To analyze the difference between the degree of importance and satisfaction of the needs of family members of patients in an Intensive Care Unit (ICU).
DesignA descriptive, cross-sectional analytical study was carried out.
SettingMedical – surgical ICU of a university hospital in Chile.
ParticipantsFamily members of critical patients with a length of stay of ≥48h, over 18 years of age, and with at least one visit to the patient.
Variables of interestThe Critical Care Family Needs Inventory questionnaire was used to determine the difference between the degree of importance and satisfaction of the needs of the family members. In addition, the needs were classified according to the categories proposed by importance – performance analysis (IPA).
ResultsA total of 253 family members were recruited, observing a negative gap (satisfaction<importance) in 100% of communication needs and in 51.9% of support needs. In turn, 8.9% of the needs were priority needs according to the IPA, including assistance with financial problems, contact in case of changes in the patient condition, talk about the possibility of death, and the reception of guidance at the patient bedside.
ConclusionsA high level of importance, compared to low levels of satisfaction, determines a negative gap in most of the needs of the family of the critical patient, particularly those referred to communication. Despite this, a low proportion of the needs should be addressed on a priority basis.
Analizar la diferencia entre el grado de importancia y satisfacción de las necesidades de los familiares de pacientes en una unidad de cuidados intensivos (UCI).
DiseñoEstudio descriptivo de corte transversal, analítico.
ÁmbitoUCI médico-quirúrgica de un hospital universitario en Chile.
ParticipantesFamiliares de pacientes críticos con estancia igual o superior a 48 horas, mayores de 18 años y con al menos una visita al paciente.
Variables de interésSe utilizó el cuestionario Critical Care Family Needs Inventory para determinar la diferencia entre el grado de importancia y satisfacción de las necesidades de los familiares. Además, se clasificaron las necesidades según las categorías propuestas por el análisis de importancia-rendimiento (AIR).
ResultadosUn total de 253 familiares fueron reclutados, observándose una diferencia negativa (satisfacción<importancia) en el 100% de las necesidades de comunicación y en un 51,9% de las de apoyo. Un 8,9% de las necesidades resultaron prioritarias según el AIR, incluyendo la ayuda con problemas financieros, el contacto en caso de cambios en la condición del paciente, hablar sobre la posibilidad de fallecimiento y orientaciones al lado de la cama del paciente.
ConclusionesUn alto nivel de importancia, en comparación con bajos niveles de satisfacción, determina una diferencia negativa en la mayoría de las necesidades de la familia del paciente crítico, particularmente en las de comunicación. A pesar de esto, una baja proporción de las necesidades deberían ser atendidas de manera prioritaria.
Hospitalization in an Intensive Care Unit (ICU) is a stressing experience not only for the patient, but also for the family. The psycho-social impact that the ICU stay causes due to the vital risk of the family member hospitalized and other potential sources of stress affect the families: a highly technological environment, life support therapies, and the way the healthcare team interacts affects them.1,2 In this setting, the medical literature describes that critically ill patients’ families have specific needs during the ICU stay,3,4 in a more holistic view of the patient and the family, where both are the target of the healthcare that is being provided.5,6 Over the last decade, numerous studies have been published on family needs in the ICU setting being the safety and information needs the most important of all.7
Although it is important to know the needs of the family members,8,9 the medical literature tells us that the healthcare team does not always make an accurate identification of these needs and even when they do, they do not give them the importance they deserve.10 In this sense, Maxwell et al. (2007) revealed that the family members attributed more importance to their needs than nurses did – especially information needs.11 This situation is seen again in other needs such as emotional needs12 and all this translates into healthcare that does not meet the expectations from the family and negatively impacts their satisfaction.
From the healthcare perspective, the user's satisfaction is a priority for the healthcare institutions since it lets us know, first hand, the experience that the individual had with the healthcare received.13 However, at the ICU setting, evaluating this is a little different compared to other clinical units since most patients cannot communicate themselves verbally or give their opinion on the healthcare received. Thus, it is usually the family that has to assess the care, treatment, and attention received14 by their loved ones at the ICU team.
Also, the user's satisfaction is associated with an improved quality in the healthcare received and it depends on the match (or difference) between prior expectations and the perception of the healthcare being received.15 This requires exploring the user's needs16 to determine the difference between the level of importance and the satisfaction of the family needs at the ICU in order to categorize the various needs families have. One of the methods described to analyze the difference between importance and satisfaction of a series of attributes is the importance-performance analysis (IPA).17 Using the IPA methodology in the context of the needs from patients’ families, at the ICU setting, will help the healthcare team identify priority needs and implement interventions when necessary and in a timely manner. The goal of this study was to analyze the difference between the level of importance and the level of satisfaction of the family needs of patients admitted to a teaching hospital ICU.
Patients and methodsDesignDescriptive, cross-sectional, analytical study conducted between the months of January and June 2017 in a closed polyvalent ICU of a teaching hospital located in Santiago, Chile. This ICU has 32 beds of medium and high complexity and receives patients from all other specialties, except for severely burned patients and patients with heart conditions. Beds are distributed in individual examination rooms without an independent-visit pattern. When it comes to the healthcare team, the unit has an intensivist 24/7 being the nurse/patient ratio, 1:2 to 1:3.
The ICU visiting policy is 7 days a week from 13:00 through 19:00h. However, based on the family specific requirements, this may vary. The intensivist is the person in charge of reporting to the family on various issues concerning the patient's condition. The nurses interact with the family periodically and provide them with general information on the patient.
