Respiratory physiotherapy (RP) incorporates techniques to promote lung re-expansion and facilitate secretion clearance. Different studies1–3 have assessed their effectiveness using as outcome variables the development of postoperative pulmonary complications (PPC), with contradictory findings. Moreover, the physiological effects produced by RP, especially the changes in ventilation, have been poorly studied.4–6
The electrical impedance tomography (EIT) has been previously used to evaluate RP in different samples and using variable protocols which makes it difficult to extrapolate their results.4–7 Besides, their impact on the end expiratory lung volume (EELV) has not been compared among each other in one single study.
To describe the effects on global and regional end-expiratory lung volume produced by five RP techniques, we conducted an observational, analytical, cross-sectional, and prospective study between April and May 2019. The protocol was previously approved by the Private Hospital's Education and Research Committee.
There were included 15 healthy respiratory therapists (8 women and 7 men), with no history of lung diseases or smoking, with a mean age of 31.6 (± 4.2) years, a height of 1.67 (± 7.2) m, a weight of 65.8 (± 6.2) kg and a BMI of 23.2 (± 9.2) kg/m2.
The following RP techniques were carried out: Deep breathing (DB), Positive expiratory pressure (PEP), Intermittent positive pressure without PEEP valve (IPP), Intermittent positive pressure with PEEP valve (IPPP) and Incentive spirometry (IS) (Fig. 1).8
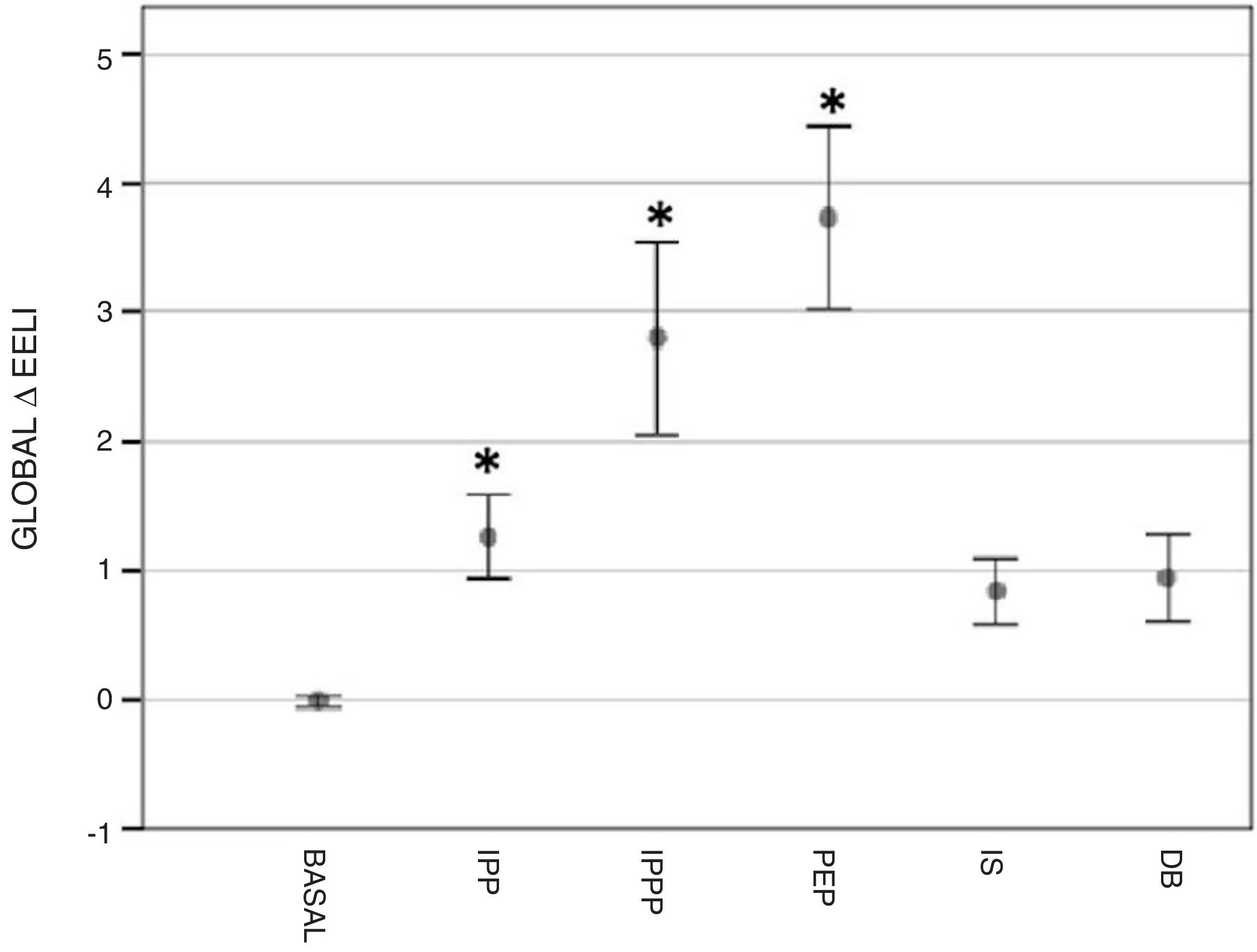
