There is a vast body of literature on cardiopulmonary arrest (CPA) and cardiopulmonary resuscitation (CPR) referred to aspects such as management and the role of witnesses and first interveners.1 In contrast, few studies have addressed whether to start CPR in the absence of do-not-resuscitate (DNR) orders or the presence of signs of doubtful usefulness.2,3 Guidelines have been published for not starting or suspending CPR,4 but the medical emergency service (ES) or hospital staff face decision-making dillemas.5 Moreover, factors such as the duration of CPA, prior CPR performed by witnesses, or age6,7 influence the start or continuation of advanced CPR. A study was therefore carried out to explore the attitudes of the professionals that assist CPA in the face of these situations, and the factors that may influence them.
An online survey was carried out among physicians and nurses assisting CPA in the out- and in-hospital settings. The study comprised two parts: one involving general questions (Table 1) and another addressing attitudes, with questions referred to 7 possible circumstances for not starting CPR, one question about whether they would perform CPR when their own personal criterion would indicate otherwise, and a group of questions referred to those situations in which they could perform CPR even if not indicated (Tables 1–5, electronic supplementary material [ESM]).
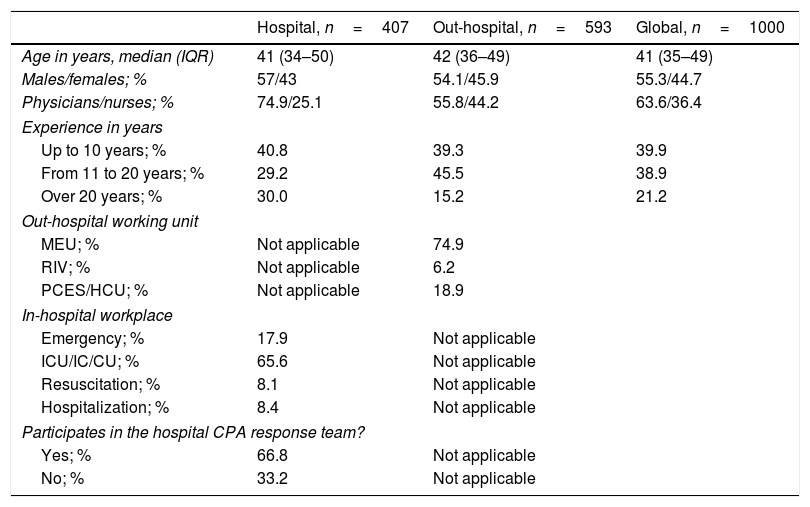
Characteristics of the surveyed professionals.
| Hospital, n=407 | Out-hospital, n=593 | Global, n=1000 | |
|---|---|---|---|
| Age in years, median (IQR) | 41 (34–50) | 42 (36–49) | 41 (35–49) |
| Males/females; % | 57/43 | 54.1/45.9 | 55.3/44.7 |
| Physicians/nurses; % | 74.9/25.1 | 55.8/44.2 | 63.6/36.4 |
| Experience in years | |||
| Up to 10 years; % | 40.8 | 39.3 | 39.9 |
| From 11 to 20 years; % | 29.2 | 45.5 | 38.9 |
| Over 20 years; % | 30.0 | 15.2 | 21.2 |
| Out-hospital working unit | |||
| MEU; % | Not applicable | 74.9 | |
| RIV; % | Not applicable | 6.2 | |
| PCES/HCU; % | Not applicable | 18.9 | |
| In-hospital workplace | |||
| Emergency; % | 17.9 | Not applicable | |
| ICU/IC/CU; % | 65.6 | Not applicable | |
| Resuscitation; % | 8.1 | Not applicable | |
| Hospitalization; % | 8.4 | Not applicable | |
| Participates in the hospital CPA response team? | |||
| Yes; % | 66.8 | Not applicable | |
| No; % | 33.2 | Not applicable | |
IC: intermediate care; CPA: cardiopulmonary arrest; IQR: interquartile range; PCES: primary care emergency service (non-home, out-hospital emergency services); HCU: home care unit (vehicle with physician or nurse, but not both); CU: coronary unit; ICU: Intensive Care Unit; MEU: mobile emergencies unit (medical ambulance, nurse and one or two technicians); RIV: rapid intervention vehicle (vehicle with physician, nurse and technician).
A comparative analysis was made of the influence of the characteristics of the possible resuscitators based on the chi-squared test and a two-phase cluster analysis seeking natural data set clustering, using log-likelihood statistics and the Bayesian information criterion (BIC) as cluster algorithm.