The sample included two family members per patient hospitalized in the ICU and the following inclusion criteria had to be met: be over 18, having visited the patient in the ICU, at least once, and ICU stays ≥48h. Exclusion criteria were ICU stays over 7 days and patients who had just been transferred to less complex units when they were invited to participate in this study.
The size of the sample was determined using the G*Power software (version 3.1.9.2; Institute of Experimental Psychology, Dusseldorf, Germany), considering an effect size of 0.2, an alpha error probability of 5% and a power of 95%, which determined a minimum of 252 family members recruited using a non-probabilistic sample. Family members were contacted on the phone individually during the ICU visiting hours or while at the waiting room by an assistant researcher external to the ICU team and they were invited to give personal answers to the questionnaires in a room for that purpose.
Tools for data miningFor data mining purposes, one questionnaire of sociodemographic characterization was used that collected all the variables relative to both the family member and the patient such as sex, age, civil status, relation to the patient, educational level, prior experience at the ICU, length of the ICU stay, and participation in the decision-making process. Additionally, the Critical Care Family Needs Inventory (CCFNI) in its Chilean Spanish version was used18 to determine the level of importance and satisfaction of the family needs. The CCFNI was created by Molterand Leske19 and it includes 45 needs with Likert-type scale responses from 1 to 4 grouped in 2 dimensions: communication and support. In order to assess the importance of the family needs, the following question was asked: “How important is each and every single one of the following needs to you?” the responses were ranked in the Likert scale from 1 (unimportant) to 4 (very important). Thus, to be able to determine the level of satisfaction, the following question was asked: “to what extent have every single one of these needs been satisfied?” being the responses ranked in the Likert scale from 1 (unsatisfactory) to 4 (very satisfactory). This adaptation from the original CCFNI scale has been used in other researches with similar purposes by other authors.20,21
The Chilean Spanish version of the CCFNI reported adequate reliability (α=0.93), communication (α=0.93) and support (α=0.87).18
Statistical analysisThe sociodemographic variables were distributed using frequency tables and percentages as needed. The importance of family needs, their level of satisfaction and the dimensions of the CCFNI were analyzed using descriptive statistics (mean). The degree of difference between the importance and satisfaction of the needs was obtained by estimating the difference between the mean of satisfaction and the mean of importance for every need and dimension of the CCFNI. Needs with negative difference were defined as those where the result of this difference was <0 (satisfaction<importance) while needs with positive difference were defined as those where the result of this difference was >0 (satisfaction>importance).
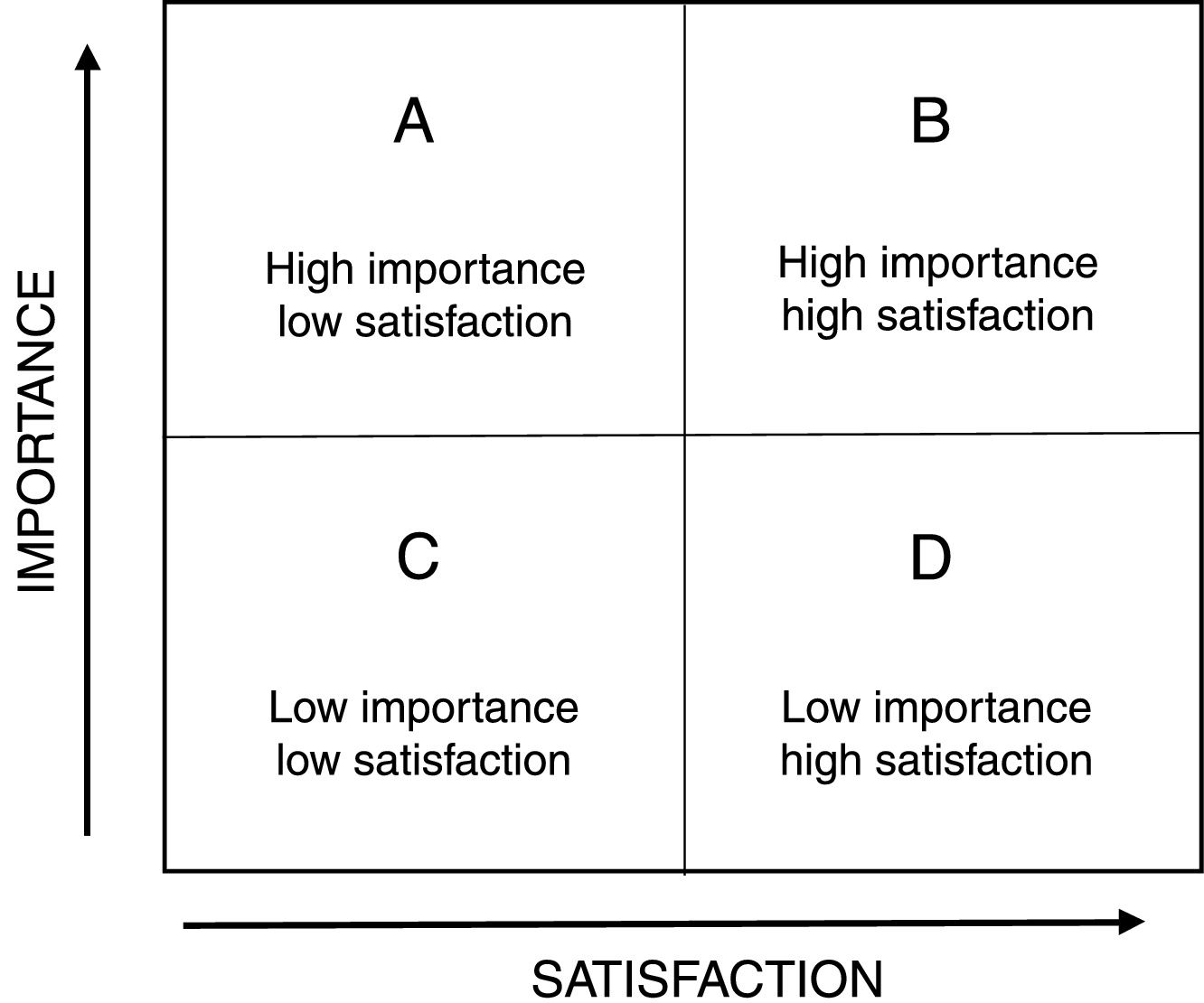
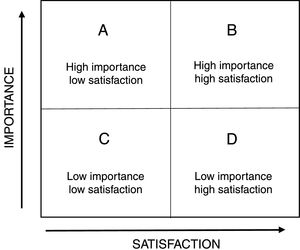
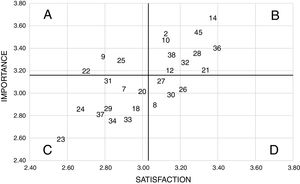
