | 1 | 0.17 | 592 |
| Patient | 106 | 16.33 | 251 | 38.67 | 243 | 37.44 | 49 | 7.55 | 649 |
AE: adverse event; CF: contributing factor; NMI: near-miss incident.
The contributing factors (CFs) that intervene in the appearance of patient safety related incidents (PSRIs) have been little investigated in the Intensive Care setting. To date, and from outside the context of critical care, the different publications have attempted to investigate CFs through retrospective studies16–19 or based on reporting systems.20–23 More recently, studies from the perspective of medicine based on evidence have attempted to structure CFs into groups that can help us understand the appearance of PSRIs.24 In this regard, Lawton et al. identified active errors (failure to adhere to norms and protocols), together with factors related to the individual (knowledge and experience), and communication deficiencies, as the groups of CFs most frequently implicated in the appearance of PSRIs. The same authors also underscored a weakness that can be extended to any study that obtains information through reporting: the reporting professional is probably not an expert in safety matters, and is only able to point to the causes closest to the incident.
In our study, based on voluntary reporting encouraged by the coordinators, the most frequently reported CFs were those related to the patient. This is not surprising, since critically ill patients are particularly vulnerable to PSRIs because of the inherent seriousness of their condition. The second most frequently reported CFs corresponded to the working conditions. In this regard, Sanghera et al.25 pointed to the working conditions as the main CFs associated to medication error in critical patients, followed by communication related factors.
The data contained in the literature are heterogeneous. As an example, studies based on systems for reporting incidents in DICMs have found the most frequently reported CFs to be human factors, followed by systemic factors such as the working conditions, equipment and communication, among others.26 On the other hand, and likewise based on a multicenter reporting system in different North American DICMs, Holzmueller et al.27 found the CFs most frequently associated to PSRIs to be related to training and education, followed by communication related factors. Probably one of the elements that explain the lack of concordance in relation to the reported CFs is the methodology used in detecting the incidents, which can give rise to different interpretations regarding the CFs.26
We consider a number of the findings of our study to be of interest. On one hand, the number of CFs reported in AEs was greater than in NMIs. Although the causal mechanism underlying incidents with and without damage or injury is similar, professionals identify more CFs when the patient experiences damage. This may be because the search to identify what has happened is more intense when damage in the form of an AE has effectively occurred.9 On the other hand, it should be mentioned that the reported CFs differ when separately considering NMIs and AEs. Among the former, the most frequently reported CFs corresponded to individual factors of the professional, followed by communication factors. In contrast, on considering AEs, the most frequently reported CFs were seen to be related to the task and to the patient. It should be noted that the group of CFs related to the task includes aspects as important as the lack of specific protocols or failure to adhere to the existing protocols. The former problem is relatively easy to solve by developing the necessary protocols, while the latter (failure to adhere to the existing protocols or even to internationally accepted treatment guides) is the subject of continuous analysis.28,29
Another aspect that should be commented is the correlation of the CFs to the class of PSRI. In this regard, patient related factors–which generally speaking were the most frequently cited CFs–were associated to surgery related incidents. This may be because surgical procedures are typically performed in seriously ill patients. In turn, professional factors, which were the most commonly reported CFs in NMIs, were associated to medication error. Lastly, task related factors, which were the most commonly reported CFs in AEs, were associated to nosocomial infection. This circumstance again points to error of omission (failure to adhere to the clinical practice guides) as possibly being the cause of AEs as sensitive as infection associated to medical care.30
In relation to avoidability, most of the incidents were classified as avoidable, in coincidence with the observations of other authors.19 The groups of CFs related to avoidable PSRIs were individual factors of the professional, followed by equipment related factors. In contrast, the unavoidable incidents were fundamentally associated to patient related factors.
This study has some limitations. On one hand, in relation to the methodology used, the incidents were recorded by professionals working in the DICMs. Although these professionals had received basic information on patient safety, they cannot be regarded as experts in this field–a fact that limits the detection of CFs. At the same time, although reporting by the professionals can allow the identification of CFs that are not easy to identify with other methods (e.g., case history reviews), it may limit assessment of the CFs by not offering a true root cause analysis. Given the voluntary and anonymous nature of reporting in the study, it was not possible to assign (as is done in other methods) a second evaluator to allow concordance analysis. On the other hand, studies based on voluntary reporting more frequently identify active factors, while other studies such as those of an observational nature or based on the use of questionnaires, favor the identification of CFs classified as belonging to other categories.31 In turn, identification of the CFs might not be extrapolatable to other settings outside Intensive Care. A systematic review of CFs related certain factors to the Department or Service in which the study was carried out.20 Lastly, the most frequently reported CFs (almost 20% of the total) were associated to the complexity and seriousness of the patient condition. In view of the study setting, this offers little information, since most critically ill patients present such CFs. Furthermore, such factors were associated to more serious incidents and unavoidable incidents–a correlation that may be due to factors inherent to the reporting persons and to a lack of safety culture among the healthcare professionals. Many professionals consider the most serious incidents to be complications of the disease process itself, and are therefore reported as being patient related and unavoidable–without recognizing them as patient safety problems.
