Continuous positive airway pressure (CPAP) is an important therapeutic tool in COVID-19 acute respiratory distress syndrome (ARDS) since it improves oxygenation, reduces respiratory rate and can prevent intubation and intensive care unit (ICU) admission. CPAP during pronation has seldom been described and never during sedation.
DesignCase series.
SettingHigh dependency unit of San Carlo University Hospital (Potenza, Italy).
PatientsEleven consecutive patients with COVID-19 ARDS.
InterventionHelmet CPAP in prone position after failing a CPAP trial in the supine position.
Main variable of interestData collection at baseline and then after 24, 48 and 72h of pronation. We measured PaO2/FIO2, pH, lactate, PaCO2, SpO2, respiratory rate and the status of the patients at 28-day follow up.
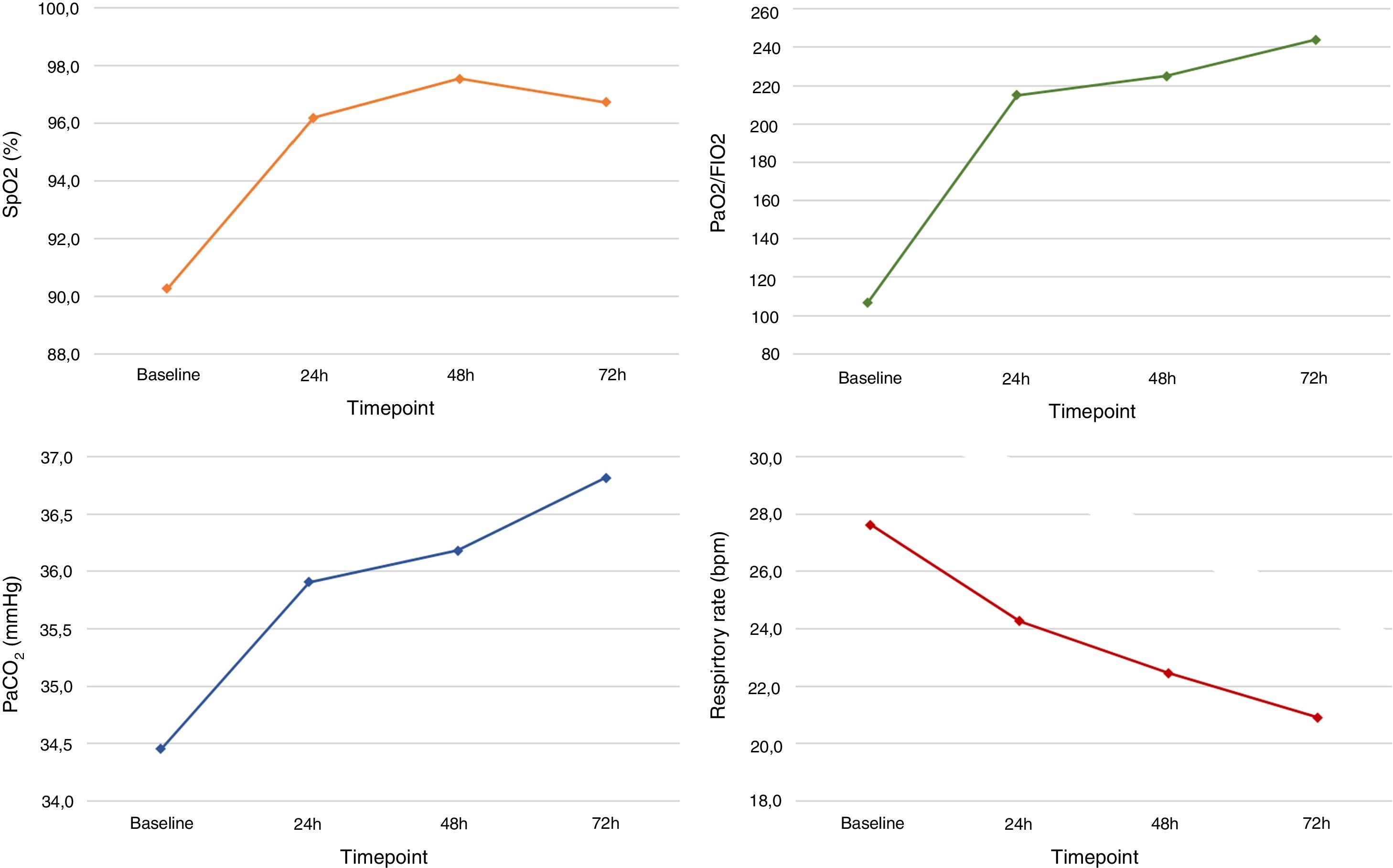
ResultsPatients were treated with helmet CPAP for a mean±SD of 7±2.7 days. Prone positioning was feasible in all patients, but in 7 of them dexmedetomidine improved comfort. PaO2/FIO2 improved from 107.5±20.8 before starting pronation to 244.4±106.2 after 72h (p<.001). We also observed a significantly increase in Sp02 from 90.6±2.3 to 96±3.1 (p<.001) and a decrease in respiratory rate from 27.6±4.3 to 20.1±4.7 (p=.004). No difference was observed in PaCO2 or pH. At 28 days two patients died after ICU admission, one was discharged in the main ward after ICU admission and eight were discharged home after being successfully managed outside the ICU.
