Cardiac resynchronization therapy is a worldwide accepted technique to improve quality of life and reduce mortality in selected patients with congestive heart failure and reduced EF. Guidelines carefully define the patients for whom this technique is most likely to succeed.1 After many trials published we can say that a patient in NYHA class III, in sinus rhythm, left bundle branch block (LBBB), EF≤35%, QRS width≥120ms, with optimal medical therapy and non-ischemic cardiomyopathy will be an ideal case for CRT. However, some other groups of patients are also beneficiaries of the technique: ischemic cardiomyopathy, atrial fibrillation patients (AV node ablation required) (according to 2012 European Society of Cardiology Guidelines is indication IIb), NYHA class II and wide QRS with right bundle branch block.2,3 From the launching of CRT the technique has shown a significant proportion of non responders as high as 30%. To overcome this burden many echocardiography techniques have been proposed as predictors of CRT response. None of them were able to discriminate adequately responders from non-responders.4
Nevertheless echocardiography is paradoxically the cornerstone on which most studies rely to assess the improvement in heart failure symptoms. We provide a comprehensive follow-up protocol in order to supply a faster and convenient office review of CRT device carrier patients.
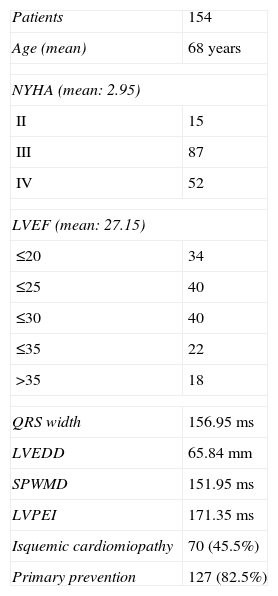
From March 1, 2006 until March 23, 2012 a total of 154 patients were implanted with a CRT device in our unit and entered into the follow-up protocol. Patient variables are shown in Table 1. Once the referral paper of a patient with a brief medical history was received in our unit the patient was scheduled for the first medical visit in the arrhythmia-CRT office.
Clinical and echocardiographic variables of patients.
| Patients | 154 |
| Age (mean) | 68 years |
| NYHA (mean: 2.95) | |
| II | 15 |
| III | 87 |
| IV | 52 |
| LVEF (mean: 27.15) | |
| ≤20 | 34 |
| ≤25 | 40 |
| ≤30 | 40 |
| ≤35 | 22 |
| >35 | 18 |
| QRS width | 156.95ms |
| LVEDD | 65.84mm |
| SPWMD | 151.95ms |
| LVPEI | 171.35ms |
| Isquemic cardiomiopathy | 70 (45.5%) |
| Primary prevention | 127 (82.5%) |
NYHA: New York Heart Association functional class; LVEF: left ventricle ejection fraction; LVTDD: left ventricle end diastolic diameter; SPWMD: septal-to-posterior wall motion delay; LVPEI: left ventricle pre-ejection interval. QRS, LVEDD, SPWMD, LVPEI expressed as mean values.
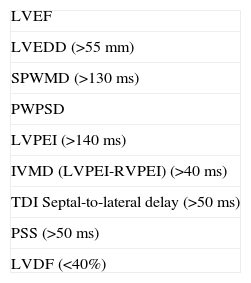
In the first office visit the patient was carefully assessed to establish NYHA class, etiology of the cardiomyopathy and co-morbidities as age, renal failure and peripheral arterial disease. Medical treatment was also registered. Electrocardiogram and echocardiography were performed. Although echocardiographic techniques are not included in CRT Guidelines, exception made for LVEF, atrioventricular (AV), interventricular and intraventricular dyssynchrony were fully determined (Table 2).5 These data are of major importance in order to adjust AV and VV pacing intervals in the follow-up visits.
Echocardiographic measures.
| LVEF |
| LVEDD (>55mm) |
| SPWMD (>130ms) |
| PWPSD |
| LVPEI (>140ms) |
| IVMD (LVPEI-RVPEI) (>40ms) |
| TDI Septal-to-lateral delay (>50ms) |
| PSS (>50ms) |
| LVDF (<40%) |
PWPSD: posterior wall post-systolic displacement as the difference of intervals from QRS onset to maximal systolic displacement of the LV posterior wall and from QRS onset to the beginning of E wave velocity; IVMD: interventricular mechanical delay as the difference of LVPEI and RVPEI (left and right ventricular pre-ejection interval); PSS: TDI post systolic shortening of left ventricle segments. LVDF: relation between mitral inflow pattern and heart cycle length.
