The first description ever on the use of the prone position in non-intubated (PPNI) adult patients goes back over 15 years1 when it was used for the first time in 4 patients to avoid using invasive mechanical ventilation (IMV). The maneuver was well-tolerated, there were no complications, and none of the patients required IMV. These results suggested that the PPNI could be a useful option to improve the ventilation-perfusion ratio. Also, that its use could extend towards any etiology of respiratory failure with some degree of collapse of the dorsal regions in the supine position. Afterwards, other descriptive studies demonstrated that it is a well-tolerated maneuver that is often associated with better oxygenation.2 However, the response to the application of PPNI is heterogeneous and some patients just cannot remain in the prone position for extended periods of time, which can limit the effectiveness of treatment.
An important point should be to determine whether the physiological effects of the prone position described in patients intubated with acute respiratory distress syndrome (ARDS) is kept in patients with non-intubated acute hypoxemic respiratory failure (AHRF). If this were the case, it would seem reasonable to anticipate the same kind of benefit regarding the clinical outcomes. In this sense, data available today are favorable to the use of PPNI. A study that included healthy volunteers treated with high nasal flow (HNF) revealed that the prone position was associated with a more homogeneous distribution of ventilation.3 On the other hand, the presence of spontaneous breathing while in the prone position in patients with ARDS on IMV reduces both the inspiratory effort and transpulmonary pressure compared to the supine position.4 That is, the use of PPNI could have beneficial effects reducing patient-self inflected lung injury,5 which is one of the mechanisms of progression of preexisting lung lesion, and a clear determinant of the need for intubation for patients treated with any kind of non-invasive respiratory support.6
At the beginning of the pandemic due to SARS-CoV-2 (COVID-19), critical care units had an avalanche of patients that triggered fear on a possible lack of ventilators all patients who may need it. This made healthcare workers look for treatment strategies and alternative support measures to prevent intubation. The PPNI maneuver was proposed as one of these measures. We have been able to confirm that it is a feasible maneuver in most patients. However, the amount of time patients can keep the prone position is highly variable. Also, the improved oxygenation seen during the prone position only remains in some patients when they return to the supine position. This improved oxygenation did not predict the future need for IMV either.7
Beyond the physiological effects, it is also necessary to determine whether the use of PPNI is associated with a lower need for IMV or even if it can have some effect on mortality itself. In this sense, the very first analyses conducted on observational studies did not show any reductions in the need for intubation or in the mortality rate reported.8 Afterwards, the first few randomized studies conducted on this issue recruited a limited number of patients with very heterogeneous characteristics treated with different systems of non-invasive support9 making it impossible to determine the effect of PPNI on the need for intubation.
More recently, the results from a meta-analysis that included over 1000 patients with COVID-19 treated with HNF showed a reduction in the rate of treatment failure (defined as the need for intubation or death within the first 28 days after recruitment).10 This reduction was basically due to the lower need for intubation without any effects on mortality. Therefore, the number needed to treat (NNT) to prevent 1 intubation was only 14 patients (95%CI, 8–69). The use of the PPNI was not associated with a higher rate of adverse events. The duration of HNF therapy prior to intubation, mortality, the duration of IMV, and the length of stay of patients who needed IMV was similar in both groups. That is, the use of the PPNI did not delay the intubation of patients with unfavorable disease progression or worse prognosis.
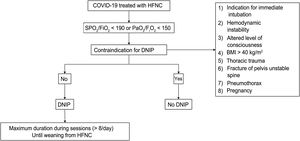
With these results, the obvious question is: should all patients with COVID-19 treated with HNF be placed in the prone position? To this date, the most probable answer to this question is yes (Fig. 1). And the answer is probably yes for different reasons. First, because it is a safe maneuver when performed correctly, in the proper setting, and with the proper monitorization. Secondly, because it can reduce the need for IMV of these patients. Thirdly, because there is no additional cost associated beyond the relative workload increase for the healthcare personnel. Also, this increase is relative if compared to the workload that the same patient could generate if intubated and connected to IMV. Last, but not least, because the use of PPNI could have beneficial effects at hospital level, not only for leaving more ventilators available to other patients, but also for saving the oxygen that it could produce. Let’s say that by using the PPNI we can reduce the fraction of inspired oxygen (FIO2) from 0.8 down to 0.6 in a patient treated with HNF at 60L/min. This reduction in the FIO2 would save around 30% in oxygen consumption. However, we should mention that it is necessary that these patients are properly monitored to detect clinical impairment as soon as it appears and avoid delayed intubation in patients with poor disease progression. Also, there are still many unsolved questions like if the effect of the PPNI is the same in non-COVID patients, what effect does the duration of the prone position have on the effectiveness of treatment or what coadjuvant strategies can favor that the patient remains longer time in the prone position, among others.
Proposal of algorithm to be used in the prone position in non-intubated patients with COVID-19. COVID-19, disease due to SARS-CoV-2; PPNI, prone position in non-intubated adult patients; FIO2, fraction of inspired oxygen; HFNC, high-flow nasal cannula; PaO2, arterial oxygen partial pressure; SpO2, oxygen saturation measured by pulse oximeter.
Despite of this, we can consider that the PPNI maneuver is safe, and its use could improve the prognosis of patients with acute respiratory failure. As a matter of fact, in patients with COVID-19 who require HNF it reduces the need for IMV. Also, when performed in a setting with proper monitorization it does not delay the intubation of patients with unfavorable progression or worsen prognosis either. Therefore, given the potential benefits reported, its easy implementation process, its safety profile, and low cost associated, the PPNI could be widely used in patients with COVID-19 who require support with HNF.
Conflicts of interestAuthors declare that they have no conflict of interest.
Please cite this article as: Pacheco-Reyes A, Garcia-de-Acilu M, Roca O, Decúbito prono más allá del paciente intubado: ¿tiene sentido? Medicina Intensiva. 2022;46:403–405.