To evaluate layperson (university student) ability to use an automated external defibrillator (AED).
DesignA repeated measures quasi-experimental study with non-probabilistic sampling and a control group was carried out.
ScopeTeacher training degree students at the University of Santiago de Compostela (Spain).
ParticipantsThe sample consisted of 129 subjects (69% women and 31% men), between 19 and 47 years of age (mean 23.2±4.7 years). As inclusion criterion, the subjects were required to have no previous knowledge of AED.
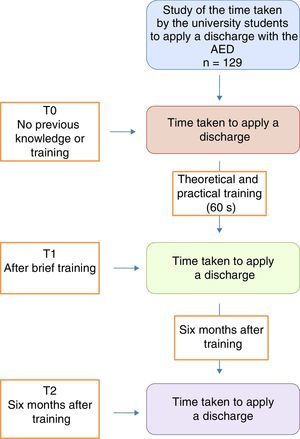
InterventionsTimes to apply defibrillation with an AED to a mannequin were recorded untrained (T0), after a theoretical and practice explanation lasting less than one minute (T1), and 6 months after the training process (T2).
Main variables of interestThe primary endpoint was the time taken to deliver a defibrillation discharge. The “improvement effect” variable was defined by the absolute time difference between T1 and T0, while the “degree of forgetfulness effect” variable was defined as the absolute difference between T1 and T2.
ResultsThe mean times were T0=67.7s; T1=44.2s; T2=45.9s. The time to apply defibrillation was reduced after explanation training (T1<T0) (−23.4s; p<0.001). T2 proved shorter than T0 (−21.8s; p<0.001) but longer than T1 (1.6s; p=0.002). The improvement effect was significant (p<0.001), in the same way as the degree of forgetfulness (p=0.002).
ConclusionsEasy handling of AED was demonstrated, since untrained people were able to deliver a discharge. Defibrillation time was reduced after brief training. This time barely increased after 6 months.
Evaluar la capacidad del personal lego (estudiantes universitarios) para usar un desfibrilador externo automatizado (DEA).
DiseñoEstudio cuasiexperimental de medidas repetidas de muestreo no probabilístico con grupo control.
ÁmbitoEstudiantes de formación de profesorado de la Universidad de Santiago de Compostela.
ParticipantesLa muestra estuvo compuesta por 129 sujetos, 69% mujeres y 31% hombres, de entre 19 y 47 años (media 23,2±4,7), cuyo criterio de inclusión fue el no tener conocimientos previos sobre DEA.
IntervencionesSe tomaron los tiempos empleados en aplicar una descarga sobre un maniquí con DEA sin formación (T0); tras una explicación teórico-práctica inferior a 1 minuto (T1) y tras 6 meses del proceso formativo (T2).
Variables de interés principalesLa variable de resultado principal fue el tiempo empleado en aplicar una descarga. Se definió la variable «efecto de mejora» mediante la diferencia absoluta de tiempo entre T1 y T0, y la variable «efecto de grado de olvido» como la diferencia absoluta entre T1 y T2.
ResultadosLas medias de tiempos fueron: T0=67,7s; T1=44,2s; T2=45,9s. Se redujo el tiempo para realizar una descarga tras la explicación formativa (T1<T0) (−23,4s; p<0,001). El T2 es inferior a T0 (−21,8s; p<0,001), pero mayor que T1 (1,6s; p=0,002). El efecto de mejora fue significativo (p<0,001), al igual que el grado de olvido (p=0,002).
ConclusionesSe demostró el fácil manejo del DEA, ya que personas sin formación fueron capaces de aplicar una descarga. El tiempo de administración de descarga se redujo tras una pequeña formación. Este tiempo apenas aumentó pasados 6 meses.
