In patients with inferior myocardial infarction, right ventricular myocardial infarction (RVMI) can occur in up to 50% of cases.1 It is associated with higher intra-hospital mortality rates.2
Management of RVMI includes preload optimization and maintenance of atrio-ventricular synchrony.3 Preload optimization is a mainstay of treatment, but it is also a double-edged sword. High filling pressures in the right ventricle can worsen the performance of preload optimization and may lead to right ventricular dilatation and further dysfunction. On the other hand, insufficient preload is associated with low right cardiac output, hypotension and shock.4
Right atrial pressure (RAP) is an essential component in the hemodynamic assessment of patients with RVMI.5 Unfortunately, RAP measurements are invasive and suffer from complications, and they are not always available to every patient. However, non-invasive evaluation of RAP is feasible with echocardiography and many techniques have been described.5 Even so, the usefulness of echocardiography in RAP assessment in patients with RVMI is uncertain.
The aim of this study was to assess whether echocardiography can accurately estimate RAP in patients with RVMI and predict increased RAP levels to guide management. The scope of the study was to assess the right ventricular function with comprehensive echocardiography and to measure the RAP with a central venous catheter.
In this study, patients with RVMI and elevated ST segment were analyzed. Consecutive cases were included from 2015 to 2016. Patients were required to satisfy a third universal definition of myocardial infarction (MI) and an ST-segment elevation of at least 0.1mV in the V4R lead.6 The Cardiology Hospital Ethical Committee revised and approved the protocol, and all of the patients gave written informed consent to participate in the study.
We conducted comprehensive echocardiograms at the bedside immediately after admission. We analyzed the following echocardiographic parameters according to current international guidelines7: tricuspid annular plane systolic excursion (TAPSE), tricuspid S′ wave velocity, global right ventricular longitudinal strain, free wall right ventricular longitudinal strain, right E/E′ ratio, right atrial area, inferior vena cava size and tricuspid regurgitation. We estimated right atrial pressure with the 3•8•15mmHg approach and the 5•10•15•20 approach according to guidelines. In the first approach the RAP is 3mmHg if inferior vena cava diameter is ≤21mm and the diameter changes ≥50% with sniff; RAP is 15mmHg if inferior vena cava diameter is>21mm and the diameter changes <50% with sniff; if neither condition is satisfied the RAP is 8mmHg. In the second approach the RAP is 5mmHg if inferior vena cava diameter is ≤21mm and the diameter changes ≥50% with sniff, if the diameter changes <50% RAP is 10mmHg; RAP is 15mmHg if inferior vena cava diameter is >21mm but the diameter changes ≥50% with sniff, if the diameter changes <50% RAP is 20mmHg. We measured parameters using the average of three consecutive beats in all cases. In cases of atrial fibrillation or atrioventricular block we used the average of five consecutive beats. Strain was analyzed offline with specific software (QLAB version 10.5, Philips Healthcare, Andover, MA, USA). Right ventricular longitudinal strain analyses consisted of a semi-automated process in which three points were selected: the tricuspid annular plane with the free wall and the interventricular septum, and the right ventricular (RV) apex. Right atrial strain analyses consisted of a similar process and three points were selected: the tricuspid annular plane with atrial lateral wall and interatrial septum, and the roof of the right atrium. We visually inspected the strain curves to ensure appropriate tracking. We defined global right ventricular longitudinal strain as the average of seven segments analyzed and free wall right ventricular longitudinal strain as the average of three free wall segments.
Just prior to the echocardiographic examination, we measured RAP with a central venous catheter as previously described in the literature.8 The RAP was measured for three times, and the average was reported in mmHg. We as investigators did not know RAP at either the time of examination or during the offline analysis. We defined increased RAP as being ≥13mmHg.
For statistical analysis we compared groups using the Student's t-test for independent groups. We used simple logistic regression and then we fit a multivariable logistic regression model with stepwise selection; the entry criteria were an association in the univariate analysis and a p value lower than 0.10, and the exit criterion was a p value higher than 0.05. We built a classification tree using the classification and regression tree (CRT) algorithm.9 We used SPSS version 22 (IBM, Chicago, IL, USA) and Stata 12 (StataCorp LP, College Station, TX, USA) for statistical analysis.
From 2015 to 2016, 460 patients had inferior MI and 106 patients fulfilled the right ventricular infarction criteria; 45 patients received a central venous catheter. Reliable RAP and complete echocardiographic was obtained for all of the 45 patients: age 68±10 years, male 71%, diabetes mellitus 58%, hypertension 76%, previous coronary artery disease 18%.
