To evaluate the effect of a mindfulness training program on the levels of burnout, mindfulness, empathy and self-compassion among healthcare professionals in an Intensive Care Unit of a tertiary hospital.
DesignA longitudinal study with an intrasubject pre–post intervention design was carried out.
SettingIntensive Care Unit of a tertiary hospital.
ParticipantsA total of 32 subjects (physicians, nurses and nursing assistants) participated in the study.
InterventionA clinical session/workshop was held on the practice of mindfulness and its usefulness. The possibility of following an 8-week training program with specifically designed short guided practices supported by a virtual community based on a WhatsApp group was offered. A weekly proposal in audio and text format and daily reminders with stimulating messages of practice were sent.
Main measurementsVarious psychometric measures were self-reported: burnout (MBI), mindfulness (FFMQ), empathy (Jefferson) and self-compassion (SCS), before and after the training program. Demographic and workplace variables were also compiled.
ResultsAmong the factors affecting burnout, the level of emotional exhaustion decreased (−3.78 points; p=0.012), mindfulness levels measured by the FFMQ were not globally modified, though “observation” and “non-reacting” factors increased. Empathy was not modified, and self-compassion levels increased (3.7 points; p=0.001). Satisfaction and program adherence levels were very high.
ConclusionsIn the population described, this program showed a decrease in emotional exhaustion and an increase in self-compassion — these being factors that can produce well-being and exert a positive impact upon burnout in this vulnerable group.
Evaluar el efecto de un programa de entrenamiento en mindfulness sobre el burnout, el mindfulness, la empatía y la autocompasión en profesionales de la salud de un servicio de medicina intensiva de un hospital terciario.
DiseñoEstudio longitudinal de diseño intrasujeto pre-post intervención.
ÁmbitoServicio de medicina intensiva de un hospital de tercer nivel de referencia.
ParticipantesTreinta y dos participantes (médicos, enfermeras y técnicos auxiliares de enfermería).
IntervenciónSe presentó la intervención en forma de sesión clínica/taller acerca de la práctica de mindfulness y sus utilidades. Se ofreció la posibilidad de seguir un programa de entrenamiento de 8 semanas en prácticas breves guiadas diseñado específicamente y creando una comunidad virtual mediante un grupo de WhatsApp. Se envió una propuesta semanal en formato audio y texto y recordatorios diarios y mensajes estimulantes de la práctica.
Variables principalesSe realizaron distintas mediciones psicométricas mediante autocuestionarios: Burnout (MBI), mindfulness (FFMQ), empatía (Jefferson) y autocompasión (SCS) antes y después del seguimiento del programa y variables sociodemográficas y laborales.
ResultadosEn los factores que inciden sobre el burnout disminuyó el nivel de cansancio emocional (−3,78 puntos, p=0,012). Los niveles de mindfulness mediante FFMQ no se modificaron globalmente, aunque aumentaron los factores «observación» y «ausencia de reactividad». La empatía no se vio modificada y se incrementaron los niveles de autocompasión (3,7 puntos, p=0,001). Los niveles de satisfacción y seguimiento del programa fueron muy altos.
ConclusionesEste programa, en la población descrita, mostró un descenso del cansancio emocional y un aumento de la autocompasión, factores que pueden producir bienestar e incidir en el burnout de este colectivo vulnerable.
Humans spend much of their lives in the working environment, and although ideally the experience should prove satisfactory, this is probably not always the case.
The working environment generates demands upon the individual. Although a degree of stress may be helpful in a given moment to remain more focused on resolving a concrete task, chronic and excessive stress has a devastating effect, with negative consequences when it overwhelms the capacity of the individual to cope with it adequately.
Professional wear or “burnout syndrome” is a normal but undesirable reaction to chronic interpersonal and emotional stress in the working environment.1 It has been described in all professions, and particularly in those characterized by care and assist activities. In this regard, some studies have underscored the risk and relevance of burnout syndrome in the intensive care setting, with prevalences among the professionals that may exceed 50%.2,3 In view of this situation, some American scientific societies in this field have developed a joint official positioning statement reviewing the diagnostic criteria, prevalence, causal factors and consequences of the syndrome, and addressing certain interventions that could be of use in preventing and mitigating it.4–6 Burnout syndrome has an impact both upon the professionals and on their capacity to adequately care and treat their patients.7
In relation to the nursing staff in Intensive Care Units (ICUs), some of the circumstances of their work, such as the perception of not being able to make decisions, collaboration in treatments that prove futile, or acting as mute witnesses of conversations dealing with complex moral decisions, can give rise to symptoms consistent with burnout syndrome. These symptoms are currently recognized as a consequence of additional psychosocial disorders such as moral distress (the sensation that appropriate care is not being provided) and compassion fatigue,8 which can also affect patient care and even lead to abandonment of the workplace. A number of measures for dealing with this kind of situation have been evaluated, with promising results.9,10
Considering the above, it is necessary to adopt strategies designed to improve the work environment. Such measures in first place should address the working conditions (rest periods, burdens, remuneration, healthy environment). However, it is also important to develop individual coping skills (resilience, cognitive flexibility and self-awareness) in the face of stressing conditions that cause uncertainty and have a strong emotional impact, and which are experienced on a daily basis in Units of this kind.
