To analyze the chronobiological and time variations of out-hospital cardiac arrest (OHCA).
DesignA retrospective descriptive study was made.
PatientsAll cases of OHCA of cardiac origin registered over 18months in the database of the emergency medical service (EMS) of the Autonomous Community of Castilla y León (Spain) were evaluated.
Variables analyzedAge, sex, recovery of spontaneous circulation (ROSC), first monitored rhythm (amenable/not amenable to defibrillation), alert site [home, public place, primary care (PC) center], alerting person (family, witness, law enforcement member, PC center staff), alert time (0–8; 8–16; 16–24), emergency team activation time, care time and day of the week. Univariate analysis (chi-squared), variance, and nonparametric tests comparing the variables in three periods of 8h. Chronobiological analysis by fast Fourier transform and Cosinor testing.
ResultsWe studied 1286 cases reported between January 2007 and June 2008. Statistically significant differences were observed in terms of younger age, higher incidence in the victim's home, and greater frequency of family-cohabiting persons as witnesses in the period between 0 and 8h. Chronobiological analysis found daily rhythm (circadian) with acrophase at 11.16h (p<0.001) and weekly rhythm (circaseptan) with acrophase on Wednesday (p<0.05). The median alert time-care time interval and emergency team activation time-care time were 11.7min and 8.0min, respectively, without differences between periods.
ConclusionsWe have demonstrated the presence of a daily rhythm of emergence of OHCA with a morning peak and a weekly rhythm with a peak on Wednesdays. These results can guide the planning of resources and improvements in response in certain time periods.
Analizar las características cronobiológicas y las variaciones temporales del paro cardiaco extrahospitalario (PCEH).
DiseñoEstudio descriptivo retrospectivo.
PacientesTodos los casos de PCEH de origen cardíaco registrados en la base de datos del servicio de emergencias médicas (SEM) de la Comunidad Autónoma de Castilla y León (España) durante 18 meses.
Variables de interés principalesEdad, sexo, recuperación de la circulación espontánea, primer ritmo monitorizado (desfibrilable /no desfibrilable), lugar de alerta [(hogar, lugar público, centro atención primaria (AP)], testigo (familiar, transeúnte, fuerzas de seguridad, personal AP), hora de alerta (0-8; 8-16; 16-24), hora de activación del equipo de emergencias, hora de atención y día de la semana. Análisis univariante mediante Chi2, varianza y tests no paramétricos. Análisis cronobiológico mediante transformada rápida de Fourier y test Cosinor.
ResultadosSe estudiaron 1286 casos registrados entre enero 2007 y junio 2008. Se observaron diferencias estadísticas significativas en menor edad (p<0,05), mayor incidencia en el hogar (p<0,001) y mayor frecuencia de familiares-convivientes como testigos (p<0,001) en el periodo de 0-8h. El análisis cronobiológico mostró ritmo diario (circadiano) con acrofase a las 11.16h. (p<0,001) y ritmo semanal (circaseptano) con acrofase en miércoles (p<0,05). Las medianas de intervalos alerta-atención y activación-atención fueron respectivamente 11,7min y 8,0min, sin diferencias entre periodos horarios.
ConclusionesSe demuestra la presencia de un ritmo diario de aparición del PCEH con pico matinal y un ritmo semanal con pico en miércoles. Estos resultados orientan al ajuste preventivo y a la planificación de recursos y mejoras en la respuesta, en determinados periodos horarios.
Out-hospital sudden cardiac arrest (OHCA) is a serious health problem. In Spain, the estimated annual incidence of OHCA is between 24,0001 and 50,000 cases,2 and the emergency medical services (EMS) play a crucial role in managing these patients. A cardiac origin of OHCA has been reported in over 80% of all cases,3 though some recent studies lower this percentage to about 60%.4
The measures adopted in recent years with the purpose of improving survival in patients with OHCA have focused mainly on the consolidation of EMS, the rapid activation of these services, witness-administered basic cardiopulmonary resuscitation, the diffusion and application of early defibrillation by both the EMS and non-medical emergency services, and the introduction of public access to defibrillation programs. However, adequate application of all these measures requires knowledge of the true situation of OHCA, determination of the response times of the installed devices, and knowledge of when and where they can be found.
