To ascertain the ability of adrenomedullin (ADM) and proadrenomedullin (proADM) to predict mortality in sepsis patients.
DesignA systematic literature search was made of the PubMed, EMBASE, Cochrane and China National Knowledge Infrastructure (CNKI) databases before May 2017, supplemented by manual searches of references. A meta-analysis of high-quality clinical studies was subsequently performed to assess the association between ADM/proADM and mortality risk among patients with sepsis.
PatientsThirteen studies involving 2556 patients were included in the study.
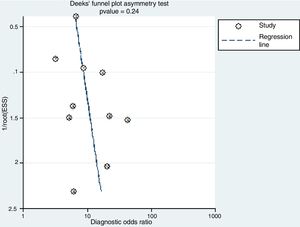
InterventionsTwo reviewers independently identified articles, extracted data, assessed quality and cross-checked the results. The predictive values of ADM and proADM referred to mortality were assessed by relative risk (RR). The overall diagnostic accuracy of ADM and proADM in application to sepsis was pooled according to a bivariate model. Publication bias was assessed using Deek's funnel plot asymmetry test.
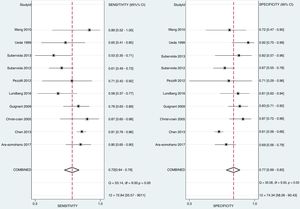
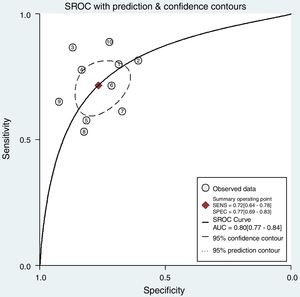
ResultsElevated ADM or proADM levels were associated with increased mortality (pooled RR=3.31; 95%CI 2.31–4.75). Subgroup analyses indicated the pooled RRs were 3.12 (95%CI 1.75–5.56) and 3.43 (95%CI 2.21–5.31) for ADM and proADM, respectively. The pooled sensitivity and specificity were 0.72 (95%CI 0.64–0.78) and 0.77 (95%CI 0.69–0.83), respectively. The overall area under the summary receiver operating characteristic (SROC) curve was 0.80 (95%CI 0.77–0.84). Publication bias was not statistically significant.
ConclusionsBoth ADM and proADM might serve as useful markers for predicting the prognosis of sepsis.
Establecer la capacidad de la adrenomedulina (ADM) y la proadrenomedulina (proADM) para predecir la mortalidad en pacientes sépticos.
DiseñoSe llevó a cabo una búsqueda sistemática de la literatura científica en las bases de datos PubMed, EMBASE, Cochrane y China National Knowledge Infrastructure (CNKI) antes de mayo de 2017, complementada con búsquedas manuales de referencia. Posteriormente, se realizó un metaanálisis de estudios clínicos de alta calidad para evaluar la asociación entre ADM/proADM y el riesgo de mortalidad en pacientes con sepsis.
PacientesEn este análisis se incluyeron 30 estudios en los que participó un total de 2.556 pacientes.
IntervencionesDos revisores identificaron de forma independiente los artículos, extrajeron los datos, evaluaron la calidad y realizaron verificaciones cruzadas de los resultados. Se evaluó el valor de ADM y proADM como factor pronóstico de mortalidad a partir del riesgo relativo (RR). La precisión global del diagnóstico con ADM y proADM en pacientes con sepsis se agrupó utilizando un modelo de 2 variables. Se evaluó el sesgo de publicación utilizando una prueba de Deek para asimetría de gráfico en embudo.
ResultadosLas concentraciones elevadas de ADM o proADM se asociaron a un aumento de la mortalidad (RR agrupado: 3,31; IC del 95%: 2,31-4,75). Los análisis por subgrupos indicaron que los RR agrupados eran de 3,12 (IC del 95%: 1,75-5,56) y 3,43 (IC del 95%: 2,21-5,31) para ADM y proADM, respectivamente. La sensibilidad y especificidad agrupadas fueron 0,72 (IC del 95%: 0,64-0,78) y 0,77 (IC del 95%: 0,69-0,83), respectivamente. El área global bajo la curva (SROC) fue de 0,80 (IC del 95%: 0,77-0,84). El sesgo de publicación no fue estadísticamente relevante.
