Trauma is one of the leading causes of death and potential years of life lost worldwide. Nearly 5% of trauma patients die during their initial care, often without the cause of death being identified by the clinician.1 Additionally, incorrect placement of medical devices is a common thing that can contribute to increased morbidity and mortality.2,3
The study of preventable mortality (PM) is part of quality programs in trauma care systems. The World Health Organization (WHO) defines PM as cases with Injury Severity Scores (ISS) < 20, and/or an estimated survival probability by the Trauma and Injury Severity Score (TRISS) > 50%. Rates < 2% are considered acceptable for a trauma center.4
A significant limitation for the study of PM is the absence of injury identification in patients who die early. Such patients are not well represented in large trauma registries.5 Autopsy is considered the gold standard to assess the cause of death. However, its performance has decreased in recent years, as it requires time and resources, and clinical data for analysis are difficult to obtain.2,6,7
The use of post-mortem computed tomography (PMCT) is a widely used tool in the field of forensic medicine and is growing thanks to its low invasiveness, speed, and low cost. Its use in severe cases of trauma can help health care workers identify the cause of death, often hidden when based solely on physical examination and basic radiology. Additionally, it allows for completing trauma records and verifying the correct placement of medical devices used during patient care.3,5,6 However, no similar studies have ever been conducted in our country to this date.
This is our pilot experience performing PMCT on trauma patients who died during initial care. The radiological study was conducted after death was declared to avoid post-mortem artifacts. A baseline study of the whole body, including limbs, was performed without the administration of IV contrast and without removing the medical devices used during patient care. Infusion pumps and drainage suction devices were disconnected, though mechanical ventilation was maintained to prevent lung collapse.
The PMCT readings were interpreted by 2 independent radiologists experienced in the management of polytrauma patients. The most plausible cause of death and the calculated ISS were determined in a joint clinical session between the Radiodiagnosis and Intensive Medicine services after reviewing the images and medical history.
The project was evaluated by the hospital research ethics committee with a favorable result, required family consent for the analysis of the images and data obtained. Since PMCT is a non-invasive imaging modality without any repercussions on the cadaver and its results can be affected by the time until it is eventually performed, implicit consent was used for immediate performance after death.
We have managed 7 cases since 2022. All of them were men, being the most frequent injury mechanism falls (n = 4; 57%), followed by motorcycle accidents (n = 2; 28%), and gunshots (n = 1; 15%). The mean age was 46 years ±16, and the median ISS calculated by post-mortem tomography, 50 (±16).
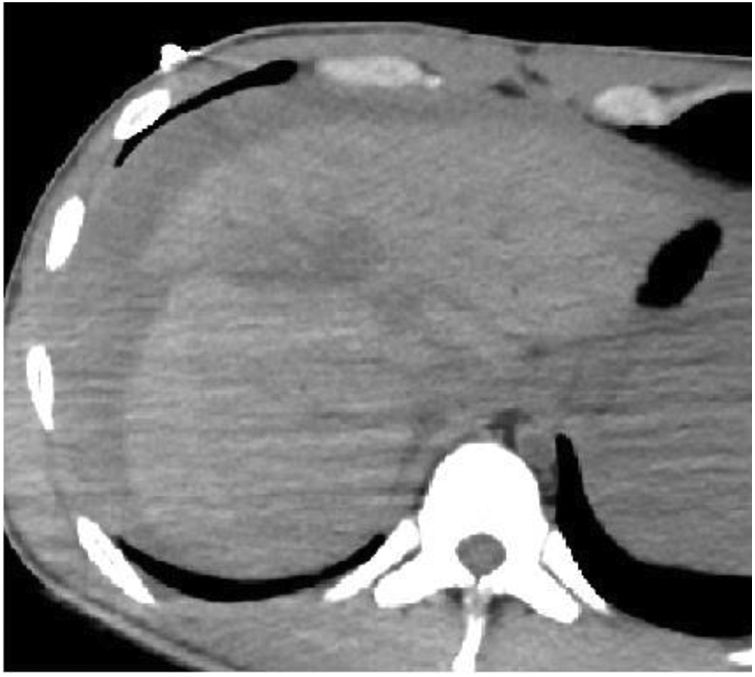
The most probable cause of death was identified in 100% of the patients, being thoracic trauma the main contributor, followed by hemorrhagic shock. Fig. 1 illustrates an example of hemorrhagic shock due to a high-grade liver injury.