While acknowledging the limitations commented above, we consider that the information obtained from the analysis of our results is very useful, since it allows identification and analysis of the CFs with the ultimate aim of better understanding the circumstances that favor or accompany PSRIs in Spanish DICMs. Although there are reference publications in different countries, we consider the availability of studies in our own country to be essential in order to enhance awareness of the importance of a problem that has been little studied in our setting, and which consequently may be underestimated.
In sum, the most frequently reported CFs were those related to the patient, followed by factors related to the working conditions and the professional. Most CFs were reported in association to incidents classified as being less serious and avoidable. The CFs related to the professional were associated to less serious and avoidable incidents–fundamentally NMIs–while the CFs related to the patient were associated to more serious incidents that moreover were classified as unavoidable. The majority of the CFs were reported by nursing personnel, followed by physicians.
Financial supportThis study was carried out thanks to a collaborative agreement between the Spanish Ministry of Health and the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC).
Conflict of interestThe authors declare that they have no conflicts of interest.
The authors thank the coordinators of the participating DICMs for the support given to this project.
Cánovas Robles J, Perales Pastor R, HGU Alicante (Alicante); Sánchez Ortega D, Serrano Calvache JA, H. de Torrecárdenas (Almería); de Rojas Román JP, Ramos Carbonero Y, H. Comarcal de Antequera (Antequera); Gutiérrez Fernández MJ, Fernández Álvarez V, H. San Agustín (Avilés); Umaran Sarachu MI, Monguillo Martiregui MJ, H. de Cruces (Baracaldo); Fernández Dorado F, Figueras Coloma E, Centro Médico Delfos (Barcelona); Morillas Pérez J, Portillo Jaurena E, SCIAS-H. de Barcelona (Barcelona); Sánchez Segura JM, Sola Sole N, H. Santa Creu i Sant Pau (Barcelona); Zavala Zegarra E, Cirerea A, H. Clínic-UCI Quirúrgica (Barcelona); Vázquez Sánchez A, Abad Peruga V, H. del Mar (Barcelona); Robles González A, Borja García MI, H. Vall d¿Hebron-Traumatología (Barcelona); Bellot Iglesias JL, Martínez Molina M, H. de Baza (Baza); Romero Pellerrejo J, Campillo Temiño C, Complejo Hospitalario de Burgos (Burgos); Martínez Hernández J, Alarcón Simarro N, H. Santa María del Rosell (Cartagena); Álvaro Sánchez R, Bernat Adell A, H. Universitario Asociado General de Castellón (Castellón); Molina Domínguez E, Ortega Carnicer J, H.G. de Ciudad Real (Ciudad Real); Alcalá López A, Pastor M, HGU de Elche (Elche); Palomeque Rico A, Nicolás Zambudio G, H. Sant Joan de Deu (Espluges); Alonso Ovies A, Balugo Huertas S, H. de Fuenlabrada (Fuenlabrada); Audicana Uriarte J, Sánchez Villamar AM, H. de Galdakao (Galdakao); Álvarez Villuendas A, Garfingou Llenas D, H. Dr. Josep Trueta (Gerona); Roca Guiseris J, García R, H. Virgen de las Nieves (Granada); Fernández del Campo R, Buendía F, H. de Hellín (Hellín); Bartual Lobato E, García Verdejo JA, H. Can Misses (Ibiza); Verduras Ruiz MA, Rodrigo Frontelo R, H. Severo Ochoa (Leganés); Pavía Pesquera MC, Pardos Peirós E, H. San Pedro (Logroño); Blanco Pérez J, Murado Bouso AM, H. Xeral-Calde Lugo (Lugo); Gómez Tello V, del Pozo Y, Clínica Moncloa (Madrid); Reyes García A, Toledano Peña J, H.U. de la Princesa (Madrid); Ramos Polo J, Suay Ojalvo C, H. Clínico San Carlos (Madrid); Menéndez de Suso JJ, Segovia Gaitán M, H. San Rafael (Madrid); Sáenz Casco L, Andrés Sarriá M, H. Central de la Defensa Gómez Ulla (Madrid); Jiménez Lendínez M, Romero C, H.U. La