SARS-CoV-2 virus (Covid-19) is an infectious disease where most cases have mild symptoms, while few have pneumonia with respiratory failure. Because prone positioning (PP) improves survival in patients with acute respiratory distress syndrome (ARDS), its use has been recommended in Covid-19 patients. PP has shown more homogenous distribution of ventilation and decreasing shunt in dorsal regions and dead space in ventral regions in mechanically ventilated COVID-19 patients. However, the impact of PP in awake patients has not been well defined. Our aim was to perform a meta-analysis to assess the impact of awake prone positioning (APP) on intubation rate, mortality and gas exchange in Covid-19.
A systematic search was performed in MEDLINE, CENTRAL, Web of Science and Lilacs on August 20th, 2021. We used a strategy that combined keywords and descriptors and screened the reference list of all the available articles. Two groups of keywords linked by the Boolean “OR” operator were included. Covid-19; SARCov2, SARSCoV-2; SARS-CoV-2; COVID; novel coronavirus; coronavirus disease; coronavirus-2019 (first group) and prone positioning; awake prone positioning; self-proning; awake prone position; early awake prone; awake proning (second group). Subsequently, both groups were joined by the Boolean operator AND. Only randomized controlled trials (RCTs) that compared the use of APP with usual care in patient with acute respiratory failure due to COVID-19 were included. No language restrictions were imposed. Two authors screened the studies for eligibility (disagreements were resolved by a third author).
We contacted investigators for unreported data. Cochrane Collaboration tool to assess risk of bias was used. The following variables were evaluated: age, sex, setting, interventions (respiratory support, time session of APP) and outcomes. The primary outcome was intubation rate and secondary outcomes were mortality and oxygenation. We combined the studies through a meta-analysis with dichotomous data as risk ratios (RRs) and continuous data as mean differences (MDs). We assessed the variation in the results by drawing a forest plot and statistical heterogeneity through the I2 test at a 95% confidence interval (CI95). According to statistical heterogeneity, fixed-effects model (I2<20%) or a random-effects model (I2≥20%) were used. Analyses were performed with Review Manager version 5.4 (The Cochrane Collaboration, Copenhagen, Denmark). The quality of the evidence was assessed according to GRADE (Grading of Recommendations Assessment, Development, and Evaluation criteria guidelines).
Of the 1041 citations, after discarding the duplicates, we identified 59 potentially relevant studies where 51 studies were discarded and eight RCT were included (Fig. 1 ESM).1–8 The age of the patients ranged between 49 and 66 years (66.7% male).
Four studies were conducted in the ICU,1–3,6 three in the medical ward4,5,8 and one study did not report the setting.7 The largest study was conducted in six countries: France, USA, Canada, Mexico, Spain, Ireland.1 The other studies were carried out in Egypt (one),2 India (two),3,7 Sweden (two)5,6 and USA (two).4,8 The number of participants ranged from 302,4 to 1121.1 APP time varied between 1 and 16h between the studies, and the supplemental oxygen used (high-flow nasal cannula, nonrebreathing mask, nasal cannula and no invasive ventilation) was variable in both groups.
All studies were at high risk of bias due to performance bias (blinding of patients and staff) and most studies did not detail the orotracheal intubation criteria.
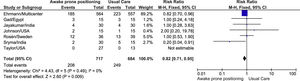
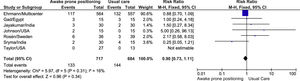
For the meta-analysis, we pooled seven studies because one study did not present outcomes.5 We found significant differences in the intubation rate in favor to the APP group [RR: 0.82 (CI95% 0.71–0.95), I2: 0%, Fig. 1], but no differences in mortality [RR: 0.90 (CI95% 0.73–1.11), I2: 16%, Fig. 2]. Regarding the intubation rate, we performed sensitivity analysis, excluding the study with the greatest weight1 [RR: 0.84 (CI95% 0.52–1.35), I2: 9%, Fig. 2 ESM], where we found that the benefit is not maintained.
Five studies, using different assessment of oxygenation (SaO2/FiO2,1,5,8 SaO22 and ROX index7), describes a positive impact of APP in gas exchange. In turn, two studies (which assessed PaO2/FiO2 ratio) show a decrease in oxygenation.3,4 In the remaining study, oxygenation was not evaluate.6 Due to the different assessments of oxygenation, no meta-analysis was performed.
The quality of the evidence according to GRADE for the outcomes intubation rate and mortality was ranked as very low. We downgrade for risk of bias (performance bias) and imprecision (due to the number of participants and the wide confidence interval).
This study shows a significant decrease in the intubation rate, without a relevant effect on mortality, in Covid-19 patients supported with APP compare to usual care. It should be noted that the quality of the evidence is low in both results. In addition, our sensitivity analysis (excluding the largest study) showed no benefit.
In addition, the current data do not allow us to draw conclusions regarding the benefit in oxygenation, although most studies show an improvement in oxygenation with APP.1,2,5,7,8. Only two studies found no improvement in oxygenation,3,4 where the authors detail it as an unexpected finding, arguing the low adherence to the protocol3 or the late assessment of oxygenation (48 or 72 post APP)4 as possible explanations.
To our knowledge, this is the first meta-analysis showing the benefit of APP in interventional studies. Although four previous reviews found significant decrease in the intubation rate and mortality, those results were obtained through meta-analysis of proportions (without a control group), including observational studies and with considerable statistical heterogeneity.9,10
The main limitations of this metanalysis are: (1) the clinical heterogeneity observed with the intervention in terms of session time and oxygenation supplementation; (2) the lack of additional well designed and large scale RCTs to improve the quality of our findings.
APP seems to be a strategy that is useful and relatively easy to implement in Covid-19 patients with acute respiratory failure. The beneficial effect of APP decreasing the intubation rate could be a great help against the potential shortage of mechanical ventilators in some countries in a new pandemic wave.
Conflict of interestThe authors declare not to have any interest conflicts.