ConclusionesTanto ADM como proADM pueden ser marcadores útiles para predecir el pronóstico de pacientes con sepsis.
Sepsis, a syndrome with physiologic, pathologic, and biochemical abnormalities triggered by infection, is a major challenge in intensive care units (ICUs) and emergency departments (EDs).1 Despite advances in antibiotic therapy and modern life support in past decade, the in-hospital mortality rate of US patients with sepsis has remained as high as 15%, posing a heavy burden to critically ill populations.2
One the most important reasons why first-line clinical physicians fail to provide timely and accurate treatment to sepsis patients is the lack of rapid and accurate diagnostic tools.3 It is therefore necessary and urgent to develop a rapid, simple, and accurate method to improve the diagnosis of sepsis. Adrenomedullin (ADM) is a 52-amino-acid peptide which can act as a hormone and is produced and secreted by multiple mammalian tissues during physiologic and infectious stress.4 Several clinical trials have demonstrated that ADM increases significantly in patients with sepsis and is positively associated with disease severity. Compared with normal individuals, ADM levels are 25- to 30-fold higher in patients with septic shock.5,6 Thus, quantification of ADM may be helpful in diagnosing and monitoring sepsis as well as establishing prognosis.5 As ADM is rapidly cleared from the circulation, the mid-region part of proadrenomedullin (proADM) that directly shows level of the fast degraded active peptide of ADM may be used instead of ADM as a predictor of sepsis.7
The present systematic review and meta-analysis aims to evaluate the prognostic value of ADM and proADM for mortality of patients with sepsis and assess their diagnostic accuracy.
MethodsSearch strategyThis systematic review and meta-analysis was performed and reported in accordance with the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).8 PubMed, EMBASE and The Cochrane Library were searched for trials in English, and China National Knowledge Infrastructure (CNKI) database were searched for trials in Chinese to identify the relevant published studies for clinical data. Searches were conducted separately for each literature databases up to May 2017. The search terms for each database were (“adrenomedullin” OR “proadrenomedullin” OR “mid-regional proadrenomedullin” OR “MR-proadrenomedullin”) AND (“sepsis” OR “septicemia” OR “septicaemia” OR “septic” OR “septic shock”). In addition to our computerized search, the bibliographies of all articles were reviewed to look for other potential articles with eligible data for the meta-analysis. The corresponding authors or first authors of the publications were contacted if additional information was needed, results were unclear, or relevant data were not reported.
Studies were considered eligible for the systematic review ad meta-analysis if they fulfilled the following criteria: 1) data was from an original, peer-reviewed study rather than review articles or meeting abstracts; 2) patients with sepsis or septic shock; 3) studies that provided mortality or diagnostic characteristics, that is, the area under the receiver operating characteristic (ROC) curve (AUC), or sensitivity and specificity. We excluded studies that were animal studies or duplicate studies.
Article screeningAfter deduplication, references were screened based on their titles and abstracts against a set of pre-defined eligibility criteria. Only one reviewer was involved in this round of review and the criteria was relative wide. If any uncertainty on inclusion existed, a second reviewer would join to assess and reach a consensus. Then, the full texts of retained references after first-round screening were obtained and reviewed by two reviewers against stringent inclusion criteria. Disagreements were resolved through discussion, and consensus was reached through a third party. All papers included after completion of the full text review were retained for data extraction and quality assessment.
Data extraction and quality assessmentThe following information was extracted from the eligible studies: first author, publication year, country of origin, setting, sample size, gender distribution, mean ages, mortality rate, test methods, and diagnostic performances (AUC, cut-off value, sensitivity, and specificity).
Two investigators independently assessed the quality of eligible studies using the revised Quality Assessment for Studies of Diagnostic Accuracy tool (QUADAS-2).9 Agreement between the two reviewers for assessment of methodological quality was evaluated using the Cohen's Kappa statistic. Any disagreement in data extraction and quality assessment was resolved by discussion.
