To evaluate the clinical usefulness and safety of the differential-time-to-positivity (DTP) method for managing the suspicion of catheter-related bloodstream infection (CR-BSI) in comparison with a standard method that includes catheter removal in critically ill patients.
Methods-DesignA prospective randomized study was carried out. Setting: A 16-bed clinical-surgical ICU (July 2007-February 2009). Interventions: Patients were randomly assigned to one of two groups at the time CR-BSI was suspected. In the standard group, a standard strategy requiring catheter withdrawal was used to confirm or rule out CR-BSI. In the DTP group, DTP without catheter withdrawal was used to confirm or rule out CR-BSI. Measurements: clinical and microbiological data, CR-BSI rates, unnecessary catheter removals, and complications due to new puncture or to delays in catheter removal.
ResultsTwenty-six patients were analyzed in each group. In the standard group, 6 of 37 suspected episodes of CR-BSI were confirmed and 5 colonizations were diagnosed. In the DTP group, 5 of 26 suspected episodes of CR-BSI were confirmed and four colonizations were diagnosed. In the standard group, all catheters (58/58, 100%) were removed at the time CR-BSA was suspected, whereas in the DTP group, only 13 catheters (13/41, 32%) were removed at diagnosis, and 10 due to persistent septic signs (10/41, 24%). In cases of confirmed CR-BSI, there were no differences between the two groups in the evolution of inflammatory parameters during the 48hours following the suspicion of CR-BSI.
ConclusionsIn critically ill patients with suspected CR-BSI, the DTP method makes it possible to keep the central venous catheter in place safely.
Evaluar la utilidad clínica y la seguridad de la diferencia del tiempo de positivización (DTP) de hemocultivos en el manejo de la sospecha de bacteriemia asociada a catéter (BAC) comparándola con un método estándar que incluye la retirada de catéter en los pacientes de cuidados intensivos.
Métodos-diseñoEstudio prospectivo aleatorizado. Ámbito: UCI médico-quirúrgica de 16 camas (julio de 2007-febrero de 2009). Intervención: aleatorización en 2 ramas de los pacientes en el momento de la sospecha de BAC. Grupo estándar: estrategia clásica que requiere la retirada de catéter para descartar o confirmar la BAC; grupo DTP: método DTP sin retirada de catéter que confirma o descarta la BAC. Variables: datos clínicos y microbiológicos, tasas de BAC, recambios innecesarios de catéteres, complicaciones debidas al recambio de catéter o al retraso en el recambio de catéter.
ResultadosVeintiséis pacientes fueron estudiados en cada grupo. En el grupo estándar 6 de los 37 episodios de sospecha de BAC fueron confirmados y 5 colonizaciones de catéter fueron diagnosticadas. En el grupo DTP 5 de los 26 episodios de BAC fueron confirmados y 4 colonizaciones diagnosticadas. En el grupo estándar todos los catéteres (58/58, 100%) se retiraron en el momento de la sospecha de BAC, mientras que en el grupo DTP solo 13 catéteres (13/41, 32%) se retiraron en el momento del diagnóstico y 10 por persistencia de signos inflamatorios (10/41, 24%). En los casos de BAC confirmada no se encontraron diferencias en la evolución de los parámetros inflamatorios en las 48h que siguieron la sospecha de BAC.
ConclusionesEn los pacientes críticos con sospecha de BAC el método DTP permite mantener los catéteres venosos centrales de forma segura.
Catheter-related bloodstream infections (CR-BSI) are the most common type of nosocomial bloodstream infections; CR-BSI increase length of stay and morbidity, thus resulting in higher healthcare costs of care1.
Central venous devices are very common in the management of patients in intensive care units (ICU). Clinical suspicion of CR-BSI often requires catheter withdrawal and replacement because a definitive diagnosis can only be reached retrospectively by finding that blood cultures and catheter tip culture are positive for the same pathogen. However, suspected CR-BSI is finally confirmed in only 15% to 25% of withdrawn catheter2.