On the other hand, the IPA methodology created by Martilla and James was used, who consider, in addition to the analysis of differences, the making of a graphic matrix in which the attributes are distributed into 4 categories, each with different management recommendations (Fig. 1).17 In this sense, the IPA allows us to identify the most appropriate strategies to optimize the different types of resources and improve competitiveness. Its main use has been described in studies on tourism, education, healthcare marketing, and service quality.22–24 In this study each of the CCFNI needs were considered as IPA attributes.
The matrix associated with the IPA consists of a Cartesian diagram, where the location and subsequent interpretation of each attribute are determined by the average score of its importance (Y axis) and satisfaction (axis X). To build the IPA quadrants, the median of each CCFNI dimension was considered as cut-off values to define its level (high/low) of importance and satisfaction. Quadrant A, called “concentrate here”, corresponds to the needs of high importance and low performance that require immediate attention to improve them. Quadrant B, “keep up the good work”, includes the needs of high importance and satisfaction where the organization performs good. The attributes with low importance and satisfaction correspond to quadrant C, called “low priority”, and they represent the organization's minor weaknesses. Finally, those attributes of low importance and high satisfaction are located in quadrant D, called “possible squandering of resources”, since they could be overrated.17,22
The reliability of CCFNI and that of its adapted version was assessed using Cronbach's alpha both for scales in general, and their dimensions. The statistics analyses were conducting using the statistic software SPSS version 22.0.
Ethical aspectsThe present study was approved by the Ethics Committee of the Pontifical Catholic University of Chile Medical School (# 16-207). All family members involved in the study accepted participating by signing a written informed consent document.
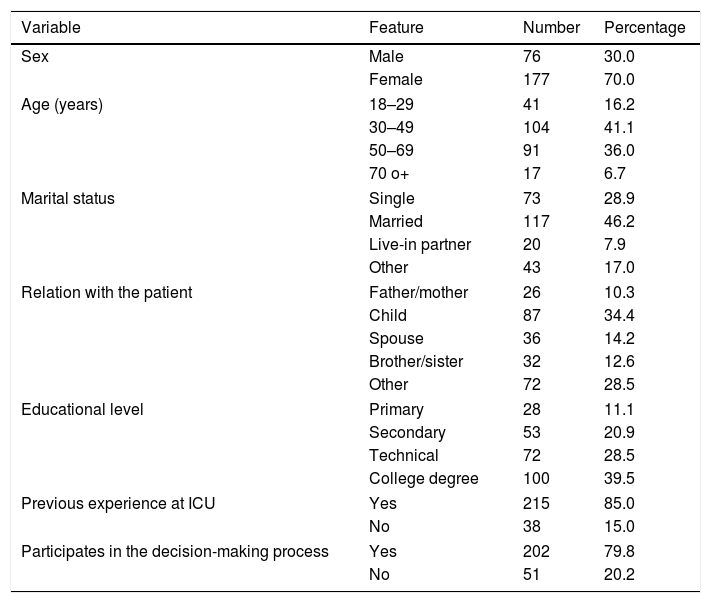
ResultsA total of 253 family members of critically ill patients were included, 70.0% of whom were women, the majority of an age between 30 and 49 years of age (41.1%) being the predominant relationship son/daughter (34.4%). In addition, most of them had the experience of having had a family member hospitalized at an ICU previously (85.0%) and participated in the decision making in connection with their relative's care and treatment (79.8%). 60.3% of the relatives were recruited up to the third day of the patient's stay at the ICU. On this respect, a similar proportion was observed between men and women, being predominantly older than 70 years of age (39.5%). The relatives’ socio-demographic characteristics are shown in Table 1.
Socio-demographic characteristics of the family members.
| Variable | Feature | Number | Percentage |
|---|---|---|---|
| Sex | Male | 76 | 30.0 |
| Female | 177 | 70.0 | |
| Age (years) | 18–29 | 41 | 16.2 |
| 30–49 | 104 | 41.1 | |
| 50–69 | 91 | 36.0 | |
| 70 o+ | 17 | 6.7 | |
| Marital status | Single | 73 | 28.9 |
| Married | 117 | 46.2 | |
| Live-in partner | 20 | 7.9 | |
| Other | 43 | 17.0 | |
| Relation with the patient | Father/mother | 26 | 10.3 |
| Child | 87 | 34.4 | |
| Spouse | 36 | 14.2 | |
| Brother/sister | 32 | 12.6 | |
| Other | 72 | 28.5 | |
| Educational level | Primary | 28 | 11.1 |
| Secondary | 53 | 20.9 | |
| Technical | 72 | 28.5 | |
| College degree | 100 | 39.5 | |
| Previous experience at ICU | Yes | 215 | 85.0 |
| No | 38 | 15.0 | |
| Participates in the decision-making process | Yes | 202 | 79.8 |
| No | 51 | 20.2 | |
ICU: Intensive Care Unit.
