To describe the incidence and clinical and epidemiological profile of patients with severe preeclampsia admitted to intensive care.
DesignA prospective, observational case series.
SettingA specific obstetric 8-bed ICU belonging to a university hospital with a total of 55 ICU beds.
PatientsA total of 262 patients admitted due to severe preeclampsia, eclampsia or HELLP syndrome.
InterventionDescriptive analysis of the population and complications in the ICU and hospital mortality.
ResultsThe mean patient age was 30.47±5.7years, with the following diagnóstico at admission: A total of 78% of the patients with severe preeclampsia, 16% with HELLP syndrome, and 6% with eclampsia, occurring in gestational week 31.85±4.45. In turn, 63% of the patients were nulliparous and had a low prevalence of previous diseases. The global complications rate was 14% (9% heart failure, 5% acute renal failure and 2% coagulopathy).
Maternal mortality was 1.5% (4 patients), and was associated with non-nulliparous status, the presence of complications, and toast >71mg/dl.
ConclusionsSevere preeclampsia has a low mortality rate (1.5%), though the complications rate is considerable (14%). The condition develops more often in nulliparous women during the third trimester of pregnancy.
Describir la incidencia y el perfil clínico y epidemiológico de las pacientes con preeclampsia grave que requieren ingreso en Cuidados Intensivos.
DiseñoEstudio observacional prospectivo de una serie de casos.
ÁmbitoUCI específica de enfermedad gineco-obstétrica de 8 camas, perteneciente a un hospital universitario de nivel 3, con una dotación de 55 camas de UCI en total.
PacientesUn total de 262 pacientes ingresadas por preeclampsia grave, eclampsia o síndrome HELLP.
IntervenciónAnálisis descriptivo de la población y de las complicaciones en UCI así como de la mortalidad intrahospitalaria.
ResultadosLa edad media fue de 30,47±5,7 años, con una distribución diagnóstica al ingreso de 78% de pacientes con preeclampsia grave, 16% por síndrome HELLP y 6% por eclampsia, que sucedió en la semana gestacional 31,85±4,45. El 63% de las pacientes fueron primigestas y presentaron escasa prevalencia de enfermedades previas. La tasa de complicaciones fue del 14% (fracaso cardiaco en 9%, insuficiencia renal aguda en 5% y coagulopatía en 2%).
La mortalidad materna fue 1,5% (4 pacientes) y se relacionó con la no-primigestación, la presencia de complicaciones y un nivel superior de la transaminasa GOT a 71mg/dl.
ConclusionesLa preeclampsia grave tiene una baja tasa de mortalidad (1,5%), no así de complicaciones (14%) y se presenta con mayor frecuencia en nulíparas durante el tercer trimestre de gestación.
Preeclampsia, a relatively common hypertensive disorder during pregnancy, manifests progressively and often gives rise to serious maternal and perinatal complications. While the etiology of preeclampsia is not clear, it is characterized by vasospasm and endothelial activation, with hypertension and proteinuria, after week 20 of pregnancy.
The incidence of preeclampsia is variable, since many studies have used estimations based only on hospital samples—a situation that could explain the relatively frequently reported figure of up to 5–10%, depending on the healthcare levels of the hospitals in which the studies are made. It has been estimated that about 7% of all pregnant women develop preeclampsia,1 though the percentage could be higher in less favorable socioeconomic settings, and in countries with a higher prevalence of cardiovascular disease.2 Although few estimations have been made in Spain, the existing data point to an incidence of 1–2%.3
Five percent of all cases of preeclampsia in turn ultimately progress toward eclampsia,4 and in up to 19% of the cases the condition can manifest as HELLP syndrome, which is associated to increased morbidity–mortality.5
The adverse maternal consequences in preeclampsia are fundamentally attributable to dysfunction of the central nervous system, liver or kidneys (hemorrhagic stroke, liver rupture or acute renal failure), and to bleeding associated to thrombocytopenia. Preeclampsia–eclampsia is one of the three most common causes of mortality in pregnant women, together with thromboembolic disease and postpartum hemorrhage.6
The criteria of severe preeclampsia were established by the Spanish Society of Gynecology and Obstetrics (Sociedad Española de Ginecologia y Obstetricia) in 2006, and refer to a subgroup of patients with increased maternal-fetal mortality and more frequent management in intensive care units (ICUs).7
The present study describes the epidemiology and risk and evolutive factors among patients with severe preeclampsia, eclampsia and HELLP syndrome.