ConclusionsHelmet CPAP during pronation was feasible and safe in COVID-19 ARDS managed outside the ICU and sedation with dexmedetomidine safely improved comfort. We recorded an increase in PaO2/FIO2, SpO2 and a reduction in respiratory rate.
La ventilación con presión positiva continua (CPAP) es una opción terapéutica útil en pacientes con síndrome de dificultad respiratoria aguda (SDRA) secundaria a infección por coronavirus 2019 (COVID-19) porque mejora la oxigenación, disminuye la frecuencia respiratoria y puede prevenir la intubación orotraqueal y así la admisión en la unidad de cuidados intensivos (UCI). El uso de la CPAP en pronación se ha descrito raramente, y nunca en pacientes con sedación superficial.
DiseñoSerie de casos.
ÁmbitoUnidad de cuidados intensivos del Hospital San Carlo (Potenza, Italia).
PacientesOnce casos consecutivos de pacientes con SDRA secundario a infección por COVID-19.
IntervencionesCasco y CPAP y en posición de prono, después de fracasar una sesión de una hora de CPAP en posición supina.
Variables de interés principalesDatos clínicos registrados antes de iniciar la primera sesión de 12h de pronación y a las 24, 48 y 72h. Los datos registrados fueron PaO2/FiO2, pH, lactatos, PaCO2, SpO2, frecuencia respiratoria y visita de seguimiento a los 28días.
ResultadosTodos los pacientes fueron tratados con CPAP y casco durante una media ±DE de 7±2,7. La posición de prono se realizó con éxito en los 11 pacientes, pero 7 pacientes recibieron dexmetodomidina para mejorar el confort.
El valor de PaO2/FiO2 mejoró desde 107,5±20,8 antes de la pronación hasta 244,4±106,2 después de 72h (p<0,001). Se observó un aumento significativo de la SpO2 desde un basal de 90,6±2,3 hasta 96±3,1 a las 72h (p<0,001) y una reducción de la frecuencia respiratoria desde 27,6±4,3 hasta 20,1±4,7 (p=0,004). No se observaron diferencias en los valores de PaCO2 o de pH. A los 28días dos pacientes habían fallecido, uno permanecía todavía ingresado en la planta después de la dimisión de la UCI y ocho fueron remitidos al domicilio después de ser tratados en la planta sin necesidad de ingreso en la UCI.
ConclusionesLa CPAP con casco durante la posición de prono fue segura y eficaz en pacientes con SDRA secundario a COVID-19 en la planta, y el uso de dexmetodomidina mejoró el confort. Se observó una mejora en los valores de PaO2/FiO2, de SpO2 y de la frecuencia respiratoria.