Statistical analysisThe analyses were performed with Review Manager (REVMAN) 5.3 Copenhagen (The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) and STATA (version 14; Stata Corp., College Station, Texas, USA). Reported values are 2-tailed, and hypothesis-testing results were considered statistically significant at P<0.05.
Relative risk (RR) was used to assess the predictive value of ADM and proADM for mortality. We tested heterogeneity with Cochran's Q statistic, with P<0.10 indicating heterogeneity, and quantified the degree of heterogeneity using the I2 and tau2 statistic. In case of significant heterogeneity between studies, DerSimonian and Laird random effects model was used; otherwise, the fixed effects model was performed.10 Publication bias was tested using Deek's funnel plot.
The presence of a threshold effect on the prognostic accuracy of ADM and proADM in patients with sepsis was evaluated with the Spearman correlation coefficient between the logits of sensitivity and specificity. If no threshold effect existed, a bivariate random effects regression model11 was used to calculate the pooled sensitivity, specificity, diagnostic odds ratio (DOR), positive likelihood ratio (PLR), and negative likelihood ratio (NLR). We also constructed a summary receiver operator characteristic (SROC) curve by plotting the individual and summary points of sensitivity and specificity to assess the overall diagnostic accuracy.12
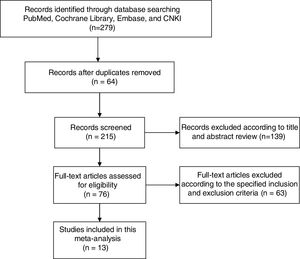
ResultsLiterature search and study characteristicsEventually, 13 articles were eventually included after examining the initial searched 279 articles. The process of study selection and the final results of the search were illustrated in the Flow Diagram (Fig. 1).
Thirteen studies involving 2556 patients were published from 1999 to 2017.13–25 Five studies reported the prognostic values of ADM and eight reported the proADM (Table 1). All studies were published in English. The mean age of patients varied between 60.0 and 72.0 years and the proportion of men ranged from 58.6% to 74.2%. Eight studies were performed in ICUs, two in EDs and three in both departments. Follow-up periods differed across studies, including 28-days mortality (5 studies), 90-days mortality (1 study), and in-hospital mortality (7 studies). The mortality rate varied from 23.5% to 47.6%.
Characteristics of included studies.
| Author | Year | Country | Setting | N | Age | Male (%) | Outcomes | Mortality rate | Cutoff value (nmol/l) | SEN (%) | SPE (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ADM | Ueda13 | 1999 | Japan | ED/ICU | 46 | 60.0±3.8 | 35 (76.1%) | 28-Day mortality | 28.3% | 0.15 | 65.0 | 92 |
| Chen14 | 2013 | China | ED | 684 | 72 (56–78) | 419 (61.3%) | In-hospital mortality | 34.7% | 34.49ng/l | 81.6 | 60.8 | |
| Marino15 | 2014 | Italy | ED | 101 | 78 (72–83) | 61 (60.4%) | 28-Day mortality | 28.7% | – | – | – | |
| Caironi16 | 2017 | Italy | ICU | 956 | 71 | 561 (58.7%) | 90-Day mortality | 38.6% | – | – | – | |
| Charles17 | 2017 | France | ICU | 237 | 67.8±13.7 | 110 (63.6%) | 28-Day mortality | 36.4% | 5.19 | – | – | |
| ProADM | Christ-Crain18 | 2005 | Switzerland | ICU | 53 | – | – | In-hospital mortality | 23.5% | 3.9 | 83.3 | 87.8 |
| Guignant19 | 2009 | France | ICU | 99 | 67 (54–76) | 58 (58.6%) | 28-Day mortality | 35.0% | 4 | 78.0 | 83.0 | |
| Wang20 | 2010 | China | ICU | 26 | – | – | In-hospital mortality | 30.8% | 0.8ng/ml | 91.0 | 73.0 | |
| Suberviola21 | 2012 | Spain | ICU | 49 | 59.4±13.4 | 33 (67.3%) | In-hospital mortality | 34.7% | 4.86 | 53.0 | 84.0 | |
| Suberviola22 | 2013 | Spain | ED/ICU | 137 | 62.6±15.9 | 90 (65.7%) | In-hospital mortality | 29.9% | 4.87 | 61.0 | 67.7 | |
| Pezzilli23 | 2012 | Italy | ICU | 21 | 69 (41–85) | 13 (61.9%) | In-hospital mortality | 47.6% | 1.64 | 71.4 | 72.7 | |
| Akpinar24 | 2014 | Turkey | ICU | 31 | 61.8±17.2 | 23 (74.2%) | In-hospital mortality | – | – | 24.0 | 90.3 | |
| Ara-Somohano25 | 2017 | France | ED/ICU | 116 | 72.0±14.8 | – | 28-Day mortality | 31.0% | 2.143 | 79.4 | 68.3 |
ADM: adrenomedullin; proADM: proadrenomedullin; ICU: intensive care unit; ED: emergence department; SEN: sensitivity; SPE: specificity.