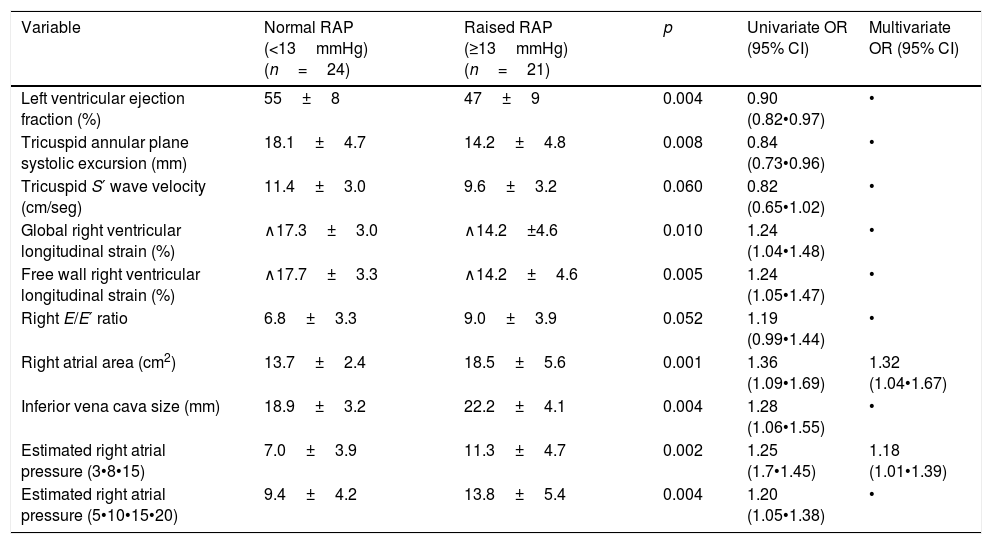
Based on univariate logistic regression, most of right heart echocardiographic variables predicted increased RAP. However, after the multivariate logistic regression, only the RAP assessment with the 3•8•15mmHg approach and the right atrial area remained independent predictors of raised RAP.
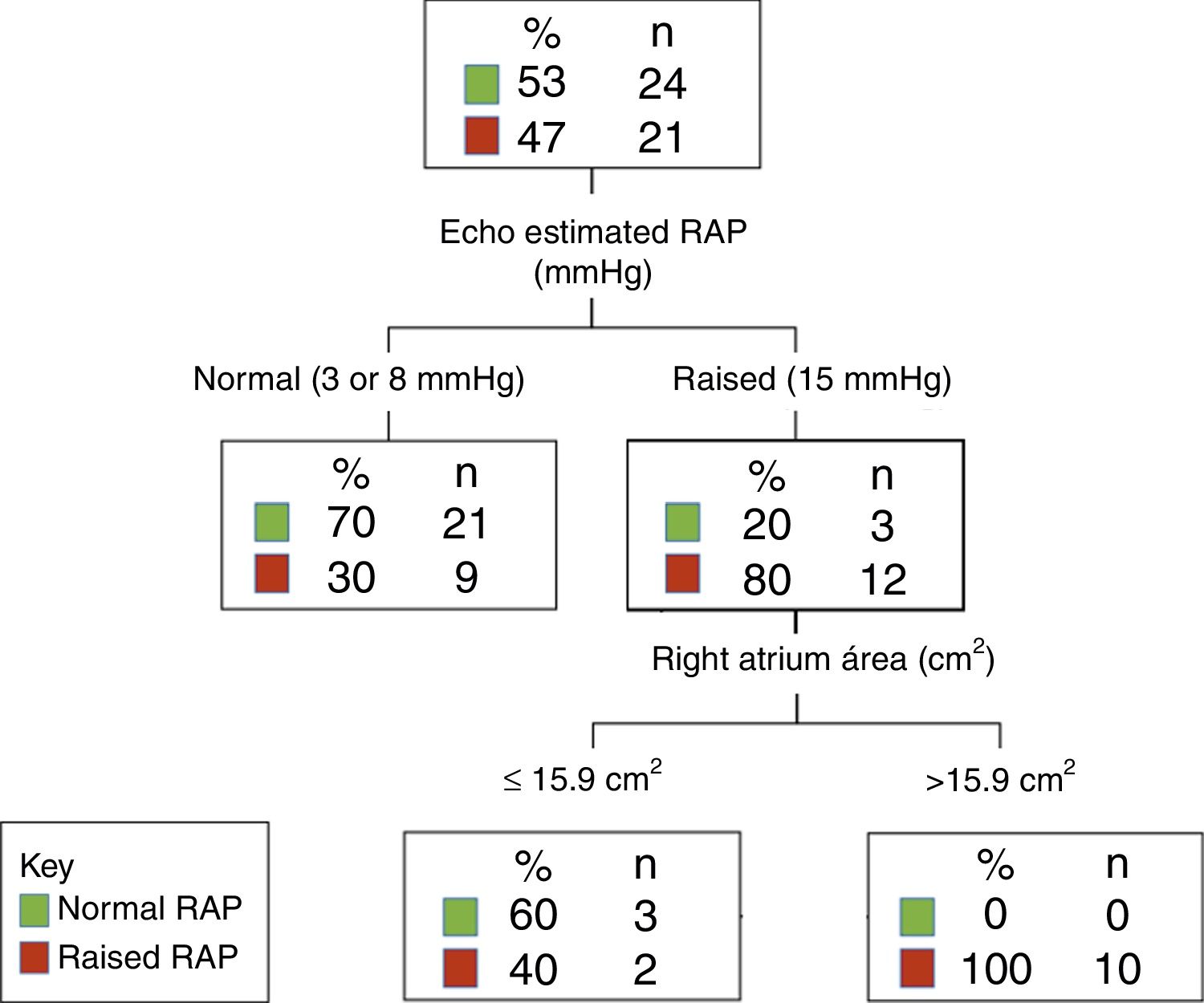
A classification tree showed that the right atrium area can be used to further identify patients with a higher probability of having raised RAP after the use of the 3•8•15mmHg approach; see Fig. 1.