Different studies5,6 have shown that in addition to myocardial infarction, other cardiovascular processes are also characterized by circadian variations in their appearance. The chronobiological analysis of a disease process allows us to determine its time of greatest incidence, and in contrast to acute myocardial infarction, this aspect has been little studied in the case of OHCA.7
Time variations have been described in cardiovascular event-triggering factors such as physical or psychological activity, environmental temperature, heart rate, blood pressure, sympathetic tone, fibrinolytic activity, platelet aggregation and even intrinsic peripheral vascular cell function.6,8–10
Time variations have also been demonstrated in the appearance of cardiac arrest, both during the day and over weekly or yearly periods.11,12 However, few studies have examined the influence of these variations upon patient survival,13–15 and none have used statistical methods specifically applied to chronobiological analysis. On the other hand, it has been shown that variations in EMS response times can influence mortality.16
Considering the above, analysis and knowledge of the chronobiological characteristics of OHCA, and the EMS response times, are of key interest as a basic source of information on the true situation of the process, and are useful in adopting preventive measures and in developing resource plans designed to offer a more adequate response.
The present study analyzes the chronobiological data and response times of the EMS referred to the OHCA cases registered in a Spanish Autonomous Community (Castilla y León), and their influence upon initial survival.
Patients and methodsType of studyA retrospective descriptive study was made of all the cases of OHCA registered in the database of the EMS of the Autonomous Community of Castilla y León (Spain) during an 18-month period between 1 January 2007 and 30 June 2008. Castilla y León is located in the north of Spain, with an area of 94,000km2 and a population of 2,563,521 inhabitants, as established by the January 2009 population census (www.ine.es). The database provides information on the characteristics of the patients, the interventions made, the alerting persons, the alert site, and the times referred to alert activation, interventions and patient transfer to a medical center, where applicable. Lastly, the database records the patient outcome after intervention or transfer to the hospital center in those cases where such transfer takes place. The EMS of Castilla y León has established a single telephone activation number (dial 112). The call is initially received by a general emergencies telephone operator, and is subsequently rerouted to the medical emergencies telephone operator. Activation of the EMS can be made by the Primary Care (PC) services, fundamentally in rural areas.
Inclusion and exclusion criteriaIn order to study the patients with out-hospital cardiac arrest of strongly suspected cardiological origin in which resuscitation attempts were made, we selected the cases with the following final diagnostic codes (ICD-9-CM): 427.4 and 427.41 (ventricular fibrillation), 427.5 (cardiac arrest), 798 (sudden death of unknown cause), 798.1 (sudden death), 798.2 (unexplained death in under 24h), 99.60 [cardiopulmonary resuscitation (CPR)], 99.62 (other cardiac electric shock) and 99.63 (cardiac massage), and registered the performance of resuscitation maneuvers.
Patients under 18years of age were excluded, as were those in which a non-cardiac cause was established, patients who had been dead for a prolonged period of time in which the time of death could not be established, cases involving a clear history of terminal or untreatable disease, and episodes with incomplete information or in which data could not be obtained from the witnesses to precisely establish an underlying cardiological cause.
Study variablesAn analysis was made of the following variables based on the Utstein model17: age, gender (male/female), outcome [death/recovery of spontaneous circulation (ROSC) and admission to hospital], first monitored rhythm (amenable/not amenable to defibrillation), alert site (home, public place, PC center), alerting witness or person [family or cohabitating person, passerby, law enforcement personnel (local or national/state police, private security), PC center personnel], alert time (dial 112), EMS emergency team activation time, emergency team care time at the alert site (defined as the time of arrival of the emergency care vehicle), and day of the week.
Analysis of the time intervals was based on the time data (hour and minute) referred to EMS alert (dial 112), activation and care. For the chronobiological analysis we used the time data (hour and minute and day of the week) referred only to the EMS alert (dial 112). In turn, the cases were grouped into three time periods of 8h each (0–8h, 8–16h, 16–24h), considering the three periods of usual activity (night, morning, afternoon), according to the EMS alert time (dial 112).