Material and methodsA prospective observational study has been made of all the patients admitted to the maternal intensive care unit (ICU) of the Maternal-Children's Hospital pertaining to the Carlos Haya Hospital Complex (Málaga, Spain) due to severe preeclampsia, eclampsia or HELLP syndrome, between January 1999 and September 2008.
The Maternal-Children's Hospital serves 50% of the population of the city of Málaga, and is the only public hospital in the province equipped with a neonatal ICU. As a result, it is the reference center for patients with severe preeclampsia, eclampsia or HELLP syndrome in cases of early gestational age. The mentioned ICU is a specific, 8-bed gynecological-obstetric unit pertaining to the Carlos Haya Regional University Hospital—a third-level center with a total of 55 intensive care beds.
Severe preeclampsia is defined by the presence of systolic blood pressure (SBP) ≥140mmHg or diastolic blood pressure (DBP) ≥90mmHg as determined by two or more measurements spaced at least 6h apart, together with proteinuria (≥300mg in 24h urine), and some of the severity criteria indicated in Table 1. Eclampsia in turn is established when preeclampsia is accompanied by seizures or coma without any apparent cause. HELLP (hemolysis with elevated liver enzymes and low platelets) syndrome is another form of presentation of severe preeclampsia.
Signs and symptoms of severe preeclampsia (at least one of the following).
| –Manifestations of central nervous system dysfunction: blurry vision, scotomas, severe headache, altered consciousness |
| –Symptoms of Gleason capsule distension: severe pain in right hypochondrial region, nausea or vomiting |
| –Liver cell damage: transaminase elevation to twice the laboratory normal reference value |
| –Severe arterial hypertension: SBP ≥160mmHg or DBP ≥110mmHg on at least 2 occasions spaced 6h apart |
| –Thrombocytopenia: <100,000platelets per mm3 |
| –Proteinuria: ≥2g in 24h |
| –Oliguria <500ml in 24h |
| –Severe fetal growth retardation |
| –Lung edema or cyanosis |
| –Cerebrovascular stroke |
Clinical–epidemiological variables were recorded, together with laboratory test parameters, upon admission or at obstetric maneuvering. An analysis was made of maternal mortality and its related factors, during hospital admission due to causes related to gestosis, as well as of the factors related to the complications, referred to the development of heart failure (signs and symptoms of acute heart failure requiring oxygen therapy or mechanical ventilation—whether invasive or otherwise), coagulopathy (prothrombin activity decreased to below 50% or aPTT double the control value, or the existence of external or internal bleeding leading to patient destabilization and requiring the transfusion of blood products or surgery to secure control), or acute renal failure (characterized by doubling of the basal creatinine levels upon admission, or oligoanuria requiring extrarenal replacement measures). Likewise, the average duration of stay in the ICU was analyzed, along with the factors conditioning such a stay.
The termination of gestation was indicated on the basis of the presence of serious maternal complications, fetal suffering, or the absence of growth during at least one week, despite adequate treatment. The decision relating to the indication and timing was established jointly with the Department of Gynecology.
The patients and/or relatives were informed of the nature of the investigation and of its intended uses. Confidentiality was guaranteed at all times, with due confirmation that the information obtained would only be used for the specified purposes.
Statistical analysisQuantitative variables were expressed as the mean±standard deviation (SD), while qualitative variables were reported as frequencies (percentage). In the case of quantitative variables, comparisons between groups were made with the Student's t-test or with the nonparametric Mann–Whitney U-test where pertinent. Analysis of variance (ANOVA) in turn was used for the comparison of more than two groups. In the case of qualitative variables, comparisons were made with the chi-squared test or Fisher exact test.