Out-hospital cardiac arrest (OHCA) is an important health problem associated to cardiovascular disease, due to its high incidence and mortality.1–3 A study conducted in 37 European countries found the annual incidence of OHCA attended by the emergency medical services to be 38 cases per 100,000 inhabitants.2 However, the on-site management of such cases is ineffective, since it is typically applied late, despite scientific evidence that early basic cardiopulmonary resuscitation performed by witnesses of the event can result in a three- to four-fold increase in the patient chances for survival.4 Thus, early basic life support (BLS) maneuvering is necessary in order to improve the prognosis of OHCA – including immediate defibrillation if available, since it forms part of the third link in the patient chain of survival.5 Early defibrillation and public access to automated external defibrillators (AEDs) have been shown to increase the chances for survival to 74%.6–10 When carried out in the first 3–5min after collapse, survival rates of up to 50–70% have been reported,11–13 provided the previous steps—i.e., recognition of cardiac arrest (CA), activation of the emergency system and start of CPR maneuvering—have been correctly executed. In this regard, the chances for survival decrease between 7 and 10% for every minute of delay.14
On the other hand, insufficient awareness and capacitation on the part of the general population in dealing with OHCA,15 and the lack of training in how to deal with an emergency, have suggested the need to incorporate instruction on the use of an AED to the protocolized educational setting in order to palliate this situation. Knowing how to apply BLS techniques means knowing how to save lives.16 In this regard, we can speak of a strategy for population-based access to public defibrillators, with the implementation of different programs—some of which have already been tested in practice.8,17,18 It has been shown that the first individuals to intervene (usually laypersons)19,20 can safely use a defibrillator, regardless of whether they have received basic training in its use or not.8,9
The present study aims to analyze the use and time taken by university students to apply a discharge with the AED, since it is considered that a good setting in which to start the chain of training in BLS techniques (including the handling of AEDs) would be the teacher training schools. In effect, once these university students become teaching professionals, they will be the individuals in closest contact with the children of the future, and thus may contribute to transmit this kind of knowledge in schools over the long term, providing instruction for as many people as possible. Furthermore, according to the observations of previous studies, both laypersons and children can use an AED without training.21,22
The objective of this study is therefore to analyze knowledge and skills referred to the use of the AED among a population of students of the University of Santiago de Compostela (Spain), without prior training or experience with BLS, and centered on their capacity to administer defibrillation with an AED—measuring the time taken to apply the discharge in three different scenarios: initially, without previous training; after a brief visual and theoretical explanation lasting less than one minute; and 6months after such training activities.
Materials and methodsStudy designA repeated measures, quasi-experimental design with a control group was used. The study was carried out in abidance with the ethical-regulatory principles of the Declaration of Helsinki (1964 and posterior updates), and approval was moreover obtained from the Bioethics Committee of the University of Santiago de Compostela. The participants in turn received a detailed explanation of the study objectives and protocol, the voluntary nature of participation, and the confidentiality of the responses and data. Verbal consent to participation was considered mandatory. The student intervention consisted of the following:
- (1)
Conceptual evaluation based on a questionnaire exploring knowledge of the AED (P-K); prior training in how to use the device (P-T); and its real use on some occasion (P-U).21,22
- (2)
After administration of the questionnaire, a clinical simulation of OHCA was carried out. The participants received access to an AED stored in its box alongside a Resusci Anne mannequin (Laerdal). From the moment in which the participants picked up the AED, we measured the time taken in fitting the device and delivering an effective discharge following the acoustic and visual instructions of the AED. This procedure was carried out on an individualized basis while one of the members of the research team applied continuous massage to the mannequin in order to produce a more realistic simulation.
- (3)
The time taken by the students in delivering an electric discharge was measured with a chronometer on three occasions (Fig. 1):
- -
Initially, upon receiving the defibrillator. The students were simply instructed to apply the device to the mannequin simulating OHCA, while one of the investigators simulated the application of continuous massage to the unconscious patient (T0).
- -
Following a brief individualized visual and theoretical explanation lasting no more than 60s, after which the students repeated the same operation as above (T1).
- -
Six months after first use of the defibrillator. In this case, the aim of the third application of the AED was to assess the long-term retention of the knowledge gained by the students (T2).
- -
The training provided between T0 and T1 involved a theoretical explanation of the steps to be followed in placing the AED and in delivering a discharge where required, following the recommendations of the American Heart Association (AHA)23 and the European Resuscitation Council (ERC).24 Practical simulation with the device was also explained: (1) turn on the device; (2) place the electrodes on the bare chest of the patient; (3) connect the electrodes to the device; and (4) press the discharge button when prompted to do so. The information was provided verbally and in practical form by one of the investigators.