Fig. 2 summarizes the methodological quality assessment with the QUADAS-2 tool of the thirteen included studies. Three studies were labeled as unclear in the patient selection domain as there is no report on whether patients were consecutive (Fig. 2A). For the index text domain, there is no cutoff value in three studies which has been labeled as unclear. The reference standard domain of two studies were labeled as high risk as the ADM or proADM levels were calculated before the endpoint was revealed. Seven studies were labeled as unclear because whether ADM or proADM were measured in a blinded fashion is unknown. There is neither risk in flow timing nor application concerns in all these thirteen studies (Fig. 2B). The Cohen's Kappa statistic for inter-rater agreement of assessment of quality between two reviewers was 0.84.
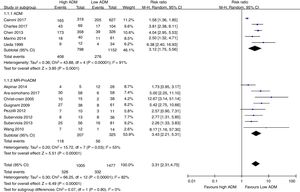
Association of ADM and proADM with mortalityAll studies showed that an elevated ADM or proADM levels were associated with a higher risk of death, with RR ranging from 1.58 to 12.67. Due to the substantial heterogeneity between studies (I2=82%, Tau2=0.30, Cochran's Q statistic P<0.01), a random-effects model was used to pool RR estimates (Fig. 3). The pooled RR in all the 13 studies was 3.31 (95%CI, 2.31–4.75). Subgroup analyses indicated the pooled RRs were 3.12 (95%CI, 1.75–5.56) and 3.43 (95%CI, 2.21–5.31) for ADM and proADM, respectively. To explore the source of between-study heterogeneity, further analyses was performed (data not shown), showing that the pooled RRs comparing high with low level of proADM were 2.96 (95%CI, 2.12–4.13) for in-hospital mortality and 5.21 (95%CI, 3.10–8.77) for 28-day mortality. The definition of cutoff value may also bring about heterogeneity as the pooled RRs were 3.18 (95%CI, 2.21–4.56) for high cutoff value (≥4nmol/l) and 5.43 (95%CI, 3.13–9.40) for low cutoff value (<4nmol/l).
Diagnostic accuracy of ADM and proADM for mortalityThere is no statistically significant difference when exploring for threshold effect (Spearman correlation coefficient=0.071; P=0.74). Totally ten studies were included for assessing the diagnostic accuracy of ADM and proADM for mortality in patients with sepsis. As shown in Fig. 4, the pooled sensitivity and specificity of included 10 studies were 0.72 (95%CI, 0.64–0.78) and 0.77 (95%CI, 0.69–0.83), respectively. The PLR and NLR were 3.1 (95%CI, 2.3–4.1) and 0.37 (95%CI, 0.29–0.47), respectively (data not shown). The DOR was 8.11 (95%CI, 5.25–12.54) (data not shown). The overall area under the SROC curve was 0.80 (95%CI, 0.77–0.84) (Fig. 5).
The Deek's funnel plot of the included studies showed that publication bias was not statistically significant (P=0.24) (Fig. 6).