Regional change in end-expiratory lung impedance (ΔEELI) with the different techniques, expressed in units, as compared to the basal value. The values are expressed in mean and confidence interval of 95%. IPP: Intermittent positive pressure: 3 insufflations with a manual resuscitation bag and an oronasal interface, followed by a 3-s inspiratory hold and a gentle 3-s exhalation. IPPP-PEEP: Intermittent positive pressure with PEEP valve: same way as IPP, but a PEEP valve (10 cmH2O) was connected to the manual resuscitation bag. PEP: Positive expiratory pressure: deep inhalation until total lung capacity (TLC), followed by a 3-s inspiratory hold and then a slow 3-s exhalation through a 100cm plastic tube (inner diameter 8.8cm) connected to a bulau bottle with a 10-cm water column. IS: Incentive spirometry: Slow and deep inhalation until reaching TLC. Then, a 3-s hold and a gentle 3-s exhalation. The 3 ball incentive spirometer (MSC, Maximal Satisfaction Commitment) provided a visual feedback. DB: Deep breathing: 3 deep inhalation, without breathing out between each of them, until TLC, followed by a 3-s inspiratory hold and then a gentle 3-s exhalation. * P ≤ 0.05 compared to the basal value.
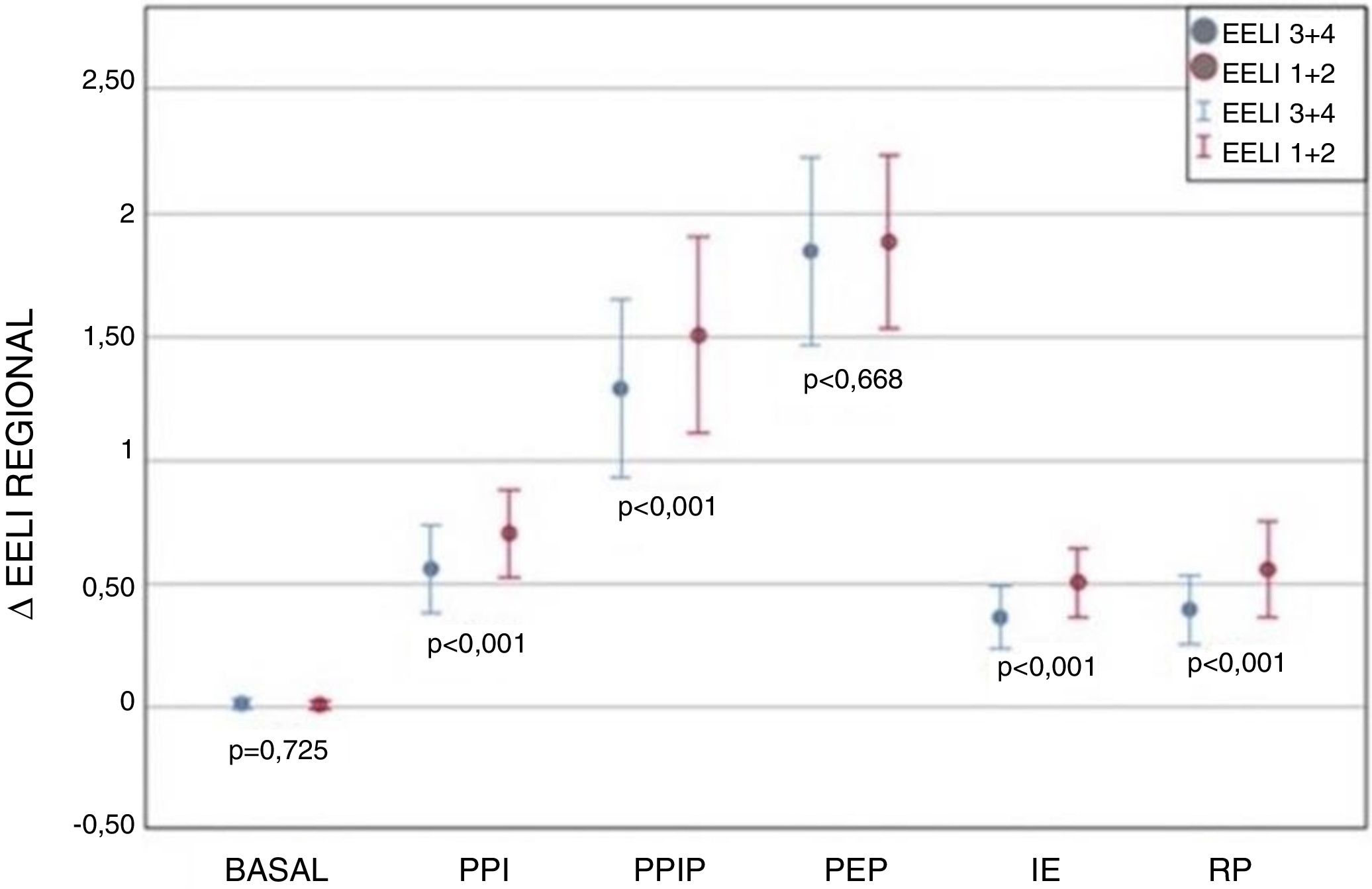
To obtain the measurements an EIT (PulmoVista500; Drager, Lubeck, Germany) was used together with a 16-electrode belt. To analyze the results we considered the sum of regions of interest (ROI) 1+2 (anterior right and left) and 3+4 (posterior right and left), determining the ventral and dorsal areas, respectively.