Multivariate logistic regression analysis was used to identify predictors of mortality and the development of complications, while multiple linear regression was applied to the predictors of stay in the ICU. Those variables that proved significant in the bivariate analysis were included in the model.
In all cases statistical significance was assumed for p<0.05, with a 95% confidence interval.
ResultsThe study included 262 women with severe preeclampsia and a mean age of 30.47±5.7years, from among the 65,503 deliveries performed in our center. The incidence of severe preeclampsia in our series was 4/1000 deliveries. This implies that 0.37% of the patients hospitalized after giving birth required admission to the ICU due to severe preeclampsia, eclampsia or HELLP syndrome.
The diagnostic distribution upon admission was as follows: 204 (78%) with severe preeclampsia, 42 (16%) with HELLP syndrome, and 16 (6%) with eclampsia, occurring in gestational week 31.8±4.4. Sixty-three percent of the patients were in their first pregnancy, with a low prevalence of smoking (3.44%), obesity (10.3%) or previous arterial hypertension (17.8%). Pregnancy terminated in the form of cesarean section in 90% of the cases.
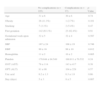
Table 2 reports some clinical and epidemiological variables according to the type of diagnosis involved.
Clinical-demographic characteristics according to diagnosis upon admission.
| Preeclampsia (n=203) | Eclampsia (n=16) | HELLP syndrome (n=43) | |
| Age | 31±5 | 29±7 | 30±6 |
| First gestation | 124 (61.1%) | 11 (68.8%) | 30 (69.8%) |
| Obesity | 23 (11.3%) | 3 (18.8%) | 1 (2.3%) |
| Arterial hypertension | 40 (19.7%) | 0 (0%) | 6 (14%) |
| Smoking | 7 (3.4%) | 1 (6.3%) | 1 (2.3%) |
| Gestational week upon admission | 32±4 | 36±5 | 31±4 |
| Stay in ICU (days) | 6±4 | 7±4 | 6±3 |
The gestational age of the women with eclampsia (35.6±5) was significantly greater than that of the patients with preeclampsia (32±4.2) or HELLP syndrome (30.9±3.8) (p=0.004 and p=0.001, respectively).
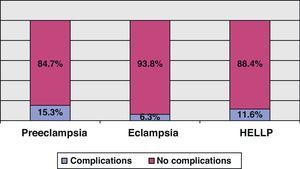
Fourteen percent of the patients developed some types of complication, specifically heart failure in 23 subjects (9%), acute renal failure in 14 (5%) and coagulation disorders in 6 cases (2%). Table 3 reports the clinical and laboratory test parameters of the patients according to whether they developed complications or not. There were no significant differences in the appearance of complications according to the diagnosis upon admission, as can be seen in Fig. 1.
Clinical and laboratory test data according to the development of complications.
| No complications (n=225) | Complications (n=37) | p-Value | |
| Age | 31±6 | 30±6 | 0.74 |
| Obesity | 26 (11.3%) | 1 (2.7%) | 0.101 |
| Smoking | 7 (3.1%) | 2 (5.4%) | 0.47 |
| First gestation | 142 (63.1%) | 23 (62.4%) | 0.91 |
| Gestational week upon admission | 32±5 | 32±4 | 0.587 |
| SBP | 167±24 | 168±19 | 0.746 |
| DBP | 99±16 | 99±10 | 0.812 |
| Hemoglobin | 11±2 | 10±2 | 0.005 |
| Platelets | 179.644±94.549 | 160.811±70.532 | 0.24 |
| GOT (AST) | 78±114 | 143±417 | 0.38 |
| GPT (ALT) | 81±98 | 104±228 | 0.57 |
| Uric acid | 6.2±1.3 | 6.3±1.9 | 0.66 |
| Stay (days) | 5±3 | 8±5 | 0.007 |
GOT: aspartate aminotransferase; GPT: alanine aminotransferase; DBP: diastolic blood pressure; SBP: systolic blood pressure.