For this reason, several diagnostic methods (quantitative blood cultures, differential time to positivity, endoluminal brush, etc.) that do not require catheter withdrawal have been tested in recent years. The differential time to positivity (DTP) of blood cultures has been validated as an accurate diagnostic method of diagnosing CR-BSI that avoids unnecessary catheter withdrawal3–10. DTP is based on the presumption that if the infection originates in the catheter, the blood from the hub will have a higher bacterial load than in the peripheral blood. Therefore, cultures of blood obtained from the catheter hub will become positive faster than those obtained from peripheral blood.
In a previous study, we found the DTP method yielded 80% sensitivity, 99% specificity, 92% positive predictive value, and 98% negative predictive value compared with quantitative and semiquantitative cultures of the tip of the withdrawn catheter4.
In the current randomized study, we aimed to evaluate the clinical usefulness and safety of the DTP method of managing suspicion of CR-BSI in critically ill patients.
Material & methodsStudy designWe conducted a prospective randomized trial, assigning patients with suspected CR-BSI to one of two groups:11
- •
DTP group, in whom the DTP method was used to diagnose CR-BSI without catheter withdrawal.
- •
Standard group, in whom quantitative and semi-quantitative cultures of catheter tips requiring catheter withdrawal were used to diagnosis CR-BSI.
We hypothesized that using the DTP method to manage suspicion of CR-BSI in critically ill patients would allow the CVC to remain in place safely (i.e., without increasing morbidity and mortality due to delay in catheter withdrawal in cases of confirmed CR-BSI), thus avoiding unnecessary catheter replacement.
The primary outcome measure was reduction in the number of catheters withdrawn. Secondary outcome measures were morbidity and mortality due to delayed catheter withdrawal in the DTP group or to catheter exchange by a new puncture in the standard group.
The study was performed in a medical-surgical ICU from July 2007 to February 2009 and was stopped due to low enrollment; we calculated a sample size of 200 CR-BSI suspicions. Patients were randomly assigned to one of the two groups at the time CR-BSI was suspected. No antimicrobial catheters were used. The attending clinical team was aware of the assignment. The patient remained in the assigned group throughout the ICU stay.
EthicsThe hospital's ethics committee approved the study. Patients or family provided written informed consent on admission to the ICU. Patients remained anonymous.
PatientsAll patients admitted to the ICU who required a short-term CVC were eligible.
All catheters were placed at ICU admission. We excluded a) patients with hemodynamic instability at the time CR-BSI was suspected (Systolic arterial pressure<90mmHg or decrease ≥ 40mmHg, Mean arterial pressure<65mmHg or the need for vasoactive drugs or an increase>5 mcg/kg/min of dopamine or dobutamine or>0.25 mcg/Kg/min norepinephrine in the last 12h), b) immunodeficient patients, c) patients with endovascular devices, d) patients with positive blood cultures in the last 72h, and e) patients participating in other experimental studies. We also excluded specific catheters: pulmonary artery catheters, long-term catheters (≥ 30 days), and catheters with local signs of infections.
The attending medical team suspected CR-BSI when three conditions were present: new clinical symptoms of infection (temperature>37°C, white blood count (WBC)>11×109/L, increase in C-reactive protein (CRP) levels), catheters were in place for more than 96h, and other sources of infection were ruled out. Temperature, WBC, and CRP levels were also recorded during the following 48h after CR-BSI suspicion and randomization.
We followed a restricted randomization scheme using computer-generated blocks of 4 patients to ensure that sequential patients were distributed equally between groups. Group assignments with associated laboratory application form and case report form were placed in sealed opaque envelopes which were opened by the attending clinical team. Nurses collected samples and sent them to the microbiological laboratory as usual. Once randomized, the patient remained in the same group throughout his ICU stay.