DiscussionEarly prognosis and risk assessment after sepsis may provide timely and accurate treatment for patients. Since it is dominated by major peripheral vasodilation and other cardiovascular system alternations during the first hours after the onset of sepsis or septic shock,26 the measurement of the biomarkers including vasodilator and vasoconstrictor may be of great interest as they play vital roles in the homeostasis of the system. Our present systematic review and meta-analysis involving 13 high-quality clinical studies illustrates that both ADM and proADM are positively associated with the mortality risk for patients with sepsis.
Studies conducted by Chen et al.14 and Akpinar et al.24 show that ADM and proADM levels in survivors are significantly lower than those in non-survivors in patients with systemic inflammatory response syndrome (SIRS), sepsis, severe sepsis and septic shock. Moreover, ADM is regarded as an independent predictor of in-hospital mortality for sepsis in the multivariate logistic regressions.14,19 A similar positive association of proADM with short-term mortality in patients with community-acquired pneumonia (CAP) has been reported in a prior meta-analysis by Cavallazzi et al.27
The pooled sensitivity and specificity in this study were optimal, reaching 0.72 and 0.77, respectively. Generally, there is a trade-off between sensitivity and specificity in a test of diagnostic accuracy. That is, an increase in sensitivity (the true positive rate) is usually accompanied by a reduction in specificity (the true negative rate). Thus, the AUC should be a comprehensive index. The present study found that the AUC for sROC was 0.80 (95%CI, 0.77–0.84), which was greater than the results of published meta-analyses of procalcitonin,28 troponins29 and lactate clearance.30 A study reported by Ara-Somohano evaluated eight biomarkers (ProADM, proANP, pro-endothelin, copeptin, amino-terminal pro-B-type Natriuretic Peptide, troponin, C-reactive protein, procalcitonin) to predict short-term mortality in patients with sepsis, among which ProADM (AUC=0.731; 95%CI: 0.658–0.804) presented the best accuracy. All the results revealed that ADM and proADM should be a strong predictor for sepsis mortality.
In view of the complexity of the sepsis response, a great number of researchers have attempted to combine the comprehensive but subjective and time-consuming severity scoring systems with biomarkers. The prognostic ability of the combination of ADM with Mortality in Emergency Department Sepsis (MEDS) score was superior to either ADM or MEDS score alone.14 In addition, the combination of Sequential Organ Failure Assessment (SOFA), Acute Physiological and Chronic Health Evaluation (APACHE) II scores, and MR-proADM was efficient to predict prognosis and mortality rate in severe sepsis or septic shock patients.24 These data indicate that combined use of severity scoring systems and biomarkers is more effective in risk stratification and prognosis.
Flaws in the design of these studies should be considered when interpreting the results of the present systematic review and meta-analysis. It is sometimes not clear how the investigators selected the subjects (consecutively, randomly, or neither).13,16,24 If the subjects were not recruited either consecutively or randomly, this may introduce selection bias. The thresholds used in the studies were not always pre-specified, which may also introduce bias.15,16,24 In addition, a limitation inherent to the meta-analysis is the potential heterogeneity among studies that might lead to inaccurate conclusions. This may relate to the fact that the definition of mortality and cutoff values were inconsistent across the trials. Moreover, most studies included in this meta-analysis are performed prior to the publication of the updated definitions and clinical criteria of sepsis and septic shock (SPESIS-3),31 which may cause a potential limitation on the reproducibility of the results.
ConclusionThe present systematic review indicates that ADM and proADM are effective biomarkers for the prediction of mortality risk in patients with sepsis. Further systematic reviews need to be performed to assess the accuracy of combination of ADM/proADM with severity scoring systems or other biomarkers.
ContributionsAll authors have approved the final article. QL, BW, LY, CP, LM and CC design the experiment, collect data and write this article; QL and BW perform the analysis.
Conflict of interestThe authors declare no conflict of interest.
The study was supported by Science and Technology Plan Project of Chengguan District of Lanzhou (No. 2016-7-17).