A relevant part of patients affected by coronavirus disease 19 (COVID-19) develops mild to severe acute respiratory failure (ARF).1,2 Continuous positive airway pressure (CPAP) has been proposed as a simple, potentially effective tool to improve oxygenation and to avoid tracheal intubation.3,4 Helmet could be the best choice as interface, to minimize the risk of viral spreading to health care workers and other patients while offering the best comfort.4,5 Moreover, CPAP use in ordinary wards is a well-established practice, a valuable possibility when intensive care units (ICU) are overcrowded like during the COVID-19 pandemic.6–10
Prone positioning proved effective in reducing mortality in ARDS invasively ventilated patients,11 and has been proposed also for COVID-19 ARDS.12 Its beneficial effects have been attributed to several mechanisms including recruitment of dorsal lung areas with improved ventilation/perfusion ratio and reduction of ventilation induced lung injury (VILI).13 The reduced difference in transpulmonary pressure between dorsal and ventral regions, makes ventilation more homogeneous, thus limiting alveolar overdistension and collapse.14 Moreover, pronation can reverse the atelectasis caused by the heart, in particular on the left lower lobe.15 Finally, diaphragm's displacement caudally decreases posterior compression of the lung, especially in obese patients.16
Prone positioning can also be applied in awake, spontaneously breathing patients treated by CPAP, both as a standard or as rescue treatment.8,17 So far, very few reports were published on this issue; moreover, no sedative strategy to improve patients’ compliance to the treatment was reported. In the present study we describe our experience with helmet CPAP and pronation during the COVID-19 pandemic, also reporting on the use of dexmedetomidine to increase tolerance to prone positioning.
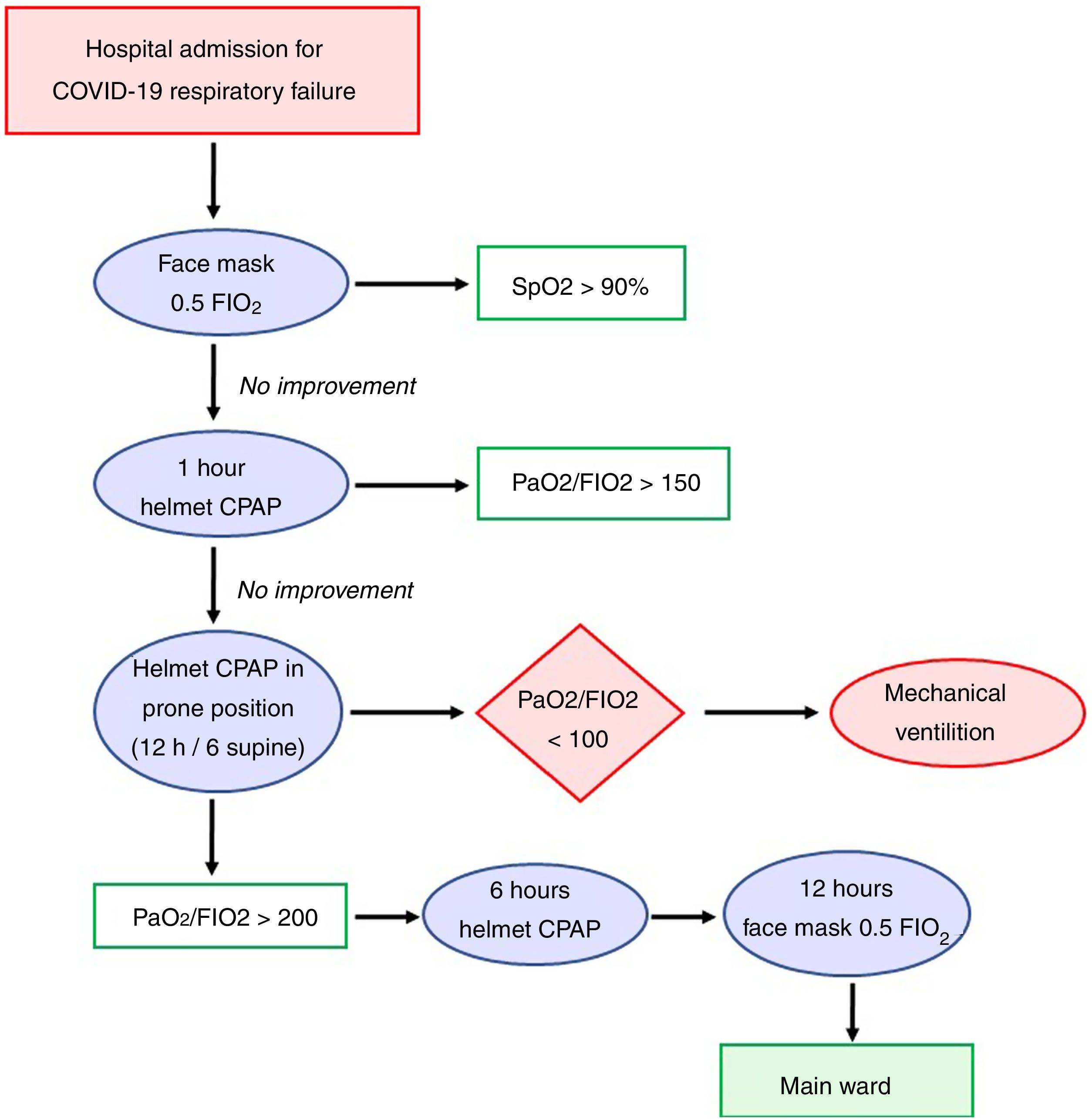
MethodsThis was a single center study conducted in San Carlo University Hospital (Potenza, Italy) between April 1st and May 1st 2020. The hospital was reshaped to be the only COVID-19 hospital of an area with half million inhabitants in South Italy during the pandemic as per Health Ministry indication: the ICU beds increased from 23 to 39 and were dedicated to invasively ventilated COVID-19 patients; the six high dependency unit (HDU) beds were dedicated to patients with helmet CPAP and jointly managed by emergency and intensive care physicians; the main infectious disease 38 bed ward was dedicated to patients who were in spontaneous breathing, eupneic, and with peripheral oxygen saturation (SpO2)≥90% while receiving oxygen by face mask with a fraction of inspired oxygen (FIO2) of 0.5. The diagnosis of COVID-19-related pneumonia was performed with both a positive swab test and a suggestive CT scan.