InterventionsDTP groupSuspected CR-BSI was confirmed or ruled out as follows: Two serial blood samples (10ml each) obtained 30minutes apart from a peripheral vein were cultured in aerobic (5ml) and anaerobic (5ml) media. Additionally, one blood sample was obtained from the distal lumen (hub) of each catheter in place (first 5ml of blood after discarding non-hematological contents), and these samples were cultured in aerobic media at the same time as the first blood sample from the peripheral vein. All blood samples were sent to the microbiology laboratory simultaneously. Times to positivity of all the blood cultures were automatically registered (BacT/ALERT, bioMerieux; Durham, North Carolina, USA). CR-BSI was confirmed when peripheral and hub blood cultures were positive for the same microorganism (i.e., identical in species and antibiogram) and DTP ≥ 120min. When the pathogen isolated in a positive hub-blood culture differed from the one isolated in peripheral blood cultures or when the hub-blood culture was positive and peripheral blood cultures were negative, we diagnosed catheter colonization. Non-CR-BSI was diagnosed when peripheral blood cultures were positive and the hub-blood culture was either negative or positive for the same pathogen but DTP<120minutes.
If hemodynamic instability occurred after blood samples were obtained, the catheters were removed. When multiple pathogens were isolated, catheters were removed because we considered it impossible to determine DTP for each microorganism4. If cultures remained negative for 72h and signs of sepsis persisted, we removed catheters.
Standard groupSuspected CR-BSI was confirmed or ruled out as follows: Two serial blood samples (10ml each) obtained 30minutes apart from a peripheral vein were cultured in aerobic (5ml) and anaerobic (5ml) media.
Suspected catheters were withdrawn and their tips (3–5cm) were processed for quantitative and semiquantitative cultures. Positivity was defined as the growth of 103 colony forming units (CFU) per catheter segment according to Cleri's modified method for quantitative cultures12] and as 15 CFU per segment according to Maki's method for semiquantitative cultures13].
CR-BSI was confirmed when the microorganism isolated in a positive peripheral blood culture was identical in species and antibiogram to any catheter-tip culture by either the quantitative or the semiquantitative method.
Other diagnoses included catheter colonization (when blood cultures were negative but one of the catheter-tip cultures was positive by either the quantitative or semiquantitative culture method) and non-catheter-related bloodstream infection (non-CR-BSI) (when the pathogen isolated in peripheral blood cultures differed from all those isolated in the catheter-tip cultures or when catheter-tip cultures were negative).
Statistical analysisWe carried out a descriptive study of all variables, expressing qualitative variables as frequencies and percentages and quantitative variables as means and standard deviations.
To compare the two groups, we used the chi-square test for qualitative variables (clinical and microbiological variables, unnecessary catheter removals, and complications due to catheter replacement or to delay in catheter removal) and Student's t-test for quantitative variables (clinical variables, CR-BSI rates, catheter days, mortality).
All P values were based on two-tailed tests (level of significance, P<0.05).
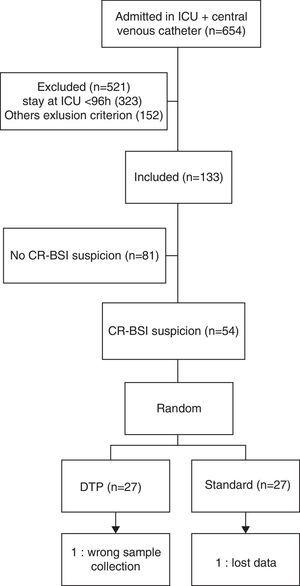
ResultsDuring the study period, 654 patients had CVCs during their ICU stay; 521 patients were initially excluded, most (323-62%) because their CVCs were in place<96h and no CR-BSI were suspected during their ICU admission.
Of the 133 initially included, 79 were not suspected of CR-BSI during their ICU admission. 54 patients were finally randomized at the time CR-BSI was suspected. Two were excluded from analyze due to errors in sample collection and lost data. Thus, we analyzed data from 26 patients in each group (Fig. 1).
The two groups were similar in terms of demographics and severity (77% males, 59 years±19, APACHE II 22±10) and in the insertion site and the time catheters have been in place (Table 1).
In the DTP group, we analyzed 26 episodes of suspected CR-BSI involving 41 catheters; each patient had an average of 1.5 catheters at the time CR-BSI was suspected. Five episodes were confirmed as CR-BSI and four were considered colonizations.