In this context, it would be desirable for organizations to be more inclined to incorporate initiatives seeking to develop internal resources (coping skills) among their professionals and thus contribute to promote more mentally healthy environments. Training in “mindfulness” as a personal wellbeing tool that has demonstrated its efficacy in the clinical setting,11 is seen as a means by which to achieve this objective in the workplace. A considerable number of publications can be found on its use and effects in relation to professional activity.12–14 Certain corporations, such as Google, the Mayo Clinic and the United States Army, have described the introduction of training in mindfulness among their professionals with the aim of improving both their wellbeing and professional performance.15 A whole country (in this case the United Kingdom) has adopted the parliamentary initiative for introducing mindfulness in different spheres, starting with the occupational setting (Mindful at Work), in the context of a broader national strategy (Mindful-Nation-UK). (http://www.themindfulnessinitiative.org.uk/).
In Intensive Care Medicine, some experiences have been published regarding the effectiveness of mindfulness programs in application to biological and psychological stress parameters among professionals in the ICU.16–18
What is mindfulness? The term is associated with a Buddhist tradition, and was used in 1881 for the English translation of the Hindu Pali word “sati” — a polysemic term that includes the concepts of attention, comprehension and recall, and which refers to a Buddhist instruction as a means for knowledge. However, since the mid-1980s, these practices have been combined with elements of modern psychology and have been developed as a secular training, unrelated to Buddhism, that is the subject of scientific research.19 In this respect, mindfulness is regarded as the capacity allowing humans to focus attention on the experience of the present moment (both internally and in relation to the environment) with openness, curiosity, acceptance and kindness.20 In this manner it can also be understood as a metacognitive skill, a trait or attitude that we may choose to develop. The term is likewise used in reference to practices for developing this skill. These practices have been structured in specific programs that have demonstrated their efficacy in clinical settings for the control of stress — Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT) — and for the prevention of major depression relapse.21
No standardized mindfulness training models are available in the workplace setting, and strategies characterized by variable durations and designs have been applied. Most initiatives comprise 8-week physical presence interventions involving sessions of variable duration. In addition to an important theoretical psychoeducational content referred to stress and emotions, these interventions are implemented on a group basis, dedicating time to the exchange of experiences and encouraging the subjects to conduct daily personal practices, with the supply of different materials.16,17,22 All this seeks to develop consciousness of the personal feelings, emotions and physiological reactions experienced in daily life. The arguments in favor of their utilization are the documented positive effects upon psychological functions such as attention (by incrementing attentional efficiency, stability and control), cognition (by increasing creativity and cognitive flexibility), emotions (by reducing reactivity and boosting positive emotional tone) and behavior (by reducing automaticity and incrementing self-regulation), and physiological variables (by reducing the response to stress).13,23,24
In general terms, it may be affirmed that programs based on mindfulness result in modifications in participant attitude toward personal thoughts, sensations and emotions, as psychological changes that appear to have neuroanatomical correlates.25,26
In the healthcare setting, the application of such programs would extend beyond the individual context of the professional, strengthening skills that are crucial for the therapeutic relationship.27–29 A number of experiences have been carried out in Spain, fundamentally in the primary care setting.13,14,30 There have been few such initiatives in Intensive Care Medicine,31 though some exceptions can be cited.18
In the context of Intensive Care Medicine, which is characterized by great emotional intensity and very particular working characteristics, training initiatives of this kind must be considered on an adapted basis. The great rotation of professionals, non-fixed work shifts, working on holidays, long duties for the medical staff and strong continuous training demands referred to technical skills, all imply that any new intervention must be carefully thought out in order to adapt it to this special setting.
The present study was carried out to evaluate the effects upon burnout levels, mindfulness, empathy and self-compassion, as well as the applicability and satisfaction, of a specifically designed brief mindfulness practices program, using digital supporting tools, targeted to the healthcare professionals of a Department of Intensive Care Medicine (DICM) belonging to a tertiary hospital.
Participants and methodsA longitudinal study with an intrasubject pre–post intervention design was carried out in the medical-surgical Department of Intensive Care Medicine of a reference tertiary hospital. With a capacity of up to 40 beds, the Department has a staff of 26 physicians (working from 8:00a.m. to 5:00p.m., with some serving as reinforcement on duty shifts) and 15 residents in training in Intensive Care Medicine. The nursing staff in turn comprises about 80 nurses and 50 nursing assistants (distributed in two shifts of 12 daytime hours and two nighttime shifts, working on alternate days). The Department also has 6 orderlies and three administrative staff members.
A clinical session was held with all the physicians and with a nursing and nursing assistant daytime shift, with the participation of a total of 53 professionals. Of these, 21 were physicians (39.6%), 17 were nurses (32.1%), 14 were nursing assistants (NAs) and one was an orderly (1.9%). The session was used to explain the practice of mindfulness, its principles, usefulness and scientific evidence, and two brief practices were carried out. The professionals were offered to participate in a study on the effect of a mindfulness training program for 8 weeks, involving brief practices. A total of 32 professionals voluntarily agreed to participate: 8 physicians (25.0%), 13 nurses (40.6%) and 11 nursing assistants (34.4%).
Evaluation instruments and measuresThe variables were compiled using the following questionnaires:
- -
Sociodemographic and occupational data. Age (≤35/36–50/>50 years of age); gender; marital status (single/couple); number of offspring; professional category (physician/nurse/NA); years working in intensive care (<5/5–15/>15 years); experience in mindfulness/meditation (yes/no).