Statistical analysisA univariate comparative study was made using analysis of variance (ANOVA) and the nonparametric Kruskal–Wallis test for continuous variables and the chi-squared test in the case of categorical variables, comparing the different parameters with respect to the three 8-h time periods. The results are expressed as absolute values and percentages, means with the corresponding 95% confidence intervals (95%CI), and median times in minutes with the corresponding percentiles 25 and 75. Statistical significance was considered for p<0.05.
A time analysis was made of the distribution of the cases during the hours of the day, seeking a circadian rhythm in their incidence. For the chronobiological rhythmometric inferential statistical study, we consecutively used a “macroscopic” analysis based on assessment of the power spectrum curves using spectral analysis with the fast Fourier transform, and a “microscopic” analysis of the harmonics resulting from application of the Cosinor or cosine multiple test.
In the Fourier spectral analysis we conducted a systematic search of all the possible rhythms based on linear studies referred to both frequency and period. With the cosine multiple test, assessing different parameters such as acrophase and batyphase (acrophase: time corresponding to the maximum value of the variable in the adapted cosine curve; batyphase: time corresponding to the minimum value of the variable in the adapted cosine curve), in each of the cases and using the amplitude different from zero test, we determined the presence of statistical significance of the rhythm in each case. As determinants of the existence of rhythm, we took all harmonics with p<0.05 to be significant. A comparative analysis was thus made between the harmonics of the cases with an outcome corresponding to ROSC and death.
A similar time analysis was made of the distribution of cases during the days of the week, in search of a circaseptan rhythm.
The SPSS statistical package (SPSS, Inc., Chicago, IL, USA) was used for the univariate analysis, while the MATLAB program (MathWorks, Inc., Natick, MA, USA) was used in application to analysis of the time series.
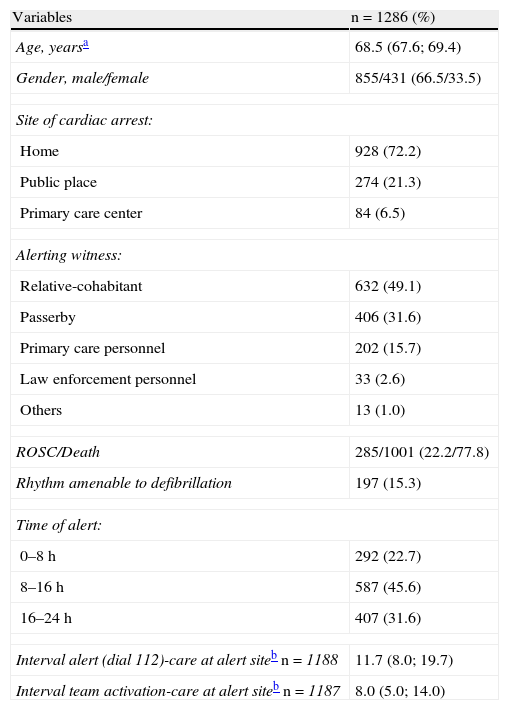
ResultsOf the 452,052 cases registered in the EMS database of Castilla y León during the 18months study period, we initially selected a total of 2018 cases corresponding to patients who had suffered cardiac arrest. Subsequently, application of the exclusion criteria led us to discard the following cases: 218 traumatisms, 123 other external causes, 251 non-cardiac medical causes, 24 patients under 18years of age, and 116 cases with insufficient data support. The final study sample thus comprised 1286 cases, the general characteristics of which are shown in Table 1.
General characteristics of the cases.
| Variables | n=1286 (%) |
| Age, yearsa | 68.5 (67.6; 69.4) |
| Gender, male/female | 855/431 (66.5/33.5) |
| Site of cardiac arrest: | |
| Home | 928 (72.2) |
| Public place | 274 (21.3) |
| Primary care center | 84 (6.5) |
| Alerting witness: | |
| Relative-cohabitant | 632 (49.1) |
| Passerby | 406 (31.6) |
| Primary care personnel | 202 (15.7) |
| Law enforcement personnel | 33 (2.6) |
| Others | 13 (1.0) |
| ROSC/Death | 285/1001 (22.2/77.8) |
| Rhythm amenable to defibrillation | 197 (15.3) |
| Time of alert: | |
| 0–8h | 292 (22.7) |
| 8–16h | 587 (45.6) |
| 16–24h | 407 (31.6) |
| Interval alert (dial 112)-care at alert siteb n=1188 | 11.7 (8.0; 19.7) |
| Interval team activation-care at alert siteb n=1187 | 8.0 (5.0; 14.0) |
Mean with 95% confidence interval.