Each measurement was taken with the subject sitting at a 90-degree position. The study procedure began with a 5-min ventilation period at normal volume or until obtaining a stable value, which was regarded as the reference basal value. Afterwards, the techniques were carried out following an order that was randomly assigned.
The subjects repeated each technique 5 times followed by a 2-min rest period or until the reference values were reached. This sequence was repeated 3 times for each maneuver. Finally, the participants were asked to order the techniques according to the level of comfort when carrying them out, from the most comfortable to the least one.
The primary variable was the global and regional change in end-expiratory lung impedance (ΔEELI) at the end of each technique and the secondary variable consisted of the global and regional ΔEELI one minute after the completion of each technique.
The sample size was determined, based on previous studies.4–7 Continuous data were expressed as mean SD or as median and interquartile range. Categorical data were expressed as absolute values and/or percentages. An analysis of variance for repeated measurements and a Tukey Test with Bonferroni correction were performed. A value of p<0.05 was considered significant. For the statistical analysis the SPSS 25.0 software was used.
All of the assessed RP techniques resulted in an increase in end-expiratory lung impedance in relation to the basal value (primary variable); however, the mean of the global ΔEELI reached statistical significance only in the following: PEP (3.74±2.36; p<0.001), IPPP (2.80±2.51; p<0.001) and IPP (1.27±1.13; p<0.05). When comparing the global ΔEELI produced by these 3 techniques, a difference was found when contrasting PEP and IPPP with IPP (p<0.001) (Fig. 1).
One minute after the completion of each exercise no significant changes were recorded in the global ΔEELI when compared to the basal value (Secondary variable) (p>0.05). Furthermore, when comparing the means of the ΔEELI between regions (ventral and dorsal) a greater change was observed in ventral areas in all techniques, except PEP where the ΔEELI was similar in both areas (Fig. 2). PEP technique was selected as the least comfortable followed by the IPPP and IS.
Regional change in end-expiratory lung impedance (ΔEELI) with the different techniques, expressed in units, as compared to the basal value. The values are expressed in mean and confidence interval of 95%. IPP: Intermittent positive pressure, IPPP: Intermittent positive pressure with PEEP valve, PEP: Positive expiratory pressure, IS: Incentive spirometry, DB: Deep breathing.
This study provides important data that help better understand the impact of respiratory physiotherapy techniques and support the rationale for their implementation. PEP, IPPP and IPP produce an increase in global end-expiratory lung impedance, therefore they could be appropriate techniques to reverse the pulmonary consequences of thoracico-abdominal surgeries.
The finding that PEP and IPPP techniques were the ones that produced more change could be related to the fact that both include a resistance during the expiratory phase.
As previous studies, the use of PEP revealed a uniform distribution in ventral and dorsal areas.4,5,9 This finding could be explained by an increase in the redistribution of air through collateral ventilation due to the greater resistance during the expiratory phase. It is probable that the tube used for its construction could have added an additional resistance.10
As reported by other authors4,7 the global ΔEELI produced returned to basal values one minute after the conclusion. We consider this an expected behavior because the participants were healthy subjects. However, in posoperative patients, the increase in lung volume could be of significance to recruit collapsed alveolar units.
To our knowledge, this is the first study to comparatively assess the physiological behavior of the mostly used RP techniques in relation to EELV increase. All the participants were physical therapists, trained in the techniques which eliminate possible confounding factors such as the learning effect or the limitations deriving from each pathology. Future research should assess their impact on patients undergoing postoperative period of thoracoabdominal surgeries.
In conclusion, in healthy subjects the techniques PEP, IPP and IPPP generated an increase in end-expiratory lung volume evaluated through EIT. Unlike the other assessed respiratory physiotherapy exercises, the PEP technique achieved a homogeneous lung volume distribution similar to the basal one.
Authors’ contributionEach of the authors collaborated equally in the process (literature search, data collection, study design, analysis of data, manuscript preparation and review of manuscript).
Conflicts of interestThe authors declare that there are no conflicts of interest.