- -
Maslach Burnout Inventory—Human Service Survey (MBI-HS). Burnout was measured with the validated Spanish version of the MBI-HS.32 This is a psychological evaluation instrument comprising a series of items referred to the thoughts and feeling of an individual in relation to his or her work. It measures three dimensions of the syndrome: emotional exhaustion (EE), which refers to the loss of emotional resources in the face of work, with a maximum of 54 points; depersonalization (DP), which describes a cold or insensitive response to people whom attention is being paid to, with a maximum of 30 points; and personal achievement (PA), which describes feelings of competence and efficacy at work, with a maximum score of 48. There are no cut-off points for defining the presence or absence of burnout, but the syndrome is defined by high emotional exhaustion and depersonalization scores, and low personal achievement scores.
- -
Five Facets of Mindfulness Questionnaire (FFMQ), validated in Spanish.33 This instrument measures the general tendency to proceed with full attention in daily activity, based on 5 skills or factors: “Observation”, which refers to the capacity to observe and attend internal and external experiences, whether sensations, emotions or thoughts; “Description”, which refers to labeling experiences with words; “Acting with awareness”, which describes the capacity to consciously focalize attention on each activity, as opposed to acting mechanically; “Non-judging of inner experience”, which explores non-evaluative or judging position-taking with respect to present experiences; and “Non-reactivity to inner experience”, which refers to the tendency to allow feelings and emotions to flow, without becoming trapped by them or rejecting them. Higher scores indicate greater full awareness, full attention or mindfulness.
- -
Jefferson Empathy Scale, validated in Spanish.34 This instrument measures empathy orientation, defined as the capacity to put oneself in the place of others. The higher the score (from 20 to 140 points), the greater the empathy.
- -
Self-Compassion Scale (SCS), in its short 12-item version validated in Spanish.35 This instrument measures how the individual tends to respond to himself or herself in difficult moments. It explores skills seeking to allow empathic understanding of ourselves in the face of failure or when we feel inadequate, instead of resorting to self-criticism or punishment. It comprises three main subscales: self-kindness (understood as warmth toward oneself); common or shared humanity (recognizing that suffering and difficulties do not only happen to us but form a common and inevitable part of human experience, avoiding feelings of isolation and self-commiseration); and mindfulness (which in this subscale refers to a concept close to decentering, as the capacity to experience painful thoughts and emotions in a balanced manner without over-identification of oneself or trying to avoid or deny them).
A clinical session was used to explain the practice of mindfulness, its principles, usefulness and scientific evidence, and two brief practices were carried out. The data compilation questionnaires and psychometric tests were previously distributed among the participants, guaranteeing anonymity and confidentiality.
At the end of the session the participants expressed their wish to participate or not in the 8-week training program. Those who agreed to participate were required to form part of a WhatsApp group and to receive information via e-mail.
The intervention program consisted of short (5–8min) practices in the course of 8 weeks. The initial clinical session and conduction of the practices were carried out by a physician of the Department holding a Master in Mindfulness, Meditation and Relaxation from the University of Barcelona (Spain). On Monday of each week, the participants received a text file via WhatsApp, explaining the exercise, and an audio file that could be used for guided meditation. A practice guide was provided to record participation as a self-reporting method. Each day the participants received a practice reminding message in the form of a motivating phrase, image or video, referred to the subject to be treated during that week.
The program was designed to allow individual training, choosing the best moment and encouraging the participants to perform the exercise at least once a day. No group practices were formally contemplated. Doubts or queries were resolved informally, since the instructor was a staff member of the Department. Meetings for joint practices proved occasionally possible.
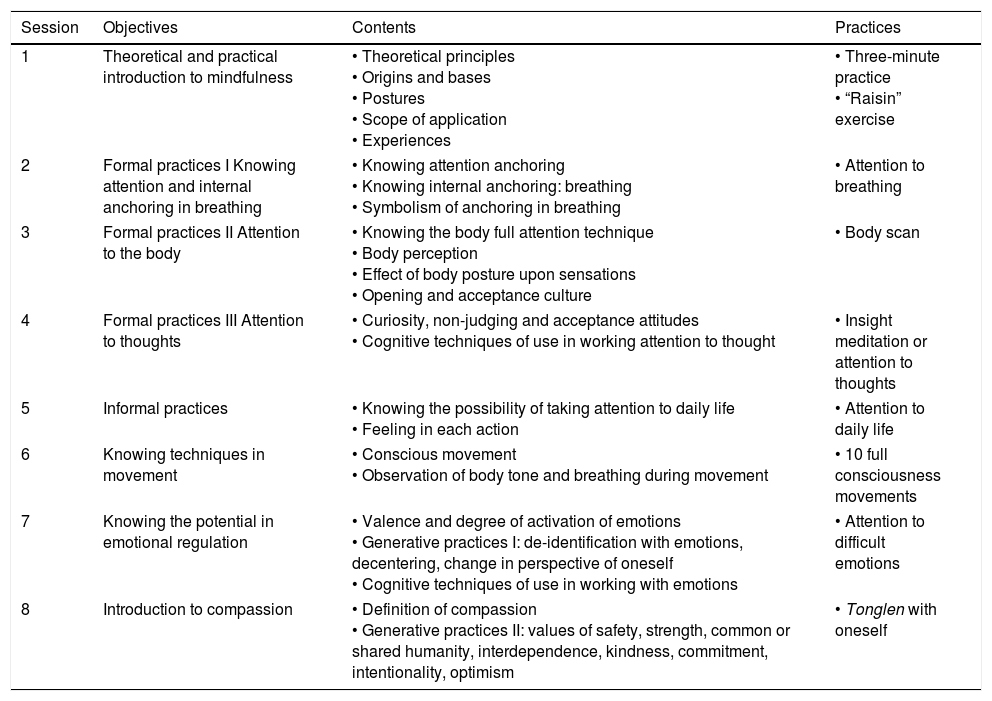
The practices proposed in the different sessions are detailed in Table 1.