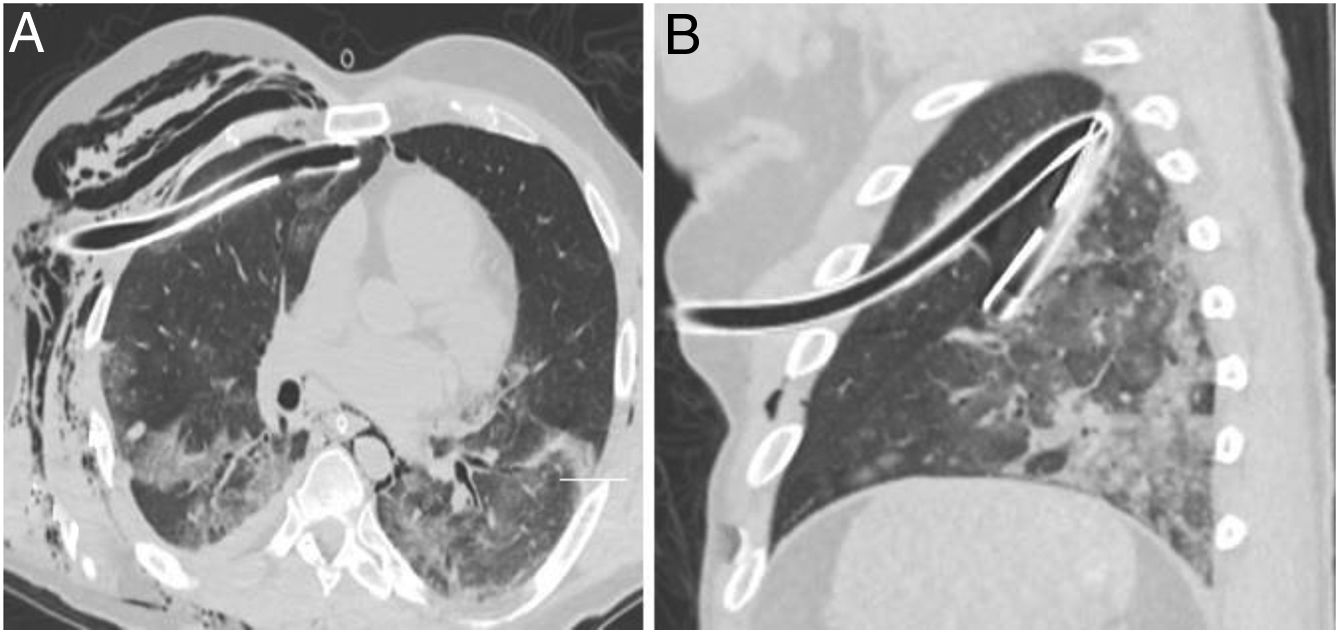
Regarding medical devices, they were removed in two patients prior to performing the PMCT. Still, we could identify the incorrect positioning of some devices in 80% of the remaining cases, being the most common incorrect position the inadequate placement of the endotracheal tube in relation to the carina. The most severe case was the incorrect placement of 2 chest tubes in the same patient, as shown in Fig. 2.
There was 1 case of PM based on ISS and TRISS. The results related to the cause of death, associated injuries, devices, and PM are shown in Table 1 of the Supplementary data.
The main limitation of PMCT is the identification of solid organ injuries and vascular lesions due to the absence of IV contrast and spontaneous circulation. This may cause severe injuries to go unnoticed.6,8 However, such injuries were inferred through indirect data such as the presence of significant hemoperitoneum, organ deformity, or perivascular hematoma. In addition, indirect findings of exsanguination, such as hemothorax/hemoperitoneum, or large injuries to vital organs incompatible with life, are enough to identify the cause of death without having to pinpoint the exact bleeding site. Post-mortem angiography with IV contrast would improve these results but adds complexity to the study and use of resources. Additionally, its clinical utility compared to PMCT without IV contrast is currently uncertain to date.8
Based on this experience, we believe that the use of PMCT can be an epidemiological tool to analyze the cause of death in patients who die early from trauma, study PM, assess the quality of care, and become an educational tool to implement improvements in the health care protocols of such patients.
Authors’ contributionsAll authors contributed to the drafting of the manuscript and are part of the project.
FundingNone declared.
Conflict of interestNone declared.