The mean systolic blood pressure (SBP) was 171.7±82.7, while the mean diastolic blood pressure (DBP) was 99±15. No association was found between the mean SBP–DBP values and the development of complications.
The maternal mortality rate was 1.5% (2 patients diagnosed with severe preeclampsia and 2 with HELLP syndrome). First gestation was seen to be a protective factor in relation to maternal mortality (p=0.008), while mean transaminase concentration was correlated to increased mortality (p=0.0001).
The mean stay in the ICU was 5.6±3.4days. The patients who experienced some complication showed a longer stay in the Unit 5.3±2.8 vs 8±5 (p=0.007); this association was retained on an isolated basis for heart failure and acute renal failure (p=0.004 and p=0.0001, respectively), but not for coagulopathy (p=0.7).
The multivariate analysis of maternal mortality in all three disease conditions showed first pregnancy, the presence of complications, and GOT concentrations of over 71mg/dl to be explanatory factors for maternal mortality (Table 4).
Multivariate analysis of maternal mortality.
| β | Sig. | OR | 95%CI | ||
| Lower | Upper | ||||
| First gestation | −5.283 | 0.026 | 0.005 | 0.000 | 0.526 |
| GOT (AST) ≤71mg/dl | −4.402 | 0.041 | 0.012 | 0.000 | 0.834 |
| Presence of complications | 3.130 | 0.041 | 22.872 | 1.141 | 45.835 |
| Constant | 28.250 | 0.033 | |||
β: beta-coefficient; GOT (AST): aspartate aminotransferase; SBP: systolic blood pressure.
The independent predictors of stay in ICU were hemoglobin level (p=0.005, 95%CI −0.6, −0.1) and age gestational at the time of delivery (p=0.001, 95%CI −0.2, −0.07). Stay in the ICU was the only independent predictor of the development of complications (p=0.0001, OR 0.8, 95%CI 0.7–0.9).
DiscussionSevere preeclampsia, eclampsia and HELLP syndrome show a low incidence (4 cases/1000 deliveries) and low mortality (1.5%), though the associated complications rate is significant (14%), in the context of intensive care.
Maternal mortality due to obstetric causes varies according to the setting involved. Thus, in western countries the mortality rate varies between 0.2% according to the series of Zeeman,8 involving only patients with gestosis, and 3% according to Gilbert et al.9 In less developed countries, maternal mortality is much higher: 33% in the series of Okafor in Nigeria,10 22% in an Indian registry,11 almost 20% is a Tunisian series,12 and 10% according to the Turkish series of Demirkirian13—all these being series published in the present decade. In our setting, Olarra et al.14 published a retrospective study in which the maternal mortality rate was 7.5% among 149 seriously ill pregnant women admitted over a 7-year period, of which 50 were admitted due to preeclampsia.
Our series, referred exclusively to patients with severe preeclampsia, registered a maternal mortality rate of 1.5%—this percentage being similar to that reported by Zeeman8 and other authors in western countries. Given the small number of deaths, no firm conclusions can be drawn.
HELLP syndrome implies an increased maternal-fetal mortality risk. A hospital in our setting recorded a maternal mortality rate of 1.8%,15 vs 1% in the larger series published by Sibai et al.16
The criteria referred to obstetric admission to specialized critical care units vary according to the prevalence of different diseases, geographical areas, operative definitions of morbidity, hospitalization criteria, and management and treatment protocols, among other relevant aspects—although an obstetric intensive care utilization rate of between 1% and 3% of all deliveries has been estimated, particularly due to severe preeclampsia and massive bleeding.8 In our center, 0.37% of the women seen in the hospital during the study period required admission to the ICU because of severe preeclampsia—this percentage being similar to those reported for other countries in our setting.17
Complications during stay in the ICU are related to a poorer prognosis, and constituted the parameter of greatest specific effect in the multivariate analysis. The incidence of acute renal failure in preeclampsia has not been clearly established. A recent review18 of renal failure of obstetric origin points to preeclampsia as the cause of 20.9% of all renal failures in this setting, while another series including 31 complicated pregnancies with renal failure found 58% of the cases to be attributable to preeclampsia—giving rise to acute tubular necrosis—and one-half of the patients required hemodialysis during hospitalization.