Program structure and contents.
| Session | Objectives | Contents | Practices |
|---|---|---|---|
| 1 | Theoretical and practical introduction to mindfulness | • Theoretical principles • Origins and bases • Postures • Scope of application • Experiences | • Three-minute practice • “Raisin” exercise |
| 2 | Formal practices I Knowing attention and internal anchoring in breathing | • Knowing attention anchoring • Knowing internal anchoring: breathing • Symbolism of anchoring in breathing | • Attention to breathing |
| 3 | Formal practices II Attention to the body | • Knowing the body full attention technique • Body perception • Effect of body posture upon sensations • Opening and acceptance culture | • Body scan |
| 4 | Formal practices III Attention to thoughts | • Curiosity, non-judging and acceptance attitudes • Cognitive techniques of use in working attention to thought | • Insight meditation or attention to thoughts |
| 5 | Informal practices | • Knowing the possibility of taking attention to daily life • Feeling in each action | • Attention to daily life |
| 6 | Knowing techniques in movement | • Conscious movement • Observation of body tone and breathing during movement | • 10 full consciousness movements |
| 7 | Knowing the potential in emotional regulation | • Valence and degree of activation of emotions • Generative practices I: de-identification with emotions, decentering, change in perspective of oneself • Cognitive techniques of use in working with emotions | • Attention to difficult emotions |
| 8 | Introduction to compassion | • Definition of compassion • Generative practices II: values of safety, strength, common or shared humanity, interdependence, kindness, commitment, intentionality, optimism | • Tonglen with oneself |
The sample description was based on the categorical and quantitative demographic and occupational parameters. Categorical variables were reported as absolute frequencies and proportions, while quantitative variables were reported as the median and percentiles 25–75. These variables and the results of the questionnaires were stratified by groups according to whether the program was completed or not. Statistically significant differences between results were explored.
The questionnaires were again administered after the end of the program. An intrasubject pre–post intervention analysis was made of the magnitude of change in measures. In view of the size of the sample, normal data distribution was assumed, with application of the Student t-test and Fisher exact test, and calculation of the difference of means, confidence interval and degree of statistical significance. For each subgroup of the variable “professional category”, we performed a pre–post intervention analysis of the difference in intrasubject questionnaire results. The nonparametric Wilcoxon test was used in view of the small size of the subgroups.
Statistically significant differences were defined with a 95% confidence interval when not including the value 0, and with a level of significance of p≤0.05.
The IBM SPSS version 20 and STATA version 14 statistical packages were used throughout.
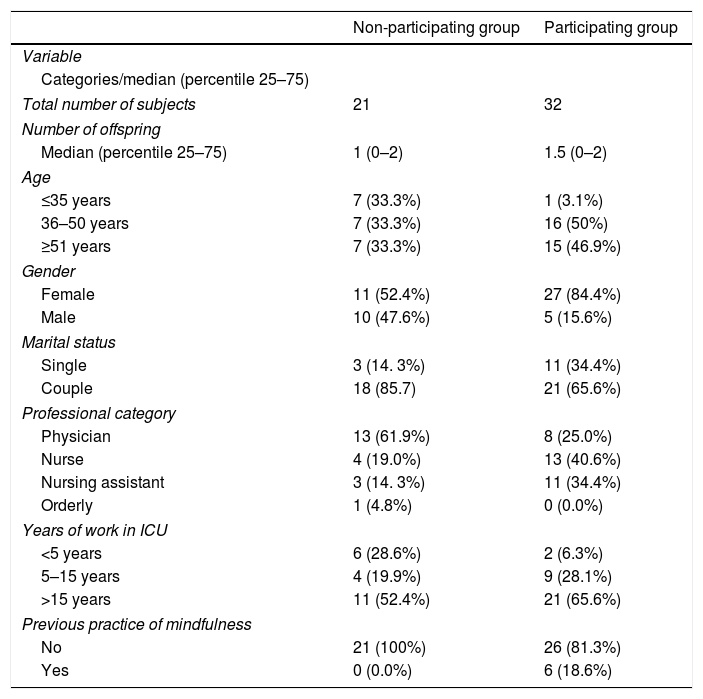
ResultsTable 2 describes the sociodemographic and occupational characteristics of the participants and non-participants.
Sociodemographic and occupational characteristics of the participants and non-participants.