In this study we collected data of all consecutive adult patients with COVID-19 ARDS who failed a one-hour helmet CPAP trial in supine position, with a persistent arterial partial pressure of oxygen/fraction of inspired oxygen (PaO2/FIO2)<150. To avoid intubation (due to ICU bed scarcity and reports of poor outcome of COVID-19 invasively ventilated patients), if patients did not improve they received helmet CPAP in prone position: Twelve hours helmet CPAP in prone position were followed by six hours helmet CPAP in supine position. We did not consider pronation in case of excessive cough, hypotension, morbid obesity or patient refusal. Intubation and transfer to the intensive care unit were performed in case of PaO2/FIO2<100 and dyspnea.
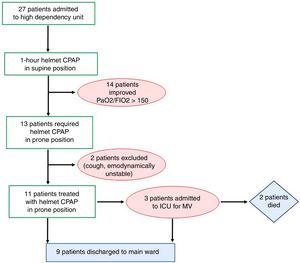
After the third pronation cycle, with a PaO2/FIO2>200 pronation was stopped and oxygen by face mask was delivered with an FIO2 of 0.5 for 48h. The patient was discharged to the main ward when hemodynamically stable with a SpO2>95%, respiratory rate (RR)<20 and without dyspnea. The protocol adopted in our instituted is presented in Fig. 1.
Since pronation with the helmet can be uncomfortable for the patient, dexmedetomidine (dose: 0.7–1.2mcg/kg/min without starting bolus) was administered in case of poor compliance to the treatment.
Along with baseline characteristics, data collection included: SpO2, PaO2/FIO2, arterial partial pressure of carbon dioxide (PaCO2), pH, RR, and arterial lactate. Variables were recorded at 4 time points on CPAP treatment: immediately before prone position, at 24, 48 and 72h. Need for ICU admission and 28-days mortality were collected.
Standard monitoring applied to all patients included: SpO2, electrocardiography, invasive blood pressure, body temperature and RR. A central venous catheter was inserted through the right internal jugular vein.
In our institute standard severe acute respiratory syndrome coronavirus 2 (SARS COV-2) protocol treatment included: hydroxychloroquine (400mg on first day, than 200mg per day), piperacillin/tazobactam (4.5g per day), acetylcysteine (300mg 3 times a day), remdesivir (150mg on first day, than 100mg for 10 days) and tocilizumab (4–8mg/kg once).
Ethical Committee approval was waived according to Italian law due to the retrospective and anonymized data collection.
Data are expressed as mean (±standard deviation) or number (percentage). Descriptive statistics were performed with STATA 16 and figures with Microsoft Excel 13. Variables were compared with unpaired t-test and statistical significance was assumed for p value less than 0.05.
