Every hour of delayed accumulated by the Intensive Medicine Service (IMS) increases the patient’s IMS-related and in-hospital mortality rates by 1.5% and 1%, respectively.1 To anticipate the detection and management of patients with significant clinical worsening, rapid response systems (RRS) have been developed in association with IMS. Although quality healthcare is at the center of the entire healthcare system, the Spanish Society of Intensive, Critical and Coronary Unit Medical Care (SEMICYUC) has not published any quality indicators associated with the activity of quality healthcare2 that is monitored by keeping count of activations, cardiac arrests, and occasionally, by estimating its repercussion in deaths and hospital admissions.3,4
The goal of this scientific letter is—based on a registry of the activity developed by our RRS—to analyze the prognostic dimension of several definitions of delayed alert (DA) for IMS admission and justify its estimation as a quality indicator to identify situations with room for improvement and deviation from the routine clinical practice. Our RRS is part of a tertiary level hospital with 2 different headquarters with 800 beds combined (35 of the IMS), 41 500 annual hospital admissions (2000 in IMS) and 200 000 hospital stays. It was first implemented back in 2012 in all hospital areas (except for IMS, pediatrics, and surgical rooms). The RRS is activated after clinical assessment by the nursing staff and, also, after registering into electronic health records values outside the range of vital statistics with a superimposed message of risk situation flashing on the screen. This is suggestive of call to the treating physician to activate the intensivist, when appropriate. If the former cannot be found or in cases of suspected great severity, the nursing staff should call the intensivist. All the physical examinations performed at the intensive care unit are prospectively registered into a database including demographic variables, pluripathology (hypertension stage ≥ 2, diabetes, chronic lung disease, kidney, liver or heart failure, neoplasm, and tracheostomy carrier), alert criterion (cardiocirculatory, respiratory, neurological, airway, warning due to cardiac arrest, subjective feeling of severity of the nurse or treating physician), warning service, working schedule, and score obtained from the patients’ risk scale. If the patient is hospitalized, the stay, the IMS-related mortality rate, and the 24-hour APACHE score5 are duly noted if they develop multi-organ failure (MOF) and if it is a DA. A total of 3 periods based on the evolution of our RRS were selected for analytical purposes: during the first period (P1), between January and June 2013, the Goldhill6 risk assessment tool (EPAR) with data from 1 of the 2 headquarters (280 beds, 17 of the IMS) was used; both the second period (P2), between March and November 2014, and the third period (P3), between May and June 2018, included both headquarters and the VIEWs scale.7 In P3 the emergency alerts were included. MOF was defined as damage to two or more organs with high scores > 2 in the SOFA8 scale. DA in P1 was defined as EPAR6 > 3 or ≥ 2 in the assessment of systolic arterial pressure or pulse oximetry at some point of the 3 working schedules prior to IMS admission. In P2 and P3 the DA was defined with VIEWs7 scores > 7 in some of the 3 working schedules prior to IMS admission, and also if they had been referred from the ER or had stayed there for over 5 hours. DAs were compared with the rest using Fisher’s exact test, the chi-square test, Mann-Whitney U test, and the odds ratio (OR) with P values < .05.
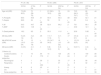
A total of 244 alerts were reported in P1, 544 in P2, and 343 in P3. The day’s average number of DAs was 0.81, 1.87, and 2.85, respectively, in each period. Also, the percentage of DAs was 13.52%, 6.3%, and 6.9%. Table 1 shows the differences of patients with DA at admission and the rest.
Characteristics of the alerts that end up in the IMS.
| P1 (N = 80) | P2 (N = 266) | P3 (N = 247) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 33 DA | 47 No DA | P | 34 DA | 232 No DA | P | 24 DA | 223 No DA | P | |
| Age md (IQR) | 75 (65-80.5) | 72 (58-76) | .1 | 67 (58.5-78.5) | 72 (69-79) | .53 | 70.5 (64.5-76.7) | 68 (52-77) | .44 |
| % Pluripath. | 66.6 | 59.5 | .51 | 55.9 | 50.4 | .58 | 58.3 | 52.1 | .61 |
| % Sepsis | 66.6 | 34 | < .05 | 50 | 19 | < .05 | 25 | 9.4 | < .05 |
| % M | 54.5 | 44.7 | .38 | 52.9 | 64.2 | .2 | 79.1 | 68.1 | .35 |
| % MOF | 54.5 | 14.9 | < .05 | ---- | ---- | ---- | 45.8 | 12.1 | < .05 |
| % Dead patients | 18.2 | 8.5 | .2 | 35.3 | 11.6 | < .05 | 20.8 | 5.82 | < .05 |
| Md stay (IQR) | 5 (2.5-14) | 3 (2-5) | .05 | 7 (1.7-11.5) | 3 (1-7) | .17 | 3.5 (2-9.7) | 2 (1-4) | .43 |
| Md APACHE score (IQR) | 19 (15.5-24) | 13 (10-18) | < .05 | 23 (14.7-34.5) | 16 (12-22) | < .05 | 15 (13-22.5) | 14 (9-20) | .1 |
| Md score (IQR) | 3 (3-5) | 2 (1-4) | .1 | 9 (8-12.2) | 6 (3-9) | < .05 | 9 (8-11) | 4 (3-8) | < .05 |
| Criterion (n) | |||||||||
| Cardiocirculatory | 11 | 16 | .94 | 14 | 120 | .25 | 6 | 100 | .06 |
| Doctor-subjective | 1 | 2 | .770 | 2 | 19 | .64 | 1 | 27 | .24 |
| Neurological | 4 | 1 | .09 | 2 | 33 | .17 | 8 | 56 | .44 |
| Respiratory | 1 | 3 | < .050 | 1 | 47 | < .05 | 8 | 32 | .01 |
| Airway | 6 | 8 | .23 | 4 | 3 | .5 | 0 | 0 | -- |
| CA | 1 | 0 | – | 0 | 3 | .5 | 1 | 5 | .01 |
| Nurse-subjective | 00 | 00 | – | 00 | 0 | -- | 0 | 3 | .56 |
P1, first period; P2, second period; P3, third period.
DA, delayed alert; p, significance level.
%, percentage; APACHE: Acute Physiology and Chronic Health Evaluation II;5 CA, cardiac arrest; IQR, interquartile range; M, males; Md, median; MOF, multi organ failure; pluripath, pluripathological patients; score, risk score.
The OR of deceased patients with DA in P1 was 2.39 (95%CI, 0.62-6.98), 4.14 in P2 (95%CI, 1.84-9.31), and 4.25 (1.37-13.2) in P3. On the other hand, the OR for developing MOF in P1 was 6.86 (95%CI, 2.39-19.71) and 6.14 (95%CI, 2.5-15.08) in P3. In conclusion, DAs multiply the chances of dying and developing MOF. Assessing this percentage facilitates the comparison between periods and hospitals and monitors the quality of the afferent arm (detection) of RRS. Establishing indicator standards is complex because the medical literature on this regard is scarce; however, with the existing literature, with the trajectory of implementation of the actual protocols, and with our own protocols the percentage should be < 20%. This means that 80% of the alerts that go off should not come with a delay.9,10
Conflicts of interestNone reported.
Please cite this article as: Castaño Ávila S, Fonseca San Miguel F, Urturi Matos JA, Iturbe Rementería M, Pérez Lejonagoitia C, Iribarren Diarasarri S. Alerta tardía a los sistemas de respuesta rápida: propuesta de un nuevo indicador de calidad. Med Intensiva. 2021;45:e50–e52.