| Non-participating group | Participating group | |
|---|---|---|
| Variable | ||
| Categories/median (percentile 25–75) | ||
| Total number of subjects | 21 | 32 |
| Number of offspring | ||
| Median (percentile 25–75) | 1 (0–2) | 1.5 (0–2) |
| Age | ||
| ≤35 years | 7 (33.3%) | 1 (3.1%) |
| 36–50 years | 7 (33.3%) | 16 (50%) |
| ≥51 years | 7 (33.3%) | 15 (46.9%) |
| Gender | ||
| Female | 11 (52.4%) | 27 (84.4%) |
| Male | 10 (47.6%) | 5 (15.6%) |
| Marital status | ||
| Single | 3 (14. 3%) | 11 (34.4%) |
| Couple | 18 (85.7) | 21 (65.6%) |
| Professional category | ||
| Physician | 13 (61.9%) | 8 (25.0%) |
| Nurse | 4 (19.0%) | 13 (40.6%) |
| Nursing assistant | 3 (14. 3%) | 11 (34.4%) |
| Orderly | 1 (4.8%) | 0 (0.0%) |
| Years of work in ICU | ||
| <5 years | 6 (28.6%) | 2 (6.3%) |
| 5–15 years | 4 (19.9%) | 9 (28.1%) |
| >15 years | 11 (52.4%) | 21 (65.6%) |
| Previous practice of mindfulness | ||
| No | 21 (100%) | 26 (81.3%) |
| Yes | 0 (0.0%) | 6 (18.6%) |
Most of the participants were women (84.4%); 96.9% were over 35 years old; 64.5% lived as a couple with a median of 1.5 offspring; and 65.6% had been working in intensive care for over 15 years. The sample distribution according to professional category was: nurses 40.6%, nursing assistants 34.4% and physicians 25.0%. The majority (81.3%) claimed to have no prior experience with mindfulness. In this respect, “prior experience” was understood as having heard about the concept of mindfulness. None of the subjects had practiced mindfulness before.
The 21 subjects that declined to participate were predominantly over 35 years of age (66.6%); 52.4% were women; 85.7% lived as a couple; 61.9% were physicians; and 28.6% had been working in intensive care for less than 5 years. None of them reported any prior experience with mindfulness.
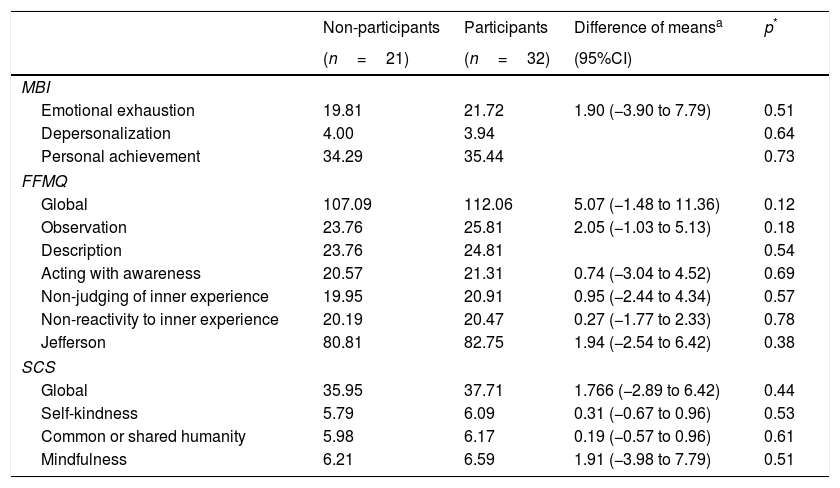
Table 3 shows the questionnaire scores stratified between participants and non-participants in the mindfulness program.
Summary of initial (baseline) scores of the different questionnaires and their sub-factors between participants and non-participants.
| Non-participants | Participants | Difference of meansa | p* | |
|---|---|---|---|---|
| (n=21) | (n=32) | (95%CI) | ||
| MBI | ||||
| Emotional exhaustion | 19.81 | 21.72 | 1.90 (−3.90 to 7.79) | 0.51 |
| Depersonalization | 4.00 | 3.94 | 0.64 | |
| Personal achievement | 34.29 | 35.44 | 0.73 | |
| FFMQ | ||||
| Global | 107.09 | 112.06 | 5.07 (−1.48 to 11.36) | 0.12 |
| Observation | 23.76 | 25.81 | 2.05 (−1.03 to 5.13) | 0.18 |
| Description | 23.76 | 24.81 | 0.54 | |
| Acting with awareness | 20.57 | 21.31 | 0.74 (−3.04 to 4.52) | 0.69 |
| Non-judging of inner experience | 19.95 | 20.91 | 0.95 (−2.44 to 4.34) | 0.57 |
| Non-reactivity to inner experience | 20.19 | 20.47 | 0.27 (−1.77 to 2.33) | 0.78 |
| Jefferson | 80.81 | 82.75 | 1.94 (−2.54 to 6.42) | 0.38 |
| SCS | ||||
| Global | 35.95 | 37.71 | 1.766 (−2.89 to 6.42) | 0.44 |
| Self-kindness | 5.79 | 6.09 | 0.31 (−0.67 to 0.96) | 0.53 |
| Common or shared humanity | 5.98 | 6.17 | 0.19 (−0.57 to 0.96) | 0.61 |
| Mindfulness | 6.21 | 6.59 | 1.91 (−3.98 to 7.79) | 0.51 |
FFMQ: Five Facets Mindfulness Questionnaire; Jefferson: Empathy Scale; MBI: Maslach Burnout Inventory; SCS: Self-Compassion Scale.
There were no significant differences in any of the questionnaires or in any of the sub-factors of the psychometric variables between the participants and non-participants.