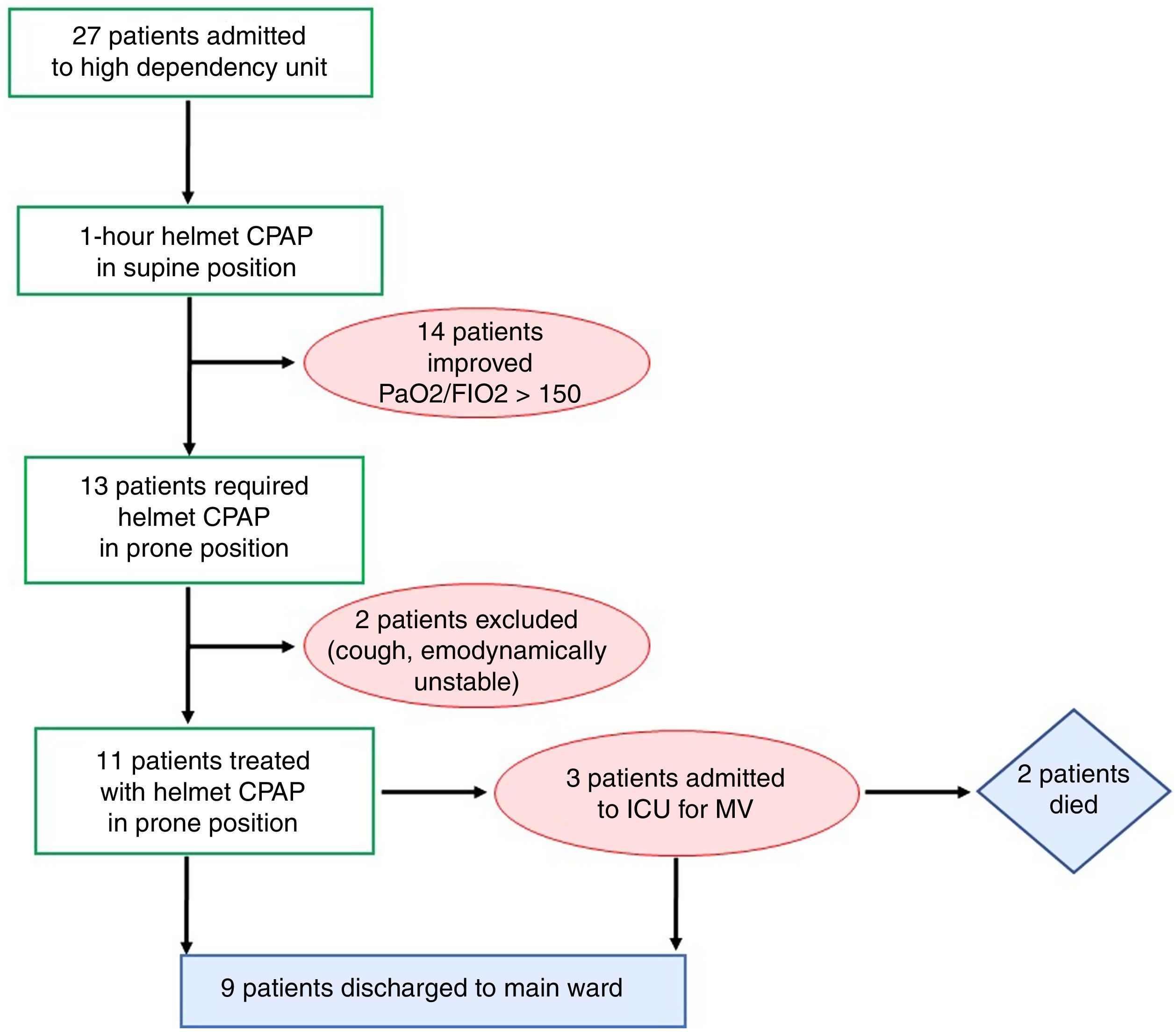
ResultsDuring the one-month study period, 27 out of the 81 patients hospitalized for SARS-COV-2 in our hospital were admitted in the high dependency unit to receive helmet CPAP for COVID-19 ARDS. Among these, 13 patients had PaO2/FIO2<150 after one hour with helmet CPAP in supine position. Two of these patients did not start helmet CPAP treatment in the prone position nor dexmedetomidine for cough and for hemodynamic instability respectively. Of the 11 consecutive patients who started helmet CPAP in the prone position, no patients interrupted helmet CPAP due to discomfort and no complications were observed during pronation sessions.