Median with percentiles 25 and 75.
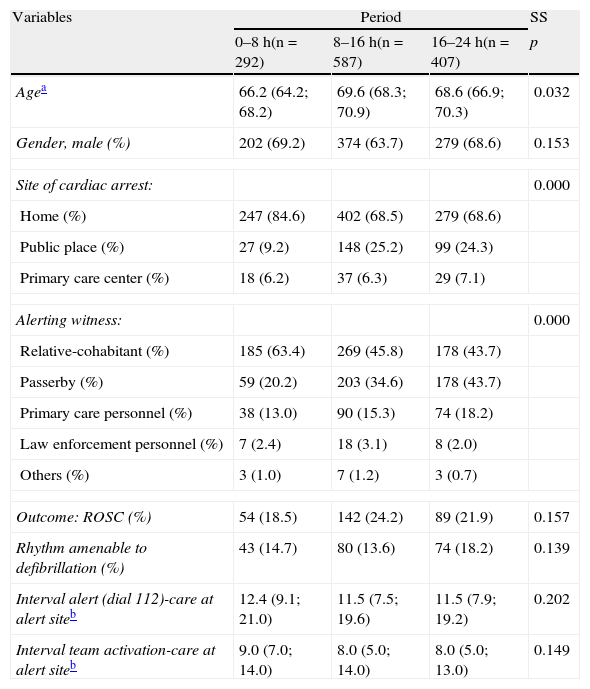
The univariate analysis revealed statistically significant differences in the form of older patient age, more frequent presentation in public places, and a greater frequency of passerby or PC personnel alert activation, in the cases occurring in the first and last of the three periods of the day (8–16h and 16–24h). In contrast, the cases manifesting in the nighttime hours (0–8h) involved comparatively younger patients, with a greater incidence in the home, and a greater frequency of alerts by relatives or cohabitating witnesses. There were no statistically significant differences among the three periods in terms of patient gender, first monitored rhythm, outcome or time intervals between alert and patient care at the alert site or team activation and patient care at the site (Table 2).
Comparisons according to the time period of out-hospital cardiac arrest.
| Variables | Period | SS | ||
| 0–8h(n=292) | 8–16h(n=587) | 16–24h(n=407) | p | |
| Agea | 66.2 (64.2; 68.2) | 69.6 (68.3; 70.9) | 68.6 (66.9; 70.3) | 0.032 |
| Gender, male (%) | 202 (69.2) | 374 (63.7) | 279 (68.6) | 0.153 |
| Site of cardiac arrest: | 0.000 | |||
| Home (%) | 247 (84.6) | 402 (68.5) | 279 (68.6) | |
| Public place (%) | 27 (9.2) | 148 (25.2) | 99 (24.3) | |
| Primary care center (%) | 18 (6.2) | 37 (6.3) | 29 (7.1) | |
| Alerting witness: | 0.000 | |||
| Relative-cohabitant (%) | 185 (63.4) | 269 (45.8) | 178 (43.7) | |
| Passerby (%) | 59 (20.2) | 203 (34.6) | 178 (43.7) | |
| Primary care personnel (%) | 38 (13.0) | 90 (15.3) | 74 (18.2) | |
| Law enforcement personnel (%) | 7 (2.4) | 18 (3.1) | 8 (2.0) | |
| Others (%) | 3 (1.0) | 7 (1.2) | 3 (0.7) | |
| Outcome: ROSC (%) | 54 (18.5) | 142 (24.2) | 89 (21.9) | 0.157 |
| Rhythm amenable to defibrillation (%) | 43 (14.7) | 80 (13.6) | 74 (18.2) | 0.139 |
| Interval alert (dial 112)-care at alert siteb | 12.4 (9.1; 21.0) | 11.5 (7.5; 19.6) | 11.5 (7.9; 19.2) | 0.202 |
| Interval team activation-care at alert siteb | 9.0 (7.0; 14.0) | 8.0 (5.0; 14.0) | 8.0 (5.0; 13.0) | 0.149 |
SS: statistical significance.
Mean with 95% confidence interval.