After assessment patients were informed about the necessity or not of implanting a CRT device. In most of the cases the patients met Guidelines criteria for CRT. They were instructed about the technique in order to gain confidence and facilitate comprehension of what they would go through. This reassured patients and made them decide more accurately. Information about non-responders and the characteristics of the ideal candidate were also given. After informed consent was signed the patient was scheduled for intervention.
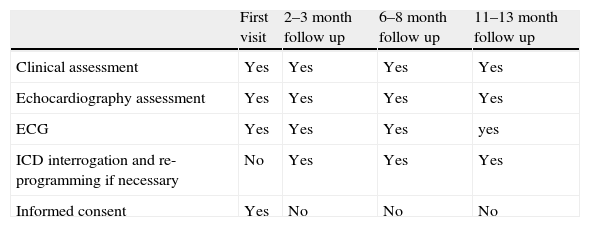
After device implantation on Fridays the patients stay for the week-end. On Saturday a chest X ray exploration and laboratory analysis are performed. The patients are permitted to get out of bed and walk in the hospital ward. On Monday, after routine device exam the patient is discharged home. They take the medical report and the date for the next medical visit within 3 months. On the first year after CRT, patients are assessed 3 times. In every one of these visits a 12-lead EKG, device exam and echocardiography are performed. We also register a clinical evaluation based on NYHA class. The echocardiographic measures and clinical evaluation give us important information to adjust the device parameters like VV and AV intervals. All the information is available for the clinical cardiologist in order to adjust medical treatment to his best knowledge. A schematic view of the protocol is displayed in Table 3.
A schematic view of the protocol.
| First visit | 2–3 month follow up | 6–8 month follow up | 11–13 month follow up | |
| Clinical assessment | Yes | Yes | Yes | Yes |
| Echocardiography assessment | Yes | Yes | Yes | Yes |
| ECG | Yes | Yes | Yes | yes |
| ICD interrogation and re-programming if necessary | No | Yes | Yes | Yes |
| Informed consent | Yes | No | No | No |
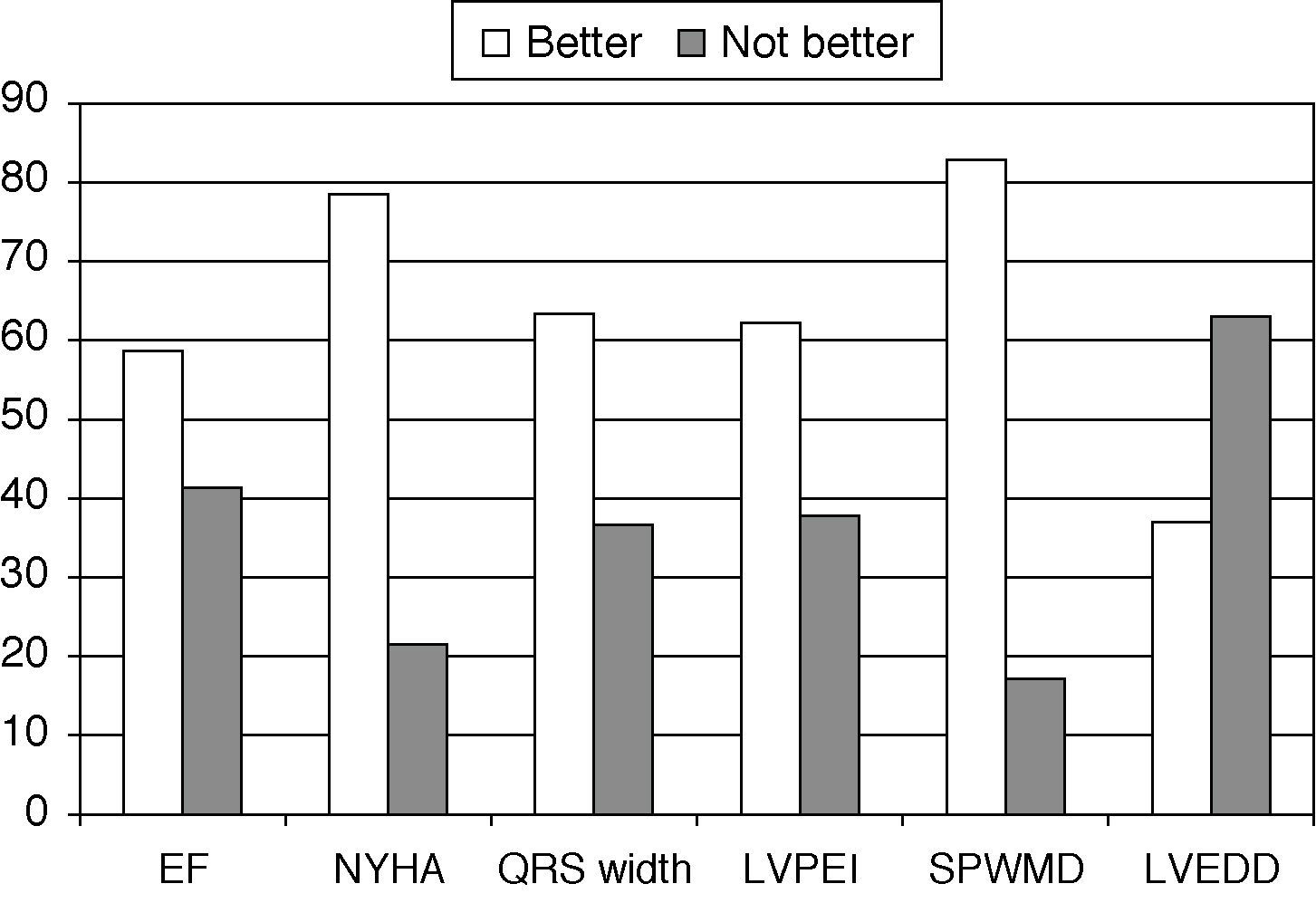
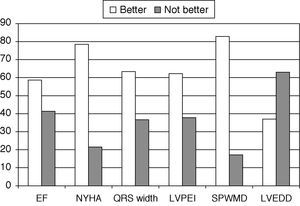