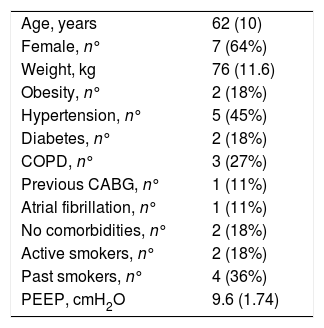
The 11 patients were treated for 7±2.7 days with a positive end expiratory pressure (PEEP) of 9.6±1.7cmH2O and pronation cycles of 13±1.2h duration. Patients were 62±10years old, seven were female and weighted 76±11.6kg. The most common comorbidity was hypertension (Table 1).
Baseline characteristics of the 11 patients who received helmet CPAP during pronation.
| Age, years | 62 (10) |
| Female, n° | 7 (64%) |
| Weight, kg | 76 (11.6) |
| Obesity, n° | 2 (18%) |
| Hypertension, n° | 5 (45%) |
| Diabetes, n° | 2 (18%) |
| COPD, n° | 3 (27%) |
| Previous CABG, n° | 1 (11%) |
| Atrial fibrillation, n° | 1 (11%) |
| No comorbidities, n° | 2 (18%) |
| Active smokers, n° | 2 (18%) |
| Past smokers, n° | 4 (36%) |
| PEEP, cmH2O | 9.6 (1.74) |
Values are presented as mean (SD) or number (%). CABG: coronary artery bypass graft, COPD: chronic obstructive pulmonary disease, PEEP: positive end-expiratory pressure.
Dexmedetomidine was administered in seven (63.6%) patients to improve compliance to pronation without episodes of hypotension or bradycardia or other adverse events related to dexmedetomidine administration.
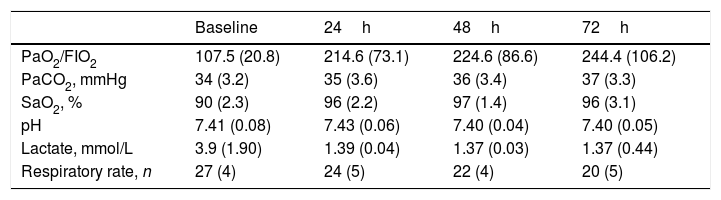
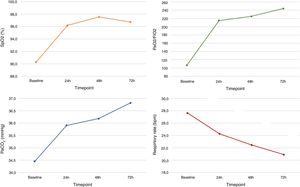
Blood gas analysis values and ventilation parameters are presented in Table 2 and Fig. 2. Mean SpO2 was 90±2.3% at baseline and improved to 97±3.1% at 72h (p<.001), meanwhile RR decreased from 27±4.3bpm to 20±4.7bpm (p=.004). At baseline mean PaO2/FIO2 was 107.5±20.8 and improved to 244.4±106.2 at 72h (p<.001). No significant differences were observed for PaCO2 pH and lactate.
Blood gas analyses results and respiratory rate at baseline and during CPAP at 24, 48 and 72h.
| Baseline | 24h | 48h | 72h | |
|---|---|---|---|---|
| PaO2/FIO2 | 107.5 (20.8) | 214.6 (73.1) | 224.6 (86.6) | 244.4 (106.2) |
| PaCO2, mmHg | 34 (3.2) | 35 (3.6) | 36 (3.4) | 37 (3.3) |
| SaO2, % | 90 (2.3) | 96 (2.2) | 97 (1.4) | 96 (3.1) |
| pH | 7.41 (0.08) | 7.43 (0.06) | 7.40 (0.04) | 7.40 (0.05) |
| Lactate, mmol/L | 3.9 (1.90) | 1.39 (0.04) | 1.37 (0.03) | 1.37 (0.44) |
| Respiratory rate, n | 27 (4) | 24 (5) | 22 (4) | 20 (5) |
Values are presented as mean (SD). FIO2: inspired fraction of oxygen, SaO2: arterial oxygen saturation, PaO2: arterial partial pressure of oxygen.
Trend of mean parameters at four time points: before pronation, 24, 48 and 72h after starting pronation. Values are presented as mean. FIO2: fraction of inspired oxygen, PaCO2: arterial partial pressure of carbon dioxide, PaO2: arterial partial pressure of oxygen, SpO2: peripheral oxygen saturation.