In the standard group, we analyzed 37 episodes of suspected CR-BSI involving 58 catheters; each patient had an average of 1.5 catheters at the time CR-BSI was suspected. Six episodes were confirmed as CR-BSI and five were considered colonizations.
The microorganisms that caused CR-BSI were Staphylococcus epidermidis (7 cases, 2 in DTP group and 5 in standard group), methicillin-resistant Staphylococcus aureus (MRSA) (1 case in DTP group), Pseudomonas aeruginosa (2 cases, one in both group), and Enterobacter cloacae (1 case in DTP group).
In the DTP group, we removed 13 catheters (13/41-32%) when CR-BSI was confirmed and ten (10/41-24%) in patients in whom signs of sepsis persisted 72h after samples were obtained although cultures remained negative. Thus, 18 (43.9%) catheters were maintained in the DTP group.
In the standard group, we removed all catheters (58/58-100%) at the time CR-BSI were suspected.
In cases of confirmed CR-BSI, comparison of inflammatory parameters during the 48h following the initial suspicion of CR-BSI found no differences between the DTP group in which the infected catheter remained in place until diagnosis and the standard group in which catheters were withdrawn at the time CR-BSI was suspected: CRP (0.4mg/dL±6 vs. 0.8mg/dL±3 p=0.86), WBC (14.05×109/L±21.05 vs. 12.01×109/L±20.90, p=0.94), increase in temperature (0.33°C±0.8 vs 0.84°C±0.7, p=0.27). Moreover, the use of vasoactive drugs in this period did not differ between the two groups (Table 2).
No catheters in the DTP group had to be removed because of hemodynamic instability following blood sample collection or because multiple pathogens were isolated in cultures. None of the catheter tips in the DTP group withdrawn because signs of sepsis persisted despite negative cultures for 72h turned out to be positive.
In the standard group, catheter exchange did not result in any major complications as pneumothorax, important hematoma or cardiac arrest (Table 3).
Results.
| DTP | STANDARD | P | |
|---|---|---|---|
| Patients | 26 | 26 | |
| Suspected CR-BSI episodes | 26 | 37 | |
| Catheters studied | 41 | 58 | |
| CR-BSI | 5 (19.2% suspected episodes) | 6 (16.2% suspected episodes) | 0.98 |
| Colonization | 4 (11.5% suspected episodes) | 5 (13.5% suspected episodes) | 0.88 |
| Catheters removed | 13 (32%) at diagnosis.10 (24%) persistent septic signs despite negative cultures for 72h | 58 (100%) | < 0.001 |
| Catheters related to CR-BSI or Colonization | 13 (32%) | 19 (32%) | 1 |
| Maintained catheters | 18 (43,9%) | 0 | <0.001 |
| Complications | 0 | 0 |
To our knowledge, this is the first randomized prospective study that compares a method for diagnosing CR-BSI that does not require catheter removal with a standard method that requires catheter withdrawal in short-term CVC. Our findings show that the DTP method makes it possible to maintain the CVC safely in critically ill patients with suspected CR-BSI.
Rijnders et al.14 compared immediate catheter removal with watchful waiting in ICU patients with suspected CR-BSI. The watchful waiting consisted of culturing two blood samples obtained from peripheral veins or through arterial catheter systematically within 48h whenever fever persisted. Catheters were removed if patients developed hemodynamic instability, if blood cultures became positive or after 5 days of observation if the attending physician still suspected CR-BSI. A major limitation of this study is that the only 8% of the patients included in the study had CR-BSI, whereas 25% of the patients excluded from the study had CR-BSI. The authors themselves pointed out that their exclusion criteria were not always based on hard clinical endpoints.
Most hospitals do not have the means for quantitative blood cultures but all have the means for the DTP method. The DTP method of diagnosing CR-BSI is reliable and is included in the latest Infectious Diseases Society of America guidelines for the diagnosis and management of intravascular catheter-related infection supported by IIa level of evidence15. This recommendation has been criticized because DTP is not widely used16 and because it is difficult to distinguish between false-positives and true infections in blood cultures17. The IIa level of evidence comes from two studies: a meta-analysis of eight prospective studies, only two of which included only short-term catheters in general ICU patients18, and a single-center study that found 81% sensitivity and 92% specificity for DTP against a gold standard of tip culture plus quantitative blood culture in cancer ill patients with short-term CVCs6.