In all cases, correct discharge was defined by placement of the electrode patches without the plastic covers onto the naked chest of the mannequin, likewise in accordance with the recommendations of the AHA23 and the ERC.24 The time taken was recorded from the moment in which the AED was picked up until the discharge button was pressed.
SampleThe experimental group consisted of a non-randomized sample of 129 subjects: 89women (69%) and 40 men (31%). All were students of the University of Santiago de Compostela (Spain), and informed consent to participation was obtained in all cases. The subjects were asked about their previous experience, training and use of the AED. Those individuals who had received previous training or had used the AED before were excluded from the study.
The control sample was selected on a convenience basis from among those individuals that gave informed consent to participation, and comprised 20 emergency healthcare technicians.25
InstrumentsAn individualized questionnaire was used to assess previous knowledge of AED among the university students, previous training in the use of the device, and previous use of the defibrillator on some occasion. The items of the questionnaire were of a dichotomic nature (Yes/No).
In the simulations, we used a Resusci Anne mannequin and an AED Trainer 2 (both from Laerdal).
Study variablesThe independent variables analyzed were subject age and gender, while the dependent variables were the times taken to deliver an effective discharge in three different moments: in the absence of previous knowledge (T0); after a brief explanation (T1); and 6 months (T2) after the first recording (T0). We also considered the variables “improvement effect”, defined as the absolute difference between T1 and T0, and the “degree of forgetfulness effect”, defined as the absolute difference between T1 and T2.
Statistical analysisAll the data were processed using the SPSS version 20 statistical package for MS Windows (SPSS Inc., IBM, USA). The data were reported with measures of central tendency (mean) and dispersion (standard deviation [SD]), with the corresponding 95% confidence interval (95%CI). The Kolmogorov–Smirnov test was used to assess normal distribution of the data. Repeated measures analysis of variance (ANOVA) with Bonferroni correction was used for the analysis of discharge time in each test, while the Pearson chi-squared test was applied for exploring group differences referred to age and gender.
ResultsThe analysis of the results obtained in relation to university student knowledge of the use of the AED is described below.
Of the 129 students included in the study, 71.3% did not know what an AED is (P-K); 100% claimed to have received no prior training (P-T); and 100% had never used the device before (P-U) (Table 1).
Results of the study questionnaire.
| Question | Yes, n (%) | No, n (%) | Total, n (%) |
|---|---|---|---|
| P-K | 37 (28.7) | 92 (71.3) | 129 (100) |
| P-T | – | 129 (100) | 129 (100) |
| P-U | – | 129 (100) | 129 (100) |
P-K: question on knowledge of the automated external defibrillator; P-T: question on training in the use of the automated external defibrillator; P-U: question on use of the automated external defibrillator.
A total of 28.7% of the university students had heard about AEDs, but had not received training or used the device before.
The results referred to the mean time (in seconds) taken by the students in applying a discharge with the AED were: T0=67.7 (SD=15.6) s; T1=44.2 (SD=6.3) s; T2=45.9 (SD=5.8)s. The mean time taken in applying a discharge among the emergency healthcare technicians was 51.9 (SD=9.7)s.
Table 2 shows the results of the repeated measures analysis of the mean times to defibrillation among the university students in the different moments of the study. Within-subject contrast testing revealed significant interaction between the time taken to deliver a discharge and the moment in which the time was recorded (T0, T1 and T2) – 66.5% of the variance of the study being explained by interaction of the factors F(1,128)=253.79 (p<0.001; Eta2p=0.665). This means that there were statistically significant differences among the three time measurements, i.e., the observed differences were not attributable to chance. A decrease of 23.4s in mean defibrillation time was observed after having received training (“improvement effect”) (34.6%). The defibrillation time in turn increased an average of 1.6s as measured after 6 months (T2) (3.7%) (“degree of forgetfulness effect”), but was still shorter than the mean time recorded at T0.