A total of 1000 responses were obtained. The characteristics of those surveyed are reported in Table 1. Sixty-six percent would not perform CPR upon arrival of the ES after more than 15min without CPR. This figure reached 86.7% if the time without CPR exceeded 20min. If basic CPR maneuvers had been started, these figures decreased to 14.9% and 43.8%, respectively. Age was not regarded as a reason for not starting CPR by 65.3% of those surveyed, and 72.5% would not start maneuvers in the case of terminal illness. In turn, 62.4% would not perform CPR in the presence of severe disability, while 19.6% did not consider this to be a reason for not starting CPR. On the other hand, 48.8% would not start CPR in the presence of DNR orders as presented by the family; 27.8% would not start CPR in response to express indication by the family of a patient wish against resuscitation; and 10.8% would not start CPR simply if so instructed by the family. Suicide was not considered a reason not to start CPR, while 36% would not start maneuvering in the presence of DNR orders (Table 1 ESM).
As to whether the surveyed professionals would perform CPR when not indicated, 18.7% stated that they would do so often or almost always. The cited reasons for performing CPR even when not indicated, in very few cases, never or almost never were environmental pressuring (53.5%), training (73.4%), teaching (69.0%), encountering staff performing basic CPR (68.3%), pediatric patients (34.9%), young victims (36.0%) and pregnant women (34.7%). In these latter three circumstances, 33.7%, 28.8% and 33.3%, respectively, would almost always perform resuscitation (Table 2 ESM).
The female participants in the survey (mostly nurses) showed a greater tendency to perform CPR in situations of terminal illness or poor basal condition, and also to perform CPR even when not indicated, in response to environmental pressuring and in the case of children, young victims or pregnant women. In accordance to teaching, the male participants were more inclined to perform CPR even when not indicated (Table 1 ESM).
In the out-hospital setting, the age of the victim was less of a conditioning factor for starting CPR, and the professionals proved more demanding when it came to requesting DNR orders, while in the in-hospital setting the intention to start CPR was greater, even in the presence of terminal illness. There was a greater incidence of affirmative answers for starting CPR in the out-hospital setting, even when maneuvering was not indicated – the causes being environmental pressuring, team training, the performance of basic CPR, and pediatric, young or pregnant victims (Table 2 ESM).
The responders of the survey with less experience would start CPR more often in extreme circumstances, without prior CPR and after a longer elapsed period of time – the causes being environmental pressuring, team training, and pediatric or young victims. Those with greater experience were comparatively less inclined to start maneuvering when not indicated (Tables 3 and 4 ESM).
The age of the participants showed differences. Those of younger age would start CPR more often, even if a longer time had elapsed after CPA, if CPR had not been started, and if there were no DNR orders. These professionals were also more inclined to perform maneuvering even when not indicated, due to training, teaching, and in the case of young victims (Table 4 ESM).
Although it would seem evident that CPR would not be indicated in terminal disease, the data obtained indicate that in such situations 72.5% of those surveyed would not start CPR. With regard to the prior condition of the patient, and although this factor was taken into account by 92% of those surveyed,2 it was not regarded as a conditioning element by 19.6%, and 37.6% would start maneuvers in patients with severe or total disability (Table 5 ESM).
These findings suggest that the general characteristics of the resuscitators, as well as age, gender, profession and experience, influence the attitudes towards CPR. In this respect, in general, women, out-hospital nurses, professionals with less experience and younger staff would be more inclined to perform CPR even when the indications are questionable – with the observation of a certain disparity of criteria among the professionals assisting CPA as to whether to start maneuvering or not.
It is advisable to establish clear recommendations or protocols for starting or not starting CPR in the event of CPA,8 where the decision making process is influenced not only by the personal perspectives of the resuscitators but also by strict criteria such as the characteristics of CPA and of the patient, the place where CPA takes place, and the medical-legal implications involved.4,9,10
In conclusion, although the opinions regarding the reasons for not starting CPR were consistent and predominant, disparity was observed in the responses regarding the performance of CPR when not indicated. The ethical recommendations in CPR are not duly taken into account by many professionals, with the criteria being based more on personal values. This shows that it will not be easy to consolidate uniform attitudes among resuscitators performing CPR under similar conditions.
Please cite this article as: Navalpotro-Pascual JM, Lopez-Messa JB, Fernández-Pérez C, Prieto-González M. Actitudes de los profesionales sanitarios ante la resucitación cardiopulmonar. Resultados de una encuesta. Med Intensiva. 2020;44:125–127.