The proportion of patients who improved along the first year after device implantation are presented in Fig. 1. Six variables are displayed, EF, NYHA, QRS width, LVPEI, SPWMD and LVEDD. Although the proportion of patients who improved varies from 40%(LVEDD) to 80% (SPWMD) approximately, one sample t-test was used to compare basal and final results of the variables measured. The improvement measured in each one of the variables showed statistical significance (P<0.0001). These results are consistent with global literature on the outcome of CRT patients.
The proportion of patients who improved along the first year after device implantation. EF better: more than 5% increase measured; QRS width, LVPEI, SPWMD better: more than 10ms decrease measured; LVEDD better: more than 5mm decrease measured. All measures expressed in percentage of patients.
The satisfaction level of the patients was not assessed by any questionnaire. We cannot offer objective data in that particular issue. What we know is that patients stay 30–45min with the doctor in every CRT follow-up visit and that is much more of what they have ever spent in any other medical visit. That makes them feel well cared during the first year after resynchronization. Furthermore they do not need to arrange more than one medical visit for the follow-up of their device.
The implementation of this protocol was not intended to improve the proportion of responders to CRT therapy nor to enhance their clinical outcome. The aim of the protocol was showing how one physician in one office can examine the device, analyze the ECG and display echocardiographic techniques for comprehensive assessing of a CRT patient. The results are consistent with other series published.
The obvious limitation for this work is the lack of a control group with standard follow-up. Also, the satisfaction of patients was not assessed by a normalized questionnaire. Anyway, we wanted to point out the necessity of implementing innovative protocols in order to streamline the limited resources currently available in Europe. A vast proportion of our efforts must go in the direction of making medicine practice more efficient for Health Services while maintaining average level clinical results.
Please cite this article as: Luque-Lezcano AO, et al. Cardiac resynchronization therapy: 6 year experience of a comprehensive follow-up protocol. Med Intensiva. 2012. http://dx.doi.org/10.1016/j.medin.2012.10.004