Descriptive statistics of the variable time with respect to gender and total.
| Variable | Men | Women | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Time (s) | Mean | SD | No. | Mean | SD | No. | Mean | SD | No. |
| T0 | 68.8 | 17.6 | 40 | 67.2 | 14.7 | 89 | 67.7 | 15.6 | 129 |
| T1 | 44.0 | 6.2 | 40 | 44.3 | 6.4 | 89 | 44.2 | 6.3 | 129 |
| T2 | 45.4 | 6.1 | 40 | 46.1 | 5.7 | 89 | 45.9 | 5.8 | 129 |
SD: standard deviation; No.: number of subjects; T0: collection of data without training; T1: collection of data after training for 60s; T2: collection of data 6 months after training.
The variable “improvement effect” was not influenced by either gender (p=0.540) or age (p=0.124) – T0 being the only variable conditioning the decrease in time registries (p=0.004). Likewise, neither gender (p=0.637) nor age (p=0.272) exerted an influence upon the variable “degree of forgetfulness effect”.
Table 3 shows the results of the bivariate comparative analysis of the mean defibrillation times of the university students in the different moments of the study.
Paired comparisons of the variable time.
| Variable | Men | women | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Time (s) | Difference of means | p | Upper and lower limit | Difference of means | p | Upper and lower limit | Difference of means | p | Upper and lower limit |
| T0-T1 | 24.7 | <0.001 | 31.8 | 22.8 | <0.001 | 26.8 | 23.4 | <0.001 | 26.9 |
| 17.6 | 18.9 | 25.1 | |||||||
| T1-T2 | −1.3 | 0.760 | 1.5 | −1.8 | 0.001 | −0.6 | −1.6 | 0.002 | −0.5 |
| −4.1 | −2.9 | −2.8 | |||||||
| T0-T2 | 23.4 | <0.001 | 30.1 | 21.0 | <0.001 | 24.9 | 21.8 | <0.001 | 25.1 |
| 16.7 | 17.2 | 18.5 | |||||||
T0: without training; T1: after training; T2: 6 months after training.
The numbers in boldface indicate the observed significant differences.
After the brief basic training provided, the time taken in delivering a discharge was seen to decrease 34.6%. Six months after the training received, the time was found to have increased an average of 1.6s.
On the other hand, regarding the results of the multivariate analysis of the mean defibrillation times of the university students in the different moments of the study, compared with the times recorded in the control group (emergency healthcare technicians), between-subject contrast testing revealed F (time 1)(1,148)=19.08 (p<0.001); F (time 2)(1,148)=21.71 (p<0.001) and F (time 3)(1,148)=15.04 (p<0.001). This means that there were statistically significant differences among the three time measurements, i.e., the observed differences were not attributable to chance – time 1 being understood as (T0us and T0eht); time 2 as (T1us and T0eht), and time 3 as (T2us and T0eht).
DiscussionThe present study shows the capacity of laypersons (university students) both without and with brief training to use an AED, compared with a group of trained staff. The findings confirm that defibrillation performed by first intervening individuals using a public access ARD is a feasible and effective strategy, in concordance with the observations in other settings, such as Japan, where excellent results were recorded in real interventions.8 Indeed, even 9-year-old children are able to understand the importance of CPR performed by witnesses, and can learn to apply BLS measures and retain the knowledge gained.26,27
The data obtained show that skill in using the AED after a brief (no more than 60s) explanation of how the device is employed and handled is noticeably greater than when the AED is used without any type of training. Specifically, the time required was found to decrease by 34.6%. This result is also 7.7s better than that obtained by the trained staff (emergency healthcare technicians). The explanation for this could be that most BLS training courses involve teamwork by two individuals: a first technician starts continuous cardiac massage, while the other member of the team is in charge of telephone activation of the emergency service switchboard and fitting of the AED. In this context, the technicians are more thoroughly trained in such aspects and in the quality of cardiac massage—with less emphasis being placed on immediate rapidity of execution.
On the other hand, the response time barely increased among the layperson sample after 6 months (−3.7%), and remained significantly better than the time taken in the absence of any previous training (about 23.4s). It therefore can be concluded that there is good retention of the skills gained, and in contrast to the situation in the case of thoracic compression maneuvers,28 no reinforcement training would be needed in under 6 months, since the time taken to deliver the discharge was seen to increase very little.21
This 22-s difference in skill retention cannot be attributed to biological aspects of the participants, since their ages were similar, and moreover studies are available corresponding to individuals of younger age in which long-term retention was found to be similar.22 Based on the results obtained, it is seen that skills in using an AED are easily gained and retained, independently of the age of the individual.