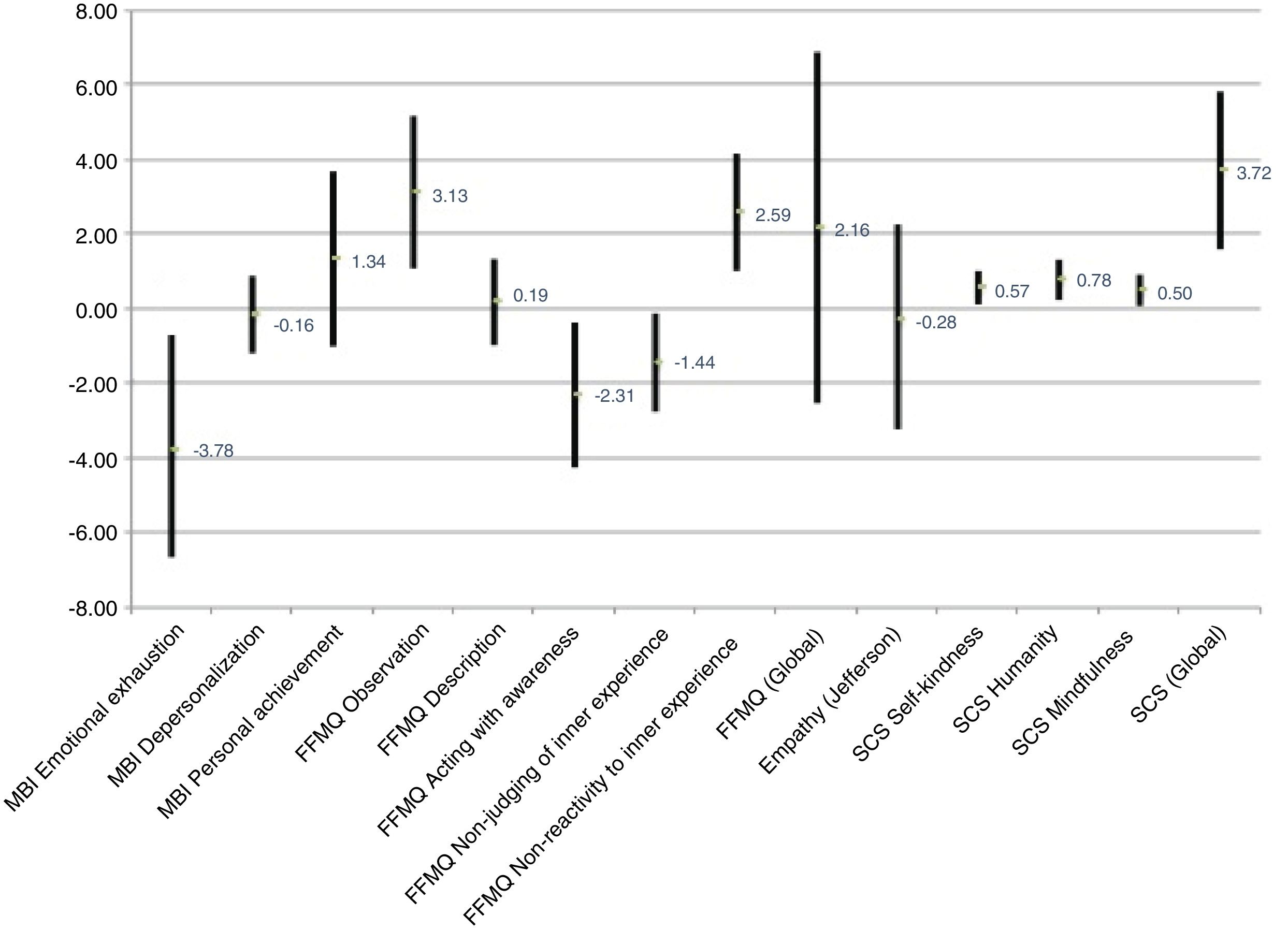
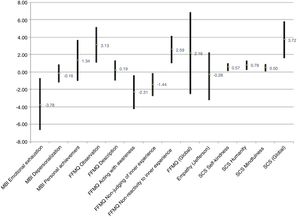
Fig. 1 shows the pre–post program differences of the means corresponding to the scores of the questionnaires and the 95% confidence interval (95%CI).
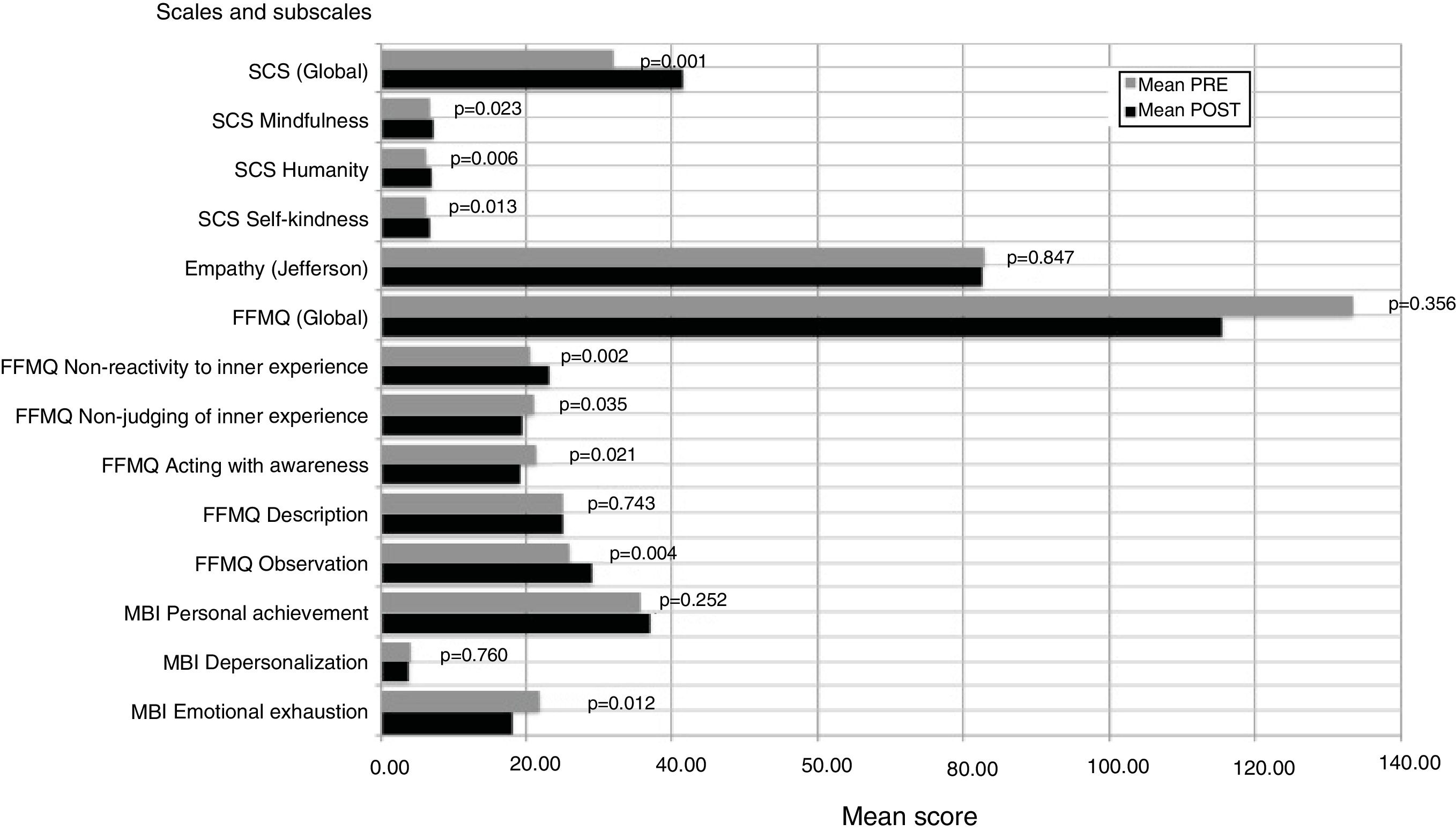
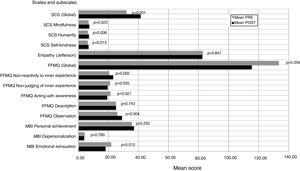
Fig. 2 in turn shows the mean scores of the different questionnaires applied before and after the intervention, with the statistical significances of the differences between them.
The results of the MBI-HS, which assesses burnout based on three dimensions of the syndrome (emotional exhaustion, depersonalization and personal achievement), differed according to the dimension considered. Following the intervention, a positive effect was observed in relation to “emotional exhaustion” for the global subjects (difference in mean −3.78 points). In the case of the dimension “personal achievement”, the positive effect only reached statistical significance among the physicians.
The assessment of mindfulness, or full attention, based on the FFMQ showed no global pre–post program modifications. However, on separately analyzing the different subscales, four of the five facets of the FFMQ did show significant variations following the intervention. No significant global changes were observed because the variations of the individual facets were of opposite sign. In effect, the scores corresponding to “Observation” and “Non-reactivity to inner experience” were seen to increase, while those corresponding to “Acting with awareness” and “Non-judging of inner experience” decreased.
The Jefferson Empathy Scale showed no significant global changes as a result of the program.
The global scores of the Self-Compassion Scale were seen to increase significantly as a result of the intervention. Although on average all the professional categories showed an increase in self-compassion, statistical significance was only reached among the physicians. The separate analysis of the three main subscales also revealed a significant post-program increase. The factor with the greatest increase was “common or shared humanity”. In terms of the professional categories, the physicians showed a significant increase in the score corresponding to “self-compassion/self-kindness” and “common or shared humanity”, while the nursing assistants showed a significant increase in “mindfulness”.