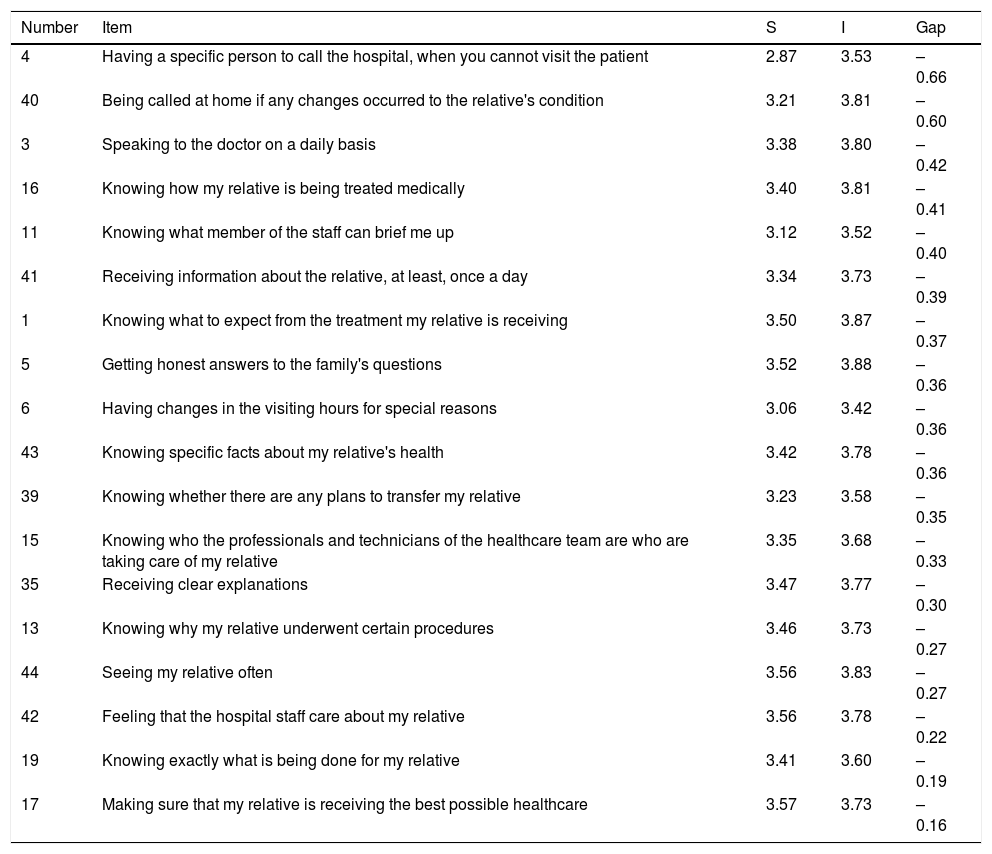
As to the difference between satisfaction and importance, it turned out to be negative in 71.1% (n=32) of the family needs, and a greater level of importance than of perceived satisfaction was observed. Table 2 shows that in the dimension of communication, 100% (n=18) of the family needs showed a negative difference, “having a specific person to call the hospital, when you cannot visit the patient” (−0.66), “being called at home if any changes occurred to the relative's condition” (−0.60) and “being able to talk to doctors every day” (−0.42) were among the ones of the biggest magnitude.
Gap between the degrees of satisfaction and importance of communication needs.
| Number | Item | S | I | Gap |
|---|---|---|---|---|
| 4 | Having a specific person to call the hospital, when you cannot visit the patient | 2.87 | 3.53 | –0.66 |
| 40 | Being called at home if any changes occurred to the relative's condition | 3.21 | 3.81 | –0.60 |
| 3 | Speaking to the doctor on a daily basis | 3.38 | 3.80 | –0.42 |
| 16 | Knowing how my relative is being treated medically | 3.40 | 3.81 | –0.41 |
| 11 | Knowing what member of the staff can brief me up | 3.12 | 3.52 | –0.40 |
| 41 | Receiving information about the relative, at least, once a day | 3.34 | 3.73 | –0.39 |
| 1 | Knowing what to expect from the treatment my relative is receiving | 3.50 | 3.87 | –0.37 |
| 5 | Getting honest answers to the family's questions | 3.52 | 3.88 | –0.36 |
| 6 | Having changes in the visiting hours for special reasons | 3.06 | 3.42 | –0.36 |
| 43 | Knowing specific facts about my relative's health | 3.42 | 3.78 | –0.36 |
| 39 | Knowing whether there are any plans to transfer my relative | 3.23 | 3.58 | –0.35 |
| 15 | Knowing who the professionals and technicians of the healthcare team are who are taking care of my relative | 3.35 | 3.68 | –0.33 |
| 35 | Receiving clear explanations | 3.47 | 3.77 | –0.30 |
| 13 | Knowing why my relative underwent certain procedures | 3.46 | 3.73 | –0.27 |
| 44 | Seeing my relative often | 3.56 | 3.83 | –0.27 |
| 42 | Feeling that the hospital staff care about my relative | 3.56 | 3.78 | –0.22 |
| 19 | Knowing exactly what is being done for my relative | 3.41 | 3.60 | –0.19 |
| 17 | Making sure that my relative is receiving the best possible healthcare | 3.57 | 3.73 | –0.16 |
I: importance; S: satisfaction.