At the 28 days follow up overall survival was 82%: eight patients were discharged home and three patients admitted to ICU for invasive mechanical ventilation. Among these, two died of multiple organ failure and one was discharged to main ward after nine days. These results are summarized in Fig. 3.
DiscussionIn our experience conducted in a HDU managed by emergency physicians and intensivists, helmet CPAP in prone position resulted feasible and safe. Moreover, the infusion of dexmedetomidine to improve patients’ compliance to pronation was well tolerated. No complication was observed in any of the pronation sessions. The failure rate (need of invasive ventilation) was relatively low (27%) considering that pronation was used as a rescue treatment in hypoxic COVID-19 ARDS patients failing supine-only CPAP. More importantly, the 28-day survival rate (82%) was high.
Mortality rate in patients requiring tracheal intubation and mechanical ventilation for COVID-19 ARF are reportedly quite high, approaching 100% in many studies.2,18,19 Furthermore, tracheal intubation can be dangerous for patients and healthcare workers.20,21 Hence, treatments to avoid tracheal intubation are valuable and potentially life-saving.3,22,23 CPAP already proved effective in several forms of ARF,9,10 and its application for COVID-19 ARF has been proposed.3,4 The use of the helmet as interface seems logical, as it can improve comfort and minimize air leakage (potentially a source of infection for other patients and healthcare workers).4,5 A very limited number of studies on helmet CPAP use for COVID-19 ARF is available.6,7
A hot topic is whether prone position could enhance the efficacy of oxygen therapy or helmet CPAP in COVID-19 pneumonia, further reducing the risk of tracheal intubation and finally improving the survival rate. Thompson et al. reported its application in 25 spontaneously breathing patients treated by standard oxygen therapy: in all cases oxygenation improved at one-hour time-point. Interestingly, the intubation rate was lower in case of patients’ SpO2 improvement above 95% after one-hour pronation.24 Elharrar et al. reported on 24 patients treated with oxygen therapy: at 10-day follow-up five of them had been intubated.25 In the context of noninvasive ventilation (NIV), Villareal-Fernandez et al. applied prone positioning in six severely hypoxemic patients while treated with NIV or high-flow nasal cannula: four avoided tracheal intubation.22 Sartini et al. applied pronation in 15 patients who had failed supine CPAP: at 14-day follow-up, one patient had been intubated and one had died.17 Finally one study evaluated pronation in 56 spontaneously breathing patients, a mixed population treated either with oxygen by face mask or NIV; only 47 actually were then pronated and 44 were treated with helmet CPAP. Thirteen patients were intubated and five deaths were observed at follow-up.8
Overall, only one complication was reported (an episode of emesis that required tracheal intubation),22 while refusal or intolerance were more common: 11% in the study by Coppo et al., 14% in the study by Thompson.8,24 Improving comfort and tolerance to prone positioning can be of high relevance, allowing longer session and ultimately reducing the risk of tracheal intubation. Accordingly, we administered an infusion of dexmedetomidine in seven patients. Dexmedetomidine is a α2-adrenoceptor agonist with sedative and anxiolytic effects; bradycardia and hypo- or hypertension are possible side-effects, but the respiratory function is commonly preserved. So far, its successful use in relation to COVID-19 ARF has been reported in a single case, for a patient intolerant to standard oxygen therapy.26 In our opinion dexmedetomidine could improve tolerance to helmet CPAP in prone position, provided that the treatments are performed in a well monitored setting like an HDU.
Limitations. None of the mentioned studies on helmet CPAP, including ours, was randomized, so the efficacy of the treatment is still unproved; on the other hand, CPAP efficacy has been demonstrated in the past in several other hypoxemic forms of ARF.5,9,10 Our study assessed a limited number of patients was assessed and larger studies are required to fully evaluate the safety of the treatment. Finally, the risk/benefit ratio of dexmedetomidine in this context requires a rigorous evaluation.
In conclusion, helmet CPAP in prone position for COVID-19 severely hypoxemic ARF resulted feasible and without complications; the infusion of dexmedetomidine to improve patients’ compliance to pronation was well tolerated. The survival rate was high, but the efficacy of the treatment must be evaluated in randomized trials.
Authors’ contributionsAll the authors equally contributed to the manuscript.
Conflict of interestThe authors have no conflict of interest to disclose.