Recent studies have supplied more evidence to validate DTP as an accurate and reliable method of diagnosing CR-BSI5,7. García et al.4 achieved sensitivity 80%, specificity 99%, positive predictive value 92%, and negative predictive value 98% for DTP compared to quantitative and semi-quantitative methods in patients in a medical-surgical ICU. The ROC curve analysis yielded a cut-off point of 17.7hours for positivity of hub blood cultures Based on the ROC cutoff and the high negative predictive value, they concluded that the probability of CR-BSI is low in cases with negative hub blood cultures within the first 24hours. Our results strongly support the safety and usefulness of the DTP method of diagnosing CR-BSI in in critically ill patients with short-term CVCs and strengthen the recommendations in the guidelines.
In the standard group, all catheters (58-100%) were replaced at the time CR-BSI was suspected. By contrast, in the DTP group only 13 catheters (32%) were replaced when CR-BSI was confirmed within 24h after sample collection and 10 (24%) were replaced after 72h when signs of sepsis persisted, although subsequent cultures of the tips were negative. In other words, 18 catheters (44%) were retained and 10 others (24%) could have been safely retained. Thus, if the DTP method had been strictly followed, it would have enabled 68% of the suspicious short-term CVCs to be safely retained in ICU patients. This percentage is similar to the 71% of negative cultures in catheters removed from patients with suspected CR-BSI in a series published by Rello et al.2
CR-BSIs are the most common type of nosocomial bloodstream infection in ICU patients, with an incidence ranging from three to five episodes per 1000 CVC days19–21. The incidence density of CR-BSI in our ICU during the study period was 2.67 episodes per 1000 CVC days. We attribute this low incidence to the implementation of a multiple-intervention protocol to reduce CR-BSI in the ICU during the same period. This protocol includes hand washing, using full-barrier precautions during CVC insertion, cleaning the skin with chlorhexidine, avoiding the femoral site if possible, and removing unnecessary catheters22,23.
Despite this low incidence, CR-BSI and colonization rates did not differ between the two groups: 6/37 (16.2%) suspected episodes of CR-BSI were confirmed in the standard group and 5/26 (19.2%) were confirmed in the DTP group.
The number of suspected CR-BSI was lower in the DTP group probably because of the need for removal when signs of sepsis persisted but blood cultures remained negative after 72h.
Our study has several limitations. First of all, the low enrollment, mainly due to the short ICU stay and to the implementation of a protocol to reduce CR-BSI that included daily checking of all the catheters to determine whether they were necessary. The planned sample size was 200 CR-BSI suspicions to find statistical differences but after a period of 20 months we only have included 54 and the trial was terminated.
Second, this study was done in a single center, so our results might not generalizable to other settings. In our ICU, protocols for CVC placement and management of suspected CR-BSI are strictly followed. We always exchange suspicious catheters by new puncture; we never use guidewires to exchange catheters in the same site. It would be interesting to see the results of a similar trial in other ICUs with different approaches to CVC management. It is interesting to note that we have had no difficulty in obtaining peripheral blood cultures often described as a limitation of the DTP method.
Third, we cannot eliminate bias introduced because the attending team was not blinded to the random assignation of patients to the two groups.
Finally, blood cultures and catheter cultures were compared exclusively by antimicrobial susceptibility testing as in usual clinical practice; we did not use biochemical and molecular identification, which provide more reliable identification, especially in coagulase negative staphylococcus24.
ConclusionsThe use of DTP in critically ill patients with suspected CR-BSI allows short-term CVCs to be retained safely in place.
Delay in catheter removal when DTP confirms CR-BSI does not increase morbidity.
Conflict of interestThe authors declare that they have no conflict of interest.
Special thanks to all residents and nurses at the critical care center of Hospital Parc Tauli for their collaboration.
This study was supported with a grant of the Research Institutional Comitee 2006, Fundació Parc Taulí, Sabadell, Spain.