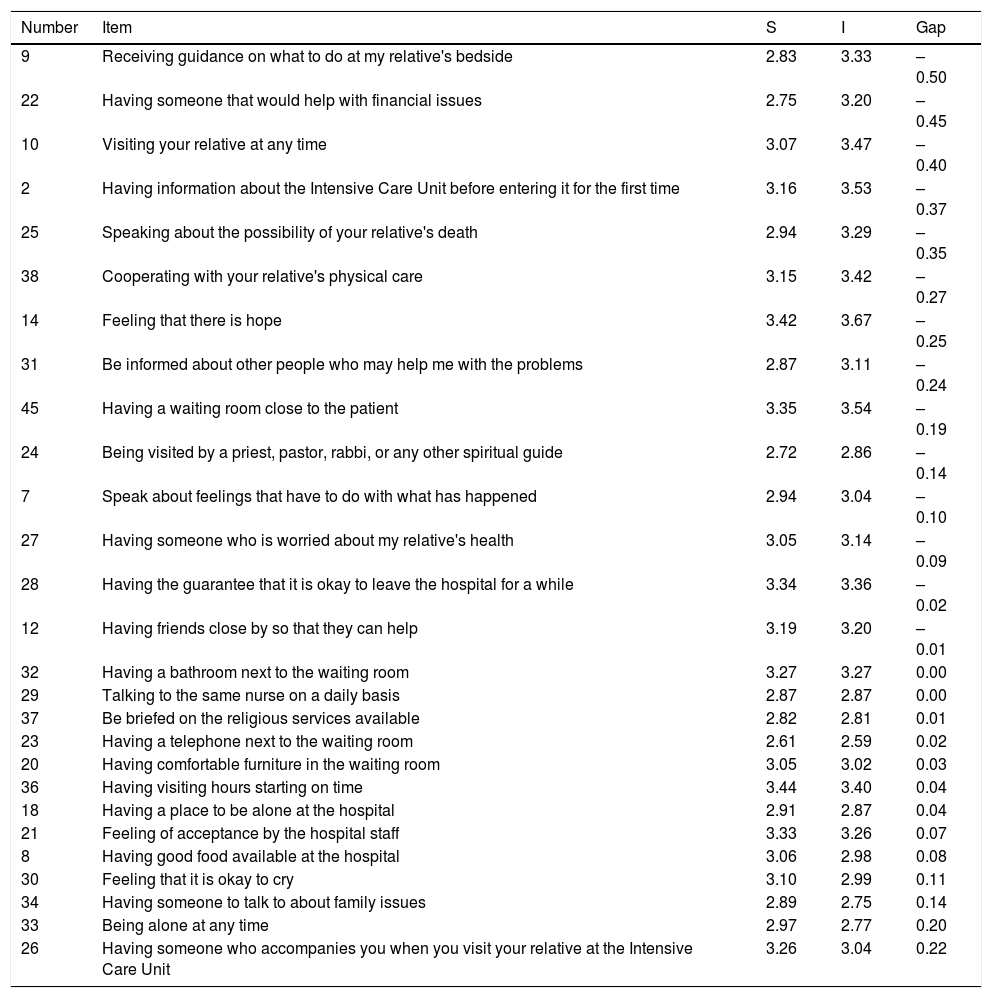
In the case of the dimension of support (Table 3), 51.9% (n=14) of the family needs showed a negative difference, and “receiving guidance on what to do at my relative's bedside” (−0.50), “having someone that would help with financial issues” (−0.45) and “visiting your relative at any time” (−0.40), were the ones with the highest value. Compared to the dimension of communication, there was a positive difference in 44.4% (n=12) of the needs.
Gap between the degrees of satisfaction and importance of support needs.
| Number | Item | S | I | Gap |
|---|---|---|---|---|
| 9 | Receiving guidance on what to do at my relative's bedside | 2.83 | 3.33 | –0.50 |
| 22 | Having someone that would help with financial issues | 2.75 | 3.20 | –0.45 |
| 10 | Visiting your relative at any time | 3.07 | 3.47 | –0.40 |
| 2 | Having information about the Intensive Care Unit before entering it for the first time | 3.16 | 3.53 | –0.37 |
| 25 | Speaking about the possibility of your relative's death | 2.94 | 3.29 | –0.35 |
| 38 | Cooperating with your relative's physical care | 3.15 | 3.42 | –0.27 |
| 14 | Feeling that there is hope | 3.42 | 3.67 | –0.25 |
| 31 | Be informed about other people who may help me with the problems | 2.87 | 3.11 | –0.24 |
| 45 | Having a waiting room close to the patient | 3.35 | 3.54 | –0.19 |
| 24 | Being visited by a priest, pastor, rabbi, or any other spiritual guide | 2.72 | 2.86 | –0.14 |
| 7 | Speak about feelings that have to do with what has happened | 2.94 | 3.04 | –0.10 |
| 27 | Having someone who is worried about my relative's health | 3.05 | 3.14 | –0.09 |
| 28 | Having the guarantee that it is okay to leave the hospital for a while | 3.34 | 3.36 | –0.02 |
| 12 | Having friends close by so that they can help | 3.19 | 3.20 | –0.01 |
| 32 | Having a bathroom next to the waiting room | 3.27 | 3.27 | 0.00 |
| 29 | Talking to the same nurse on a daily basis | 2.87 | 2.87 | 0.00 |
| 37 | Be briefed on the religious services available | 2.82 | 2.81 | 0.01 |
| 23 | Having a telephone next to the waiting room | 2.61 | 2.59 | 0.02 |
| 20 | Having comfortable furniture in the waiting room | 3.05 | 3.02 | 0.03 |
| 36 | Having visiting hours starting on time | 3.44 | 3.40 | 0.04 |
| 18 | Having a place to be alone at the hospital | 2.91 | 2.87 | 0.04 |
| 21 | Feeling of acceptance by the hospital staff | 3.33 | 3.26 | 0.07 |
| 8 | Having good food available at the hospital | 3.06 | 2.98 | 0.08 |
| 30 | Feeling that it is okay to cry | 3.10 | 2.99 | 0.11 |
| 34 | Having someone to talk to about family issues | 2.89 | 2.75 | 0.14 |
| 33 | Being alone at any time | 2.97 | 2.77 | 0.20 |
| 26 | Having someone who accompanies you when you visit your relative at the Intensive Care Unit | 3.26 | 3.04 | 0.22 |
I: importance; S: satisfaction.