In this study, the 3•8•15mmHg approach and right atrium area exhibited the highest correlation with RAP and were predictors of increased RAP (Table 1).
Echocardiographic predictors for raised right atrial pressure.
| Variable | Normal RAP (<13mmHg)(n=24) | Raised RAP (≥13mmHg)(n=21) | p | Univariate OR (95% CI) | Multivariate OR (95% CI) |
|---|---|---|---|---|---|
| Left ventricular ejection fraction (%) | 55±8 | 47±9 | 0.004 | 0.90 (0.82•0.97) | • |
| Tricuspid annular plane systolic excursion (mm) | 18.1±4.7 | 14.2±4.8 | 0.008 | 0.84 (0.73•0.96) | • |
| Tricuspid S′ wave velocity (cm/seg) | 11.4±3.0 | 9.6±3.2 | 0.060 | 0.82 (0.65•1.02) | • |
| Global right ventricular longitudinal strain (%) | ∧17.3±3.0 | ∧14.2±4.6 | 0.010 | 1.24 (1.04•1.48) | • |
| Free wall right ventricular longitudinal strain (%) | ∧17.7±3.3 | ∧14.2±4.6 | 0.005 | 1.24 (1.05•1.47) | • |
| Right E/E′ ratio | 6.8±3.3 | 9.0±3.9 | 0.052 | 1.19 (0.99•1.44) | • |
| Right atrial area (cm2) | 13.7±2.4 | 18.5±5.6 | 0.001 | 1.36 (1.09•1.69) | 1.32 (1.04•1.67) |
| Inferior vena cava size (mm) | 18.9±3.2 | 22.2±4.1 | 0.004 | 1.28 (1.06•1.55) | • |
| Estimated right atrial pressure (3•8•15) | 7.0±3.9 | 11.3±4.7 | 0.002 | 1.25 (1.7•1.45) | 1.18 (1.01•1.39) |
| Estimated right atrial pressure (5•10•15•20) | 9.4±4.2 | 13.8±5.4 | 0.004 | 1.20 (1.05•1.38) | • |
Data are mean±standard deviation. RAP=right atrial pressure.
We found that the 3•8•15mmHg approach (the one recommended by current international guidelines)7 showed the highest correlation with invasively obtained RAP. However, we emphasize that because of the importance of preload in patients with RVMI, accurately assessing RAP is critical. It is extremely important because both a very low and a very high preload have deleterious effects on right ventricular performance.4
In this study, the 3•8•15mmHg approach was the best predictor of RAP. This is explained because there is strong evidence to support the fact that inferior vena cava size and collapse during inspiration are closely related to RAP.5,8,10
Interestingly, novel echocardiographic parameters such strain were associated with RAP, but they did not improve reclassification after the 3•8•15mmHg approach.
The classification tree shows that when a patient has a normal estimated RAP (3 or 8mmHg in the 3•8•15mmHg approach), most patients will have a normal RAP. Therefore, preload optimization with a higher intravascular volume might be indicated depending on the hemodynamic state at that precise moment. However, if the estimated RAP is high (15mmHg in the 3•8•15mmHg approach), the clinician would not administer more volume in order to avoid right ventricular dilatation and dysfunction. However, up to 20% of patients do not have increased RAP and might need higher intravascular volume. The assessment of right atrium area will help to confirm increased RAP. If the right atrium is enlarged or close to the maximum area, 100% of patients will have increased RAP and thus, no further intravascular volume would be necessary. However, if the right atrium area is normal, up to 60% of patients will have normal RAP, and preload optimization might be warranted depending on hemodynamic state.
We note that this is an observational study and thus is susceptible to bias. Variability in echocardiographic measures and sample size are other limitations.
In conclusion, the echocardiography can accurately estimate a raised RAP in patients with RVMI and guide fluid management in these high risk patients.
FundingNo funding received for this study.
Conflicts of interestWe declare that we have no conflicts of interest to declare, relevant to the content of this paper.