DiscussionProfessionals involved in areas of high-intensity care such as the ICU may be particularly vulnerable to burnout, and the strategies used to deal with the problem must be adapted to the peculiarities of work in this environment, without consuming too much time in continuous or ongoing training or in terms of working hours lost. The initiative must be adapted to the great rotation of professionals, variable resting periods and long duties characterizing this particular occupational scenario. Furthermore, such a proposal offered from the workplace should not be experienced as something that reduces off-work resting time. The present study describes the first reported intervention of this kind in a medical-surgical ICU of a reference tertiary university hospital with a very large staff, adapted to all the professional categories, and generating a program practice community on a virtual basis (WhatsApp group).
Mindfulness programs are usually physical presence interventions involving group sessions with a duration of about 2.5h. They are also characterized by a significant psychoeducational content referred to stress and emotions. The novelty of our program is that it has little physical presence activity and few joint practices, scarce theoretical psychoeducational content, and offers complete flexibility for the participants in performing the practices. The proposed practices over a period of 8 weeks were relatively brief. However, vehiculization of the proposals and reminders through the creation of a WhatsApp group generated a virtual community in which the participants could share their mindfulness experiences with each other and with the instructor (one of the Department staff members). The participants were very satisfied with this program format, its design and duration, and with the proposals and quality of the materials, and most of them expressed a desire to further their training in mindfulness, with the purpose of applying it to both their personal and professional lives. Although the classical format establishes a duration of 8 weeks, it is becoming apparent that shorter interventions may prove equally effective in nonclinical contexts.24 In our particular work setting it would be interesting to evaluate such briefer initiatives in future to see whether the same results can be obtained. On the other hand, the generative practices (working with difficult emotions and self-compassion) were seen to pose the greatest difficulties. This may be because these concepts are not so well known and must be addressed more in depth before these practices are started. Ways to address this issue need to be explored in future.