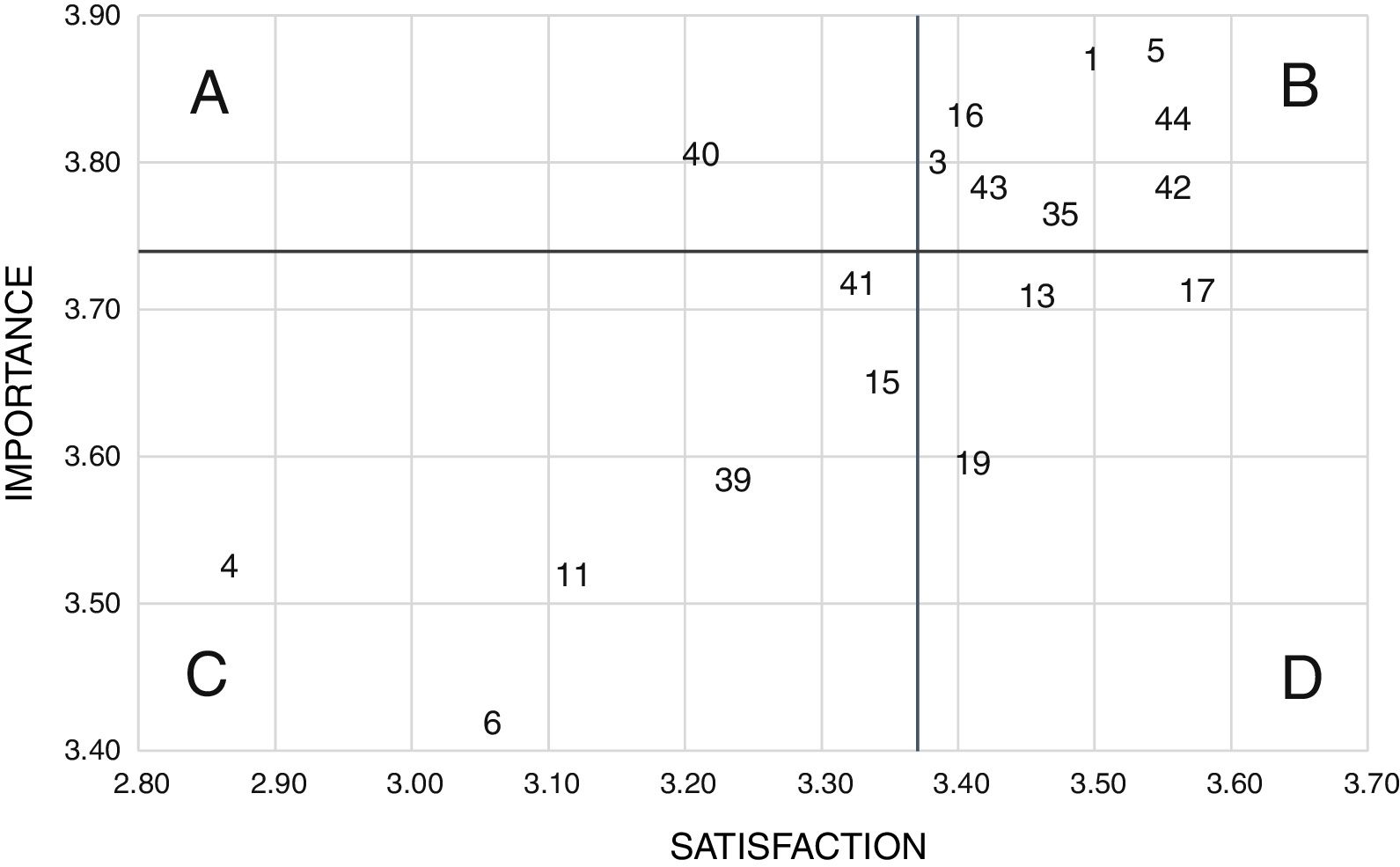
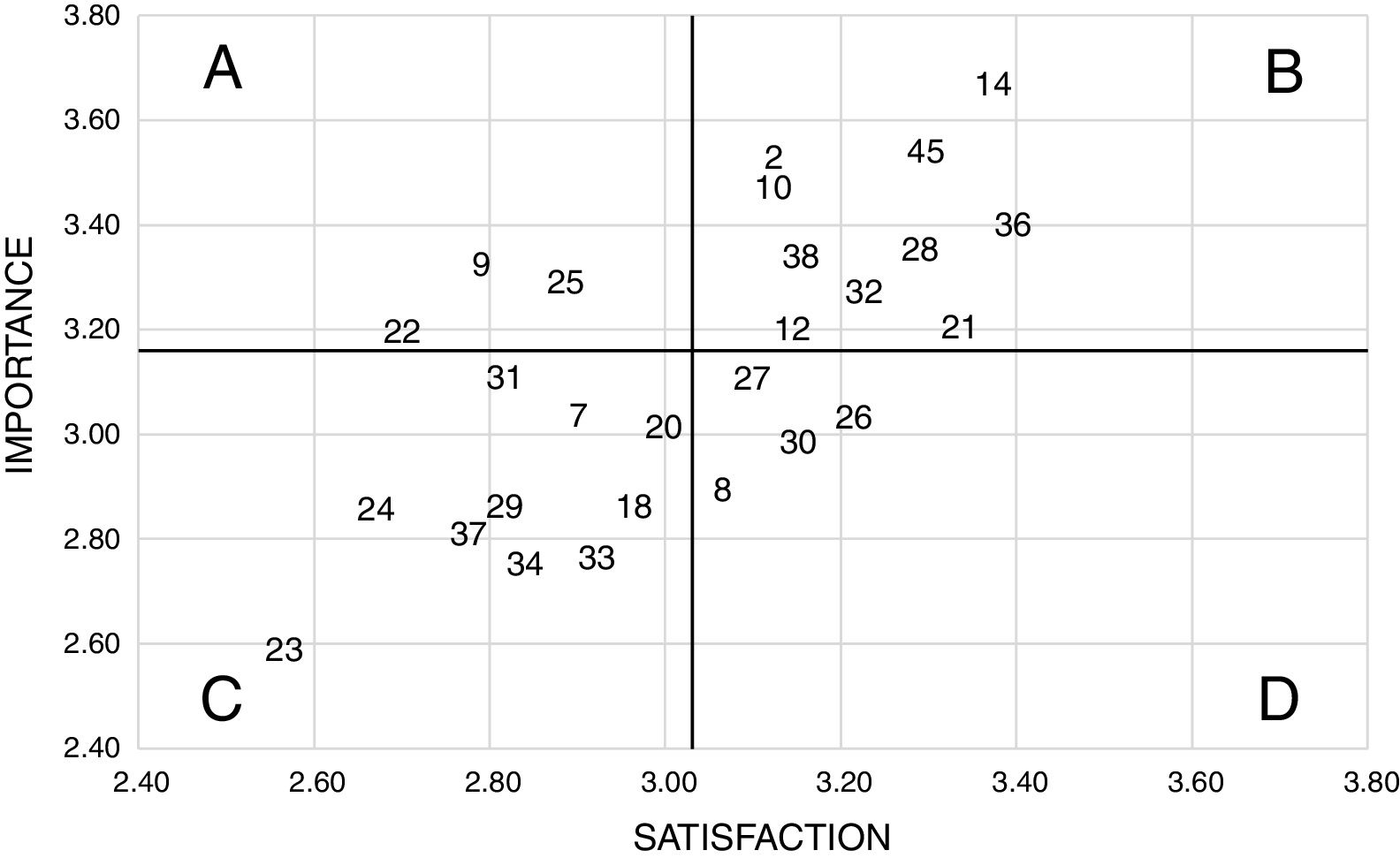
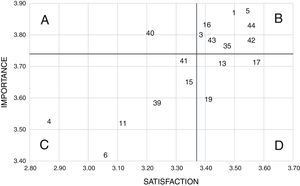
With respect to the IPA methodology, the cut-off points of the matrix were defined with the median for the level of importance of the needs of the communication dimension equaling 3.74, while for that of satisfaction, it equaled 3.34. In turn, in the dimension of support a median of 3.16 was observed in the degree of importance and 3.03 in that of satisfaction. Fig. 2 shows that most needs of communication concentrated on quadrant B (44.4%), while only “being called at home if any changes occurred to the relative's condition” belonged to quadrant A. Similarly, the support needs (Fig. 3) were grouped preferentially in quadrant B (37.1%), while quadrant A was included the need “speaking about the possibility of your relative's death”, “having someone that would help with financial issues” and “receiving guidance on what to do at my relative's bedside”.
When it comes to the reliability of the questionnaires, adequate internal consistency was observed both in the original CCFNI version (α=0.91) and in the modified version (α=0.96). Similarly, the dimensions of communication and support obtained high levels of reliability, both in their levels of importance (α=0.82 and 0.89) and satisfaction (α=0.93 and 0.94).
DiscussionThe goal of this study was to analyze the difference between importance and satisfaction in relation to the needs of critically ill patients’ family members. Although it is possible to find studies in the medical literature that have explored both features of family needs,25,26 as far as we know, our study is the first application of the IPA methodology for the analysis of the difference between importance and satisfaction.