Median with percentiles 25 and 75.
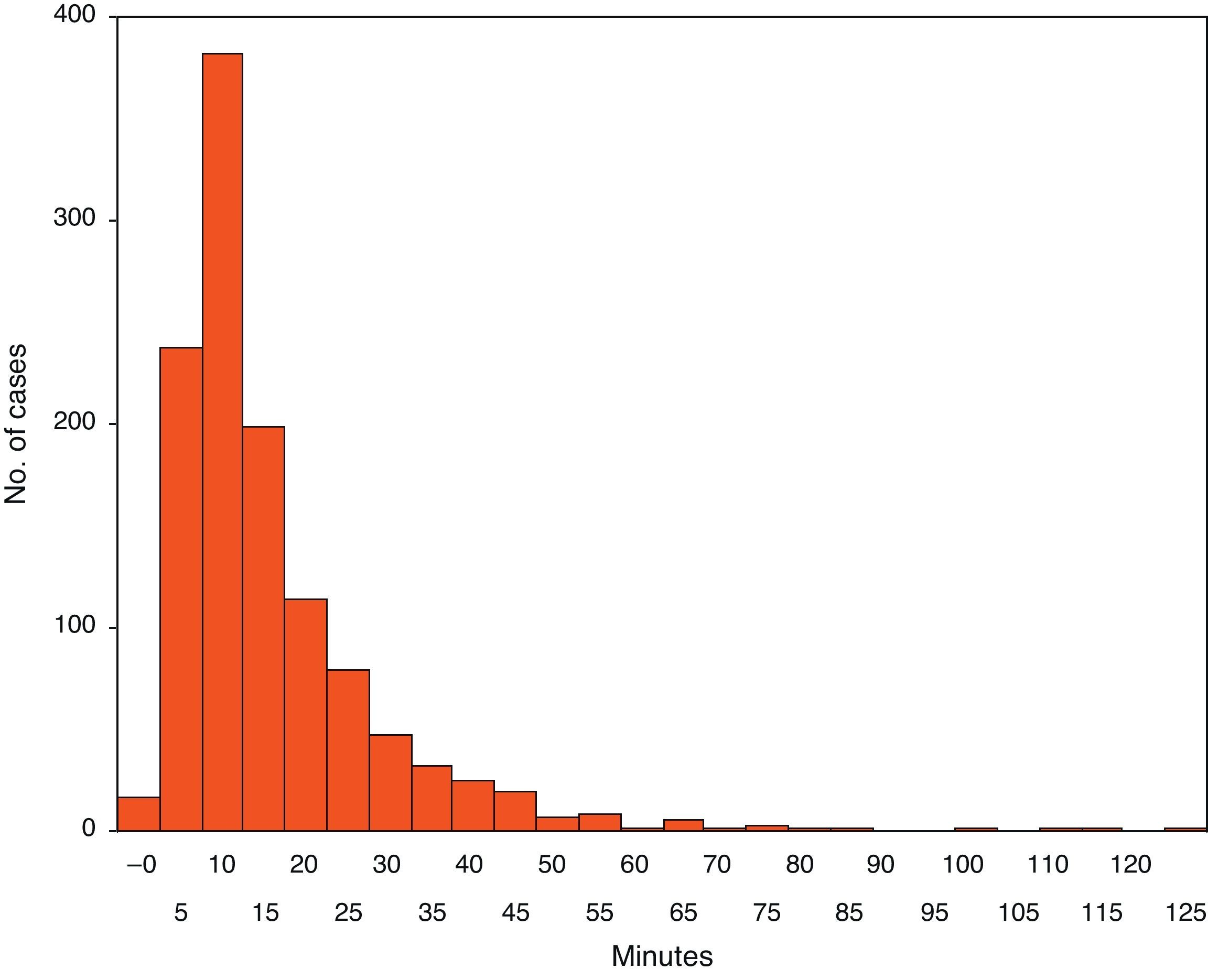
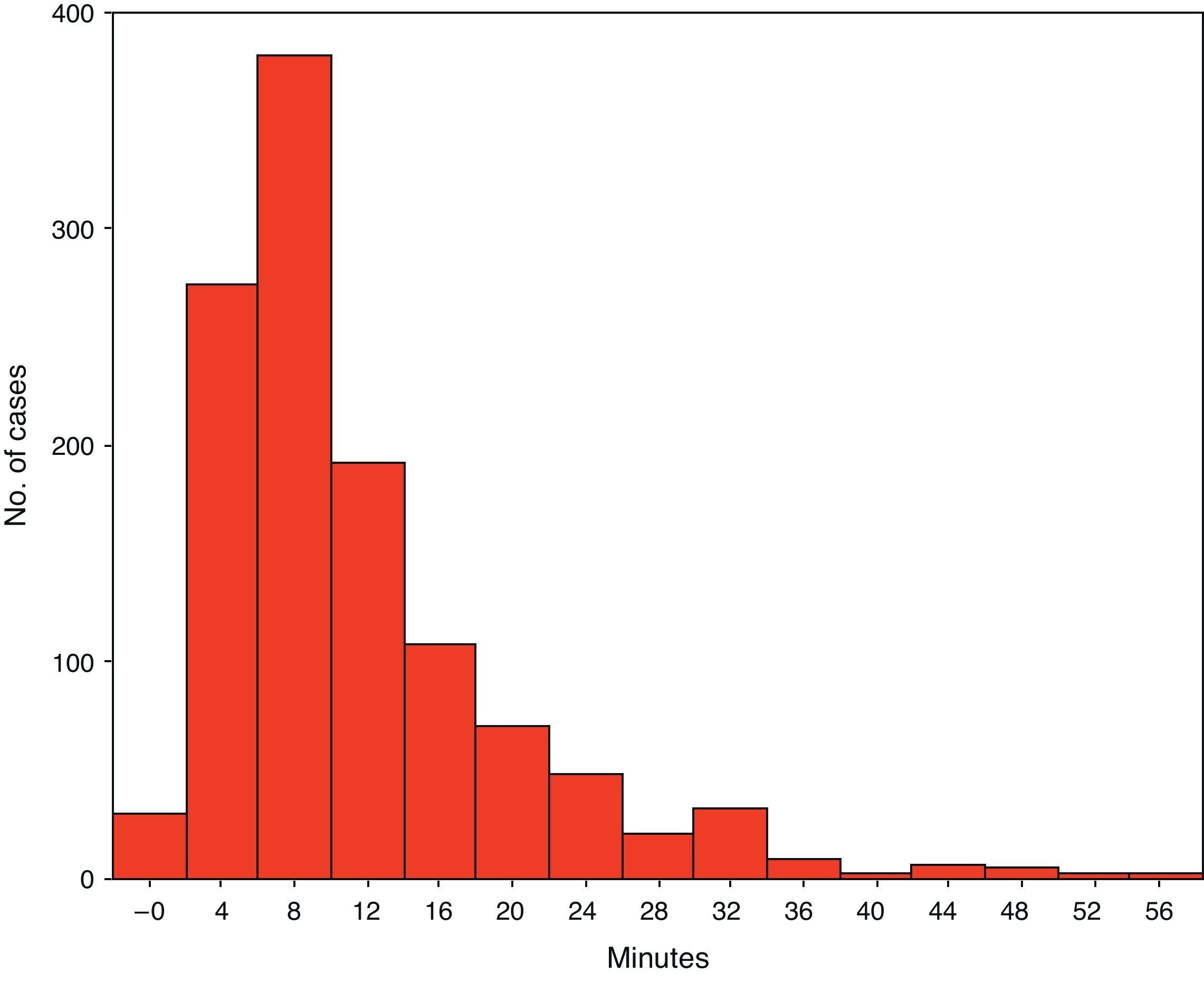
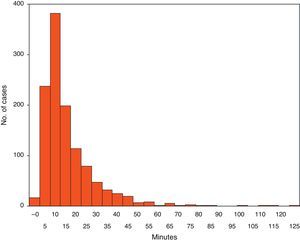
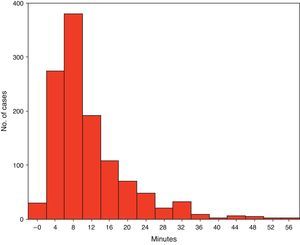
The distribution of the median time intervals between the alert call (dial 112) and EMS care, and between emergency team activation and care at the alert site is shown in Figs. 1 and 2.