If laypersons were able to make use of a defibrillator several minutes before the arrival of professional help, the survival rates could be improved to about 49–75%.10 This is of great importance, since an early defibrillation program has a better chance for success if the time elapsed from CA to defibrillation is under 12min.29
On the basis of the results obtained, and as reflected by the European Resuscitation Council (ERC), AEDs can be regarded as safe and effective when used by both laypersons and medical staff.24 The Spanish Cardiopulmonary Resuscitation Council considers liberalization of the non-negligent use of AEDs by untrained non-sanitary staff (citizens in general) to be adequate when done with the intention of helping a CA victim.30
The results obtained in this investigation support the recommendations of the Spanish Cardiopulmonary Resuscitation Council,30 the ERC24 and the AHA,23 since university students—as a sample of general citizens without training in the use of defibrillators—can apply a discharge with the AED if necessary.
All this would reinforce implementation of the strategy proposed in 1992 by the AHA,31 whereby placing the AED in the hands of a great number of people capable of using the device could represent the key intervention for increasing the chances of survival among patients with OHCA. The generalized effectiveness and safety demonstrated by the AED make it acceptable for effective handling by non-professionals,8 in conjunction with the necessary recommendations and instructions received from the urgencies and emergencies coordination centers by telephone.32
In the context of training in BLS, the recognition of OHCA, activation of the emergencies system and the start of basic CPR maneuvering are crucial elements, followed by the use of the AED (if available) as the third link in the chain of survival. However, it must be mentioned that mere use of the AED alone is not enough: correct execution of the previous steps is equally important.5 For this reason, citizen training in BLS is essential, even when the programs used for this purpose are very brief, as demonstrated in the present study.
These contents should be incorporated to the training of future teachers, with a view to reaching as much of the population as possible. In this regard, teachers are regarded as targets for training since they in turn can become future instructors in their own classroom settings,33,34 transmitting this knowledge to the children in the morning, with the aim of achieving the goal of the ERC,5 i.e., to ensure that defibrillation with the AED occurs between 3 and 5min after patient collapse, though the adoption of programs contemplating public access to devices of this kind.
LimitationsDue to ethical reasons, this study has not been carried out in the real-life setting. Instead, we simulated OHCA with a mannequin and a training AED. On the other hand, it is not clear whether the study design (an investigator performing continuous massage) may have influenced the electrode application times.
It was not the aim of our study to assess AED safety of use (defibrillation errors), and the errors in placing the patches on recording of the initial times periods were not documented. We likewise did not measure the time taken in removing the patient clothing, and have not evaluated the quality of basic CPR performed by the investigators.
The sample consisted of university students, and in this regard we do not know whether the assimilation of knowledge may have been faster in these individuals due to their particular academic characteristics.
ConclusionsConsensus is still lacking regarding the timelines for a training program in AED, though our study could be a starting point for implementing public access to early defibrillation, since the AED is easy to handle. The university students, as laypersons without training, were able to perform defibrillation without prior instruction.
Training is simple, and should be carried out in the context of the university education of teacher training school students, as possible future teachers of children who in turn can receive the necessary knowledge and offer better chances for survival among people who suffer OHCA.
FundingNo funding was received for this investigation or preparation of the article.
AuthorshipAll the authors have participated in all parts of the investigation and in preparation of the manuscript (study conception and design, data acquisition, data analysis and interpretation, drafting of the manuscript, critical review of the intellectual content, and definitive approval of the manuscript).
Conflicts of interestThe authors declare that they have no conflicts of interest.
Thanks are due to the university students and the emergency healthcare technicians for their generous contribution to this study.
Please cite this article as: Basanta Camiño S, Navarro Patón R, Freire Tellado M, Barcala Furelos R, Pavón Prieto MP, Fernández López M, et al. Evaluación del conocimiento y de las habilidades para el uso de un Desfibrilador Externo Automatizado (DEA) por estudiantes universitarios. Un diseño cuasiexperimental. Med Intensiva. 2017;41:270–276.