Another study examined in the aforementioned review found 5% of all cases of gestosis to be complicated by acute renal failure—this figure reaching 7.3% in the subgroup of patients with HELLP syndrome. On the other hand, most of the cases documented in the literature recovered normal kidney function in a variable period of time, in coincidence with our own patients.18
Among the cardiovascular changes occurring in preeclampsia, mention should be made of a decrease in cardiac output and an increase in peripheral vascular resistance. Terrone et al.19 recorded cardiac morbidity in 7.6% of a numerous series of women with preeclampsia and HELLP syndrome. In this subgroup of pregnant women, cesarean section predominated as the form of termination of pregnancy, with an increased incidence of low-weight infants, arterial hypertension and laboratory test anomalies. Heart failure and lung edema showed a similar frequency in preeclampsia and HELLP syndrome. Our series presented a slightly higher percentage (9%, 23 cases) of gestosis complicated by heart failure. The latter implies a significantly longer stay in the ICU compared with patients who do not suffer heart failure.
The univariate analysis of the maternal complications only identified prolonged stay in the ICU as predictor, though this may have been due to the presence of complications. Thus, in our case, the multivariate model did not allow us to draw firm conclusions.
The mean duration of stay in our patients was 5days, which coincides with the observations of other authors,8 with no differences among the three diagnostic entities. It seems reasonable to assume that a longer mean stay implies a poorer course and a higher complications rate, and this was effectively found to be the case in our series. As independent predictors of stay in the ICU, the statistical analysis identified hemoglobin concentration and gestational age at delivery; accordingly, a lesser hemoglobin concentration or low gestational week was associated to a longer stay in the ICU, in relation to increased needs for monitorization and treatment. In the series published by Zeeman, longer stay was attributed to the need for temporary mechanical ventilation, blood product transfusions or inotropic drug support.
The association between gestosis and first pregnancy remains the subject of controversy.20,21 In our series, first pregnancy was a frequent factor (62.9%), in coincidence with the observations of other authors21; however, first pregnancy is possibly overestimated as a risk factor for gestosis, since out of fear of suffering preeclampsia again on subsequent occasions, patients may tend to avoid further pregnancies.
A recent metaanalysis22 of 26 studies published between 1966 and 2005 concluded that the risk of preeclampsia is 2.42-fold greater in primiparous women than in multiparous patients—this observation being attributed to differences in immune response between primiparous and multiparous women, in angiogenic profile, or in insulin resistance reactivity pattern.
The research program Pre-eclampsia Integrated Estimate of RiSk (PIERS), created with the purpose of developing a scale serving as a clinical practice and decision-taking guide in cases of maternal risk associated preeclampsia, established that most disease severity criteria show poor performance in predicting maternal-fetal morbidity–mortality. In contrast, standardized assessment and vigilance of patients with severe preeclampsia was seen to reduce maternal risk.23 Accordingly, vigilance and monitorization of these patients in intensive care can allow the early detection of complications, with secondary benefits in relation to mortality.
The limitations of our study are referred to the few conclusions that can be drawn in relation to mortality, due to the few deaths recorded in our series (1.5%), and the lack of specificity of some of the definitions used—such as renal failure—which have changed in recent years, without adaptation to more current classifications such as the RIFLE or the AKIN scale.
In contrast, the positive aspects are the sample size involved—this being one of the largest series of severe gestosis published to date in Spain—and the specialized nature of the care provided (ICU of a third-level hospital, limited exclusively to gynecological-obstetric disease).
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Curiel-Balsera E, et al. Análisis de la morbimortalidad materna de las pacientes con preeclampsia grave, eclampsia y síndrome HELLP que ingresan en una Unidad de Cuidados Intensivos gineco-obstétrica. Med Intensiva. 2011;35:478–83.