Paz (Madrid); Arias Verdú MD, García Santana JL, H. Parque San Antonio (Málaga); Arboleda Sánchez JA, Velasco Bueno JM, H. Costa del Sol (Marbella); Solsona Perlasia M, Vilalta Llibre M, Consorci Sanitari del Maresme (CSdM) (Mataró); García Fernández AM, Morales Adeva L, H. de Mérida (Mérida); Galdos Anuncibay P, Arias Castro I, H.G. de Móstoles (Móstoles); Gómez Ramos MJ, Cevidanes M, H.G.U. Reina Sofía (Murcia); Martínez Fresneda M, Banacloche Cano C, H. Virgen de la Arrixaca (Murcia); Carrillo Alcaraz A, Peñalver F, H. Morales Meseguer (Murcia); Iglesias Fraile L, Álvarez Méndez B, H.G. de Asturias (Oviedo); Rialp Cervera G, Bestard Socías C, H. Son Llàtzer (Palma de Mallorca); Rodríguez Albarrán F, Ballester Belcos R, Clínica San Miguel (Pamplona); Ramos Castro J, Herranz Ayesa MV, H. Virgen del Camino (Pamplona); Martínez Urionabarrenetxea K, Elizondo Soto A, H. de Navarra (Pamplona); Gil Cebrián J, Delgado Poullet N, H.U. Puerto Real (Puerto Real); Prieto Valderrey F, Nieto Galeano J, H. Santa Bárbara (Puertollano); Rovira Angles C, Cerrillo E, H.U. Sant Joan de Reus (Reus); Domínguez López S, Malnero López M, H. Valle del Nalón (Riaño); Baigorri González F, Jam Gatell R, H. de Sabadell-Corporació Parc Taulí (Sabadell); Lacueva Moya V, Hernández Santamaría F, H. de Sagunt (Sagunto); González Robledo J, Coca Hernández MA, H.U. de Salamanca (Salamanca); Azkárate Ayerdi B, Marcos A, H. Donostia (San Sebastián); Rull Rodríguez VE, Morras Pineda B, Complejo Hospitalario de Soria-H. de Santa Bárbara (Soria); Gilavert Cuevas MC, Aragonés M, H. Joan XXIII (Tarragona); Jurado Castro MT, Bell Ribatallada M, H. de Terrasa (Terrasa); Pérez-Pedrero Sánchez-Belmonte MJ, Pinilla López A, H. Virgen de la Salud (Toledo); Vázquez Casas JR, Herrero Gómez E, H. Verge de la Cinta (Tortosa); Soto Ibáñez JM, Romero Morán MA, H.U. Dr. Peset (Valencia); García Galiana E, Fernández Martínez A, Fundación Instituto Valenciano de Oncología (Valencia); Domínguez Quintero LA, Acebes Sancho BE, Domínguez Quintero LA, Palencia García MA, H. Río Hortega-Polivalente (Valladolid); Tizón Varela AI, de Castro Rodríguez P, Complexo Hospitalario Universitario de Vigo-H. Xeral Cíes (Vigo); Manzano Ramírez A, Ruiz de Ofenda E, H. Santiago Apóstol (Vitoria); Marcos Gutiérrez A, Larruscain León MV, H. Virgen de la Concha (Zamora); Temiño Palomera S, Lasheras Palomero L, Mutua de Accidentes de Zaragoza (Zaragoza); Gutiérrez Cía I, Moreno MA, H. Clínico Universitario Lozano Blesa-UCI Quirúrgica (Zaragoza); Tirado Angles G, González Caballero M, H. Royo Villanova (Zaragoza); Valero García R, Casa Venta J, H.U. Miguel Servet-Coronaria (Zaragoza); García Mangas P, Mahave Carrasco R, H.U. Miguel Servet-Polivalente (Zaragoza); Olmos Pérez F, Villabona Resano J, H.U. Miguel Servet-Cirugía Cardiaca (Zaragoza); Williams L, Patiño Y, Centro de Especialidades Anzoátegui, Lechería (Venezuela); Margarit Ribas A, Flamarique Zaratiegui MT, H. Nostra Senyora de Meritxell, Escaldes-Engordany (Andorra); Ortega RA, Sánchez Reinoso J, San Juan Bautista, Catamarca (Argentina); Diosdado Iraola Ferrer M, Mora Pérez Y, H.U. Dr. Gustavo Aldereguía Lima, Cienfuegos (Cuba); Carrazana Osorio V, Prieto Fuentemayor JR, H. Clínico-Quirúrgico Lucía Íñiguez Landín, Holguín (Cuba); Díaz Águila H, Companioni Sola Y, H. Mártires de 9 de Abril, Sagua la Grande (Cuba); Morales Valderas A, Solís Sotero M, H.U. Arnaldo Milian Castro, Santa Clara (Cuba).
Please cite this article as: Martín Delgado MC, Merino de Cos P, Sirgo Rodríguez G, Álvarez Rodríguez J, Gutiérrez Cía I, Obón Azuara B, et al. Análisis de los factores contribuyentes en incidentes relacionados con la seguridad del paciente en Medicina Intensiva. Med Intensiva. 2015;39:263–271.