The participants were predominantly women, as would be expected from the strong female presence in the nursing and nursing assistant professions. Of note is the lack of participation on the part of the younger members of the Department. The concrete reasons for this are not clear. Nevertheless, there were no significant differences in the psychometric parameters between those who decided to participate in the program and those who did not.
The results of this research study supports the applicability of mindfulness as a strategy for reducing those factors that can influence the development of burnout in healthcare professionals,13,14,30 and also in the concrete field of Intensive Care Medicine.18,31 Although the prior burnout rates in our population were low (moderate emotional exhaustion, very low depersonalization and moderate personal achievement), the emotional exhaustion scores were seen to decrease after the intervention.
On the other hand, brief practices have been used to develop a strategy that appears to be promising, and which has already produced evidence of benefit in healthcare professionals.36
In relation to the effects of the program upon the variables referred to burnout, the factor seen to experience statistically significant improvement as a result of the program was emotional exhaustion in the global participants. This observation is consistent with the data found in the literature, where emotional exhaustion is regarded as the core dimension of burnout syndrome.37 The emotional exhaustion levels were moderate at baseline and were seen to decrease after the intervention. Of note in our population is the fact that depersonalization was already very low at baseline, and consequently implementation of the program was unlikely to improve this parameter any further. On the other hand, the personal achievement levels were intermediate.
Our program had no effect upon the levels of mindfulness as measured with the FFMQ. There were significant variations in four of the five facets of this instrument, but the fact that the variations were of opposite sign implied that there were no significant global changes as a result of the intervention. Specifically, the scores corresponding to “Observation” and “Non-reactivity to inner experience” were seen to clearly increase, while those corresponding to “Acting with awareness” and “Non-judging of inner experience” decreased. We postulate that a program of this kind may produce an “awareness effect” referred to personal ways of acting, thereby making it easier to detect moments in which less attention is being paid, while “non-judging” proves more difficult. This aspect of our pilot study should be considered and explained in the initial instructions and in the different practices.
No effect upon empathy was observed. A possible explanation for this may be the measuring scale itself, though the previous empathy levels in our study sample were most likely already high. This is consistent with the observations of Amutio et al.23 and Galantino et al.,38 who likewise found no significant differences in the variable empathy among healthcare professionals after 8 weeks of training.
However, we did detect an impact upon self-compassion, which showed a significant increase, in concordance with the observations of Demarzo et al.24
The described intervention could influence emotional exhaustion and its repercussions upon the stress to which these professionals are susceptible.39 Our study demonstrates the usefulness of practicing mindfulness among ICU professionals, particularly as regards the reduction of emotional exhaustion and increase in self-compassion. It would be interesting for future studies to investigate whether the increase in self-compassion can act as a mediating factor of the positive effects of mindfulness upon emotional exhaustion, and to explore the possible undesirable effects of these interventions.40
Our study has some limitations. Its empirical validity is limited by the lack of a control group. Furthermore, since the participants constituted an incidental group, some bias was introduced by their interest in the study subject — with some participants already knowing things about the practices before they were actually carried out.
Nevertheless, in global terms, the psychometric tests performed showed no significant baseline differences between the participants and the non-participants. On the other hand, since the practices were not recorded, we cannot rate commitment on the part of the participants. On an informal basis, two-thirds of them claimed to have largely followed the practices as proposed. However, we were unable to quantify dedication, which is a significant conditioning factor of the effectiveness of the intervention.41
The impact which this intervention may have over the long term is not clear, though it is encouraging that the program encouraged the participants to learn more and practice mindfulness. Given the mentioned limitations, future randomized controlled studies with larger sample sizes are needed.
ConclusionsA brief and personal practice-based mindfulness training program supported by the creation of a WhatsApp virtual community group among healthcare professionals belonging to a Department of Intensive Care Medicine has demonstrated psychological and cognitive effects that may afford wellbeing and have an impact upon burnout by reducing emotional exhaustion and incrementing self-compassion. All this in turn may result in improved quality patient care.
AuthorshipThe contributions of the authors were as follows:
- •
Study conception and design: R.M. Gracia, J.M. Ferrer.
- •
Data compilation, analysis and interpretation: R.M. Gracia, J.M. Ferrer, A. Ayora, M. Alonso.
- •
Drafting of the manuscript: R.M. Gracia, J.M. Ferrer, M. Alonso.
- •
Critical review of important parts of the intellectual content: R.M. Gracia, J.M. Ferrer, A. Ayora, M. Alonso, A. Amutio, R. Ferrer.
- •
Approval of the final manuscript version for publication: R.M. Gracia, J.M. Ferrer, A. Ayora, M. Alonso, A. Amutio, R. Ferrer.
The authors declare that they have no conflicts of interest.
The authors wish to express their sincere gratitude to the colleagues of the Department of Intensive Care Medicine of Vall d’Hebron Hospital (Barcelona, Spain) for sharing this experience and making it possible for the study to be carried out.
Please cite this article as: Gracia Gozalo RM, Ferrer Tarrés JM, Ayora Ayora A, Alonso Herrero M, Amutio Kareaga A, Ferrer Roca R. Aplicación de un programa de mindfulness en profesionales de un servicio de medicina intensiva. Efecto sobre el burnout, la empatía y la autocompasión. Med Intensiva. 2019;43:207–216.