The negative difference observed in all the needs of the dimension of communication was determined mainly by the high levels of importance reported by the family members, which is consistent with what has been observed in other studies on the need for information,3,10,27 and contrasts with the low levels of satisfaction. In order to address these differences, it is necessary to incorporate new strategies that would allow optimizing communication between the family and the healthcare team, such as family meetings, participation in clinical rounds, training in communication skills, or the incorporation of a nurse, within the multidisciplinary ICU team, exclusively devoted to the family. These interventions have proven to be able to improve family satisfaction with communication, commitment from the family, and the healthcare personnel self-efficacy.28,29 Additionally, more specific information on how the ICU actually works such as visiting hours, the assignments of each and every member of the team, and common care and therapies could be made available through leaflets or websites, that have already been able to improve understanding diagnoses and procedures, increase satisfaction, and lower the levels of post-traumatic stress in the family members.30,31
The most important negative difference was observed in the need for being called if any changes occurred in the patient's condition, which also turned out to be the only priority need in the dimension of communication. This may be associated with the high level of importance observed, which was considerably greater compared to other studies,2 which, in turn, would contribute to increasing this difference. Although the need to call someone in particular when they could not visit the patient showed the greatest difference of all in the dimension of communication, it is shown in the low priority quadrant.
In the case of the dimension of support, the two needs with the greatest difference of all also turned out to be priorities according to the IPA methodology. The need for receiving guidance on what to do at my relative's bedside would be associated with the family's growing interest in having a more active role in the process of recovery of their loved ones. In this sense, the participation of the family in the basic care of the critically ill patient, such as bathing, oral hygiene, feeding or assistance in the mobilization of the limbs, has proven to have a positive impact on the levels of anxiety, depression, and satisfaction of the family needs, which would help reduce such differences.32,33
In turn, the need for help with respect to financial issues could be explained in the context of the high costs involved in the care and treatment of a patient in critical condition, which is not usually reduced substantially by the local healthcare team. Although the ICU team can be trained to address different family needs, intervention on this particular need would require the management and knowledge of more suitable professionals, such as social workers who, according to the medical literature, not only can cooperate solving the family's financial issues,34 but also provide counseling and psychosocial evaluation, crisis intervention, family training, and support to the ICU members.35 The addition of other professionals with specific, complementary competences will bring the traditional structure of multidisciplinary teams at the ICU to new levels of competence.
The last priority need, speaking about the possibility of their relative's death, was associated with an important negative difference due to a low level of satisfaction that could be explained by different factors. In general, healthcare professionals receive training to maintain health and prevent disease, but training in other aspects is often insufficient, for example, communicating with a patient who is dying and with their family. Also, this could make it difficult to discuss important decisions at the ICU, such as limiting the therapeutic effort.36 Also, that there are cultural and socio-demographic factors, such as beliefs, religion or the geographical area that influence the way the families and professionals make decisions and brief one another on issues that have to do with the end of life.37 In this sense, up to 49% of the patients hospitalized at European ICUs and 25% of those hospitalized in South American make decisions that have to do with suspending or maintaining life-support therapies.38 These elements add to the need for regularly training ICU professionals on effective communication techniques.
When it comes to the tool being used to find out about family needs, the CCFNI is considered to be a valid, reliable tool with suitable psychometric properties.39 However, the 45 items that make up the CCFNI could be a problem in cases where a much larger number of priority attributes were to be observed compared to the number found in this study. Comparatively, the CCFNI has a significantly greater number of attributes compared to other tools used to evaluate the family satisfaction at the ICU, such as the 24-item version of the Family Satisfaction in the Intensive Care Unit or the Critical Care Family Satisfaction Survey – including 20 items. In this sense, the range of the Likert scale associated with the CCFNI (1–4) may not have been broad enough to expose more clearly the differences seen among some of the needs. Also, it is not possible to rule out the fact that a low assessment of some needs may have been associated with the lack of the of the “not applicable” option in the CCFNI. A future validation of the tools that explore these differences should include broader Likert scales with appropriate selection alternatives.
Finally, this study has some limitations, among these the type of sampling used because, since it is not probabilistic, it could have introduced some degree of selection bias. Also, only family members from a single private center were included which means that the interpretation and extrapolation of the results should have been made with caution. On the contrary, among the strengths of the study, we should emphasize here that most studies using the IPA methodology are based on selecting a set of attributes whose validity and reliability have not been confirmed previously. However, in our study, a validated CCFNI version was implemented, which, in addition to the results of internal consistency, increases the reliability of the results obtained. Finally, the sample size used is larger than that of other studies that have assessed importance and family satisfaction at the ICU setting, although without using the IPA methodology.26,27
ConclusionThere is a negative difference between the degrees of importance and satisfaction in the needs from most critically ill patients’ families determined by low satisfaction and high importance, especially in the dimension of communication. The IPA methodology confirmed than only a low percentage of needs should be addressed as a priority, while in a high percentage of those we would be doing a good job. Also, the IPA methodology is a simple tool that allows us to organize the needs and differences of family needs hierarchically facilitating the optimization of the interventions aimed at providing healthcare which would be more consistent with the families’ expectations and requirements at the ICU setting.
FundingThis study has been funded by Nursing School Masters Directorate at the Pontifical Catholic University of Chile as part of the contest “Support while elaborating the Nursing master's thesis (APET-2017)”.
AuthorsCP, NR, and MA participated in the study design. CP conducted the analysis and interpretation of data. CP, NR, and MA collaborated reviewing the manuscript. All authors read and approved the final version of the manuscript.
Conflicts of interestThe authors declare no conflicts of interest whatsoever.
We wish to thank all family members from this ICU for their generous participation in this research. Also, we wish to thank Paz Pardo, Andrea Piña, and Constanza Isla for their committed work during the data mining process.
Please cite this article as: Padilla-Fortunatti C, Rojas-Silva N, Arechabala-Mantuliz MC. Análisis de la diferencia entre importancia y satisfacción de las necesidades de los familiares de pacientes críticos. Med Intensiva. 2019;43:217–224.