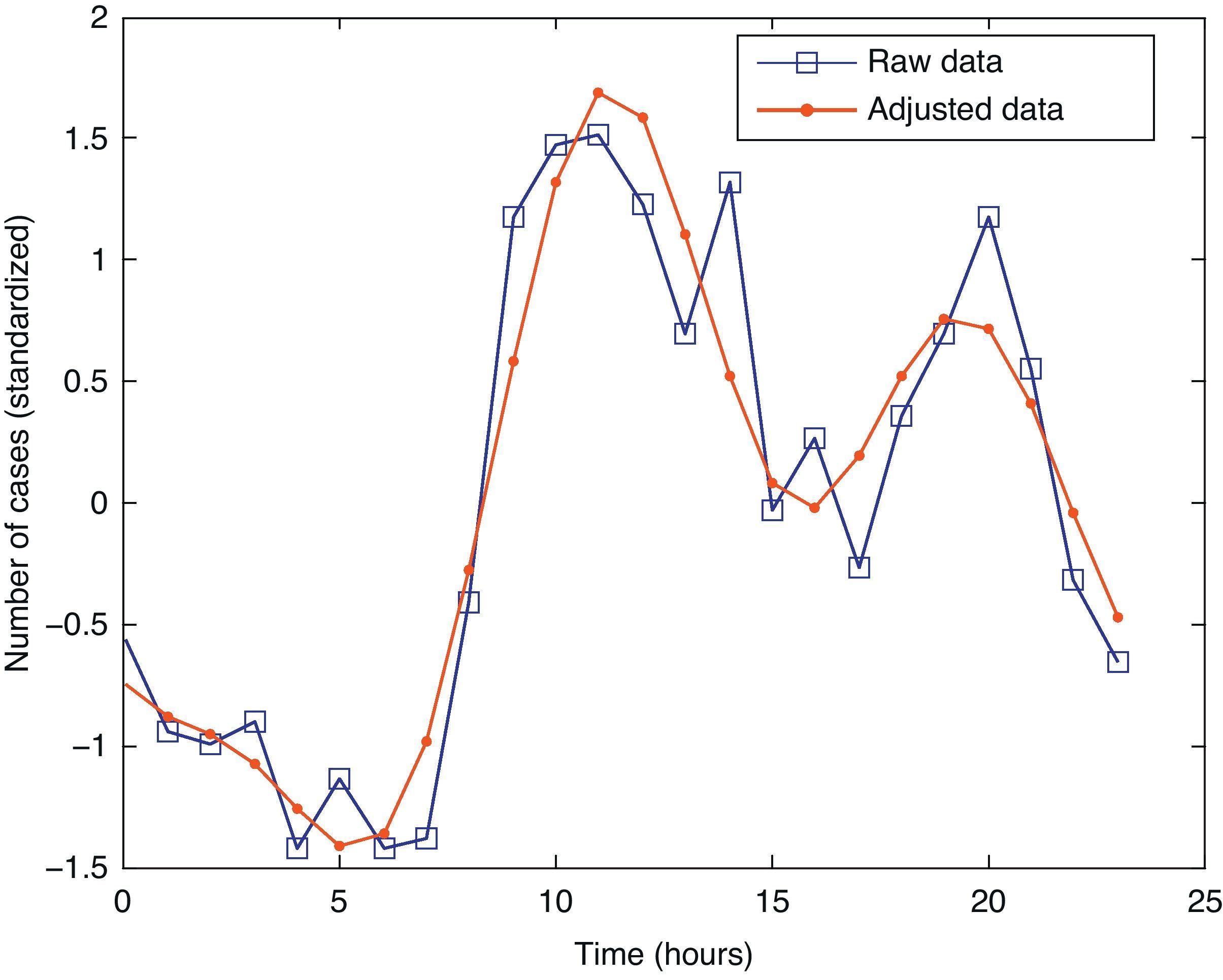
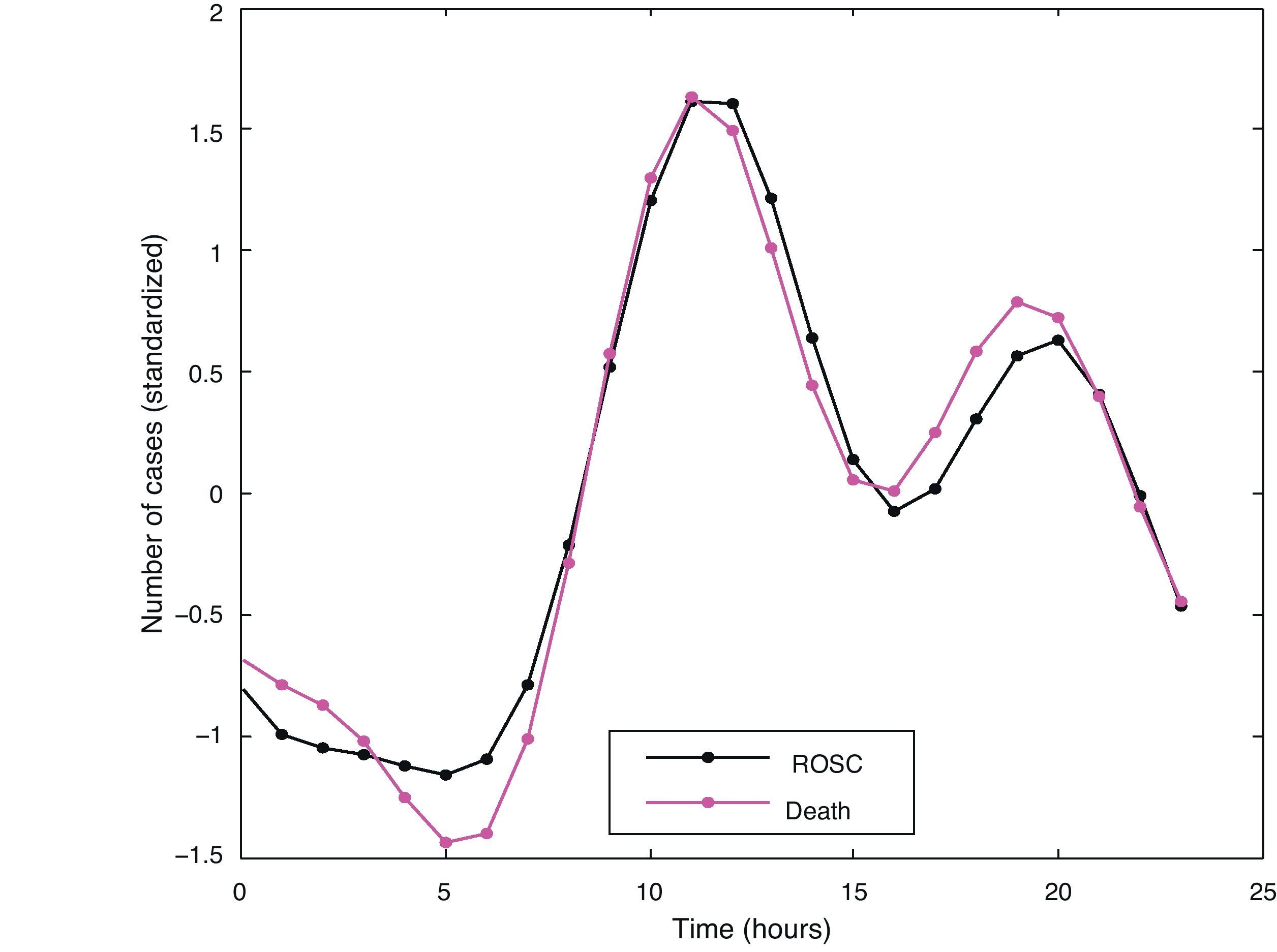
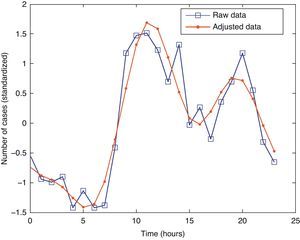
The chronobiological analysis based on the simple cosine test in seek of 24-h rhythms revealed a global acrophase at 11:16h, and a global batyphase at 5:20h (Fig. 3). This was concurrent to the demonstration of a statistically significant 24-h or circadian harmonic rhythm (p=0.000). The grouping of cases over the hours of the day showed clear peaks, with a greater number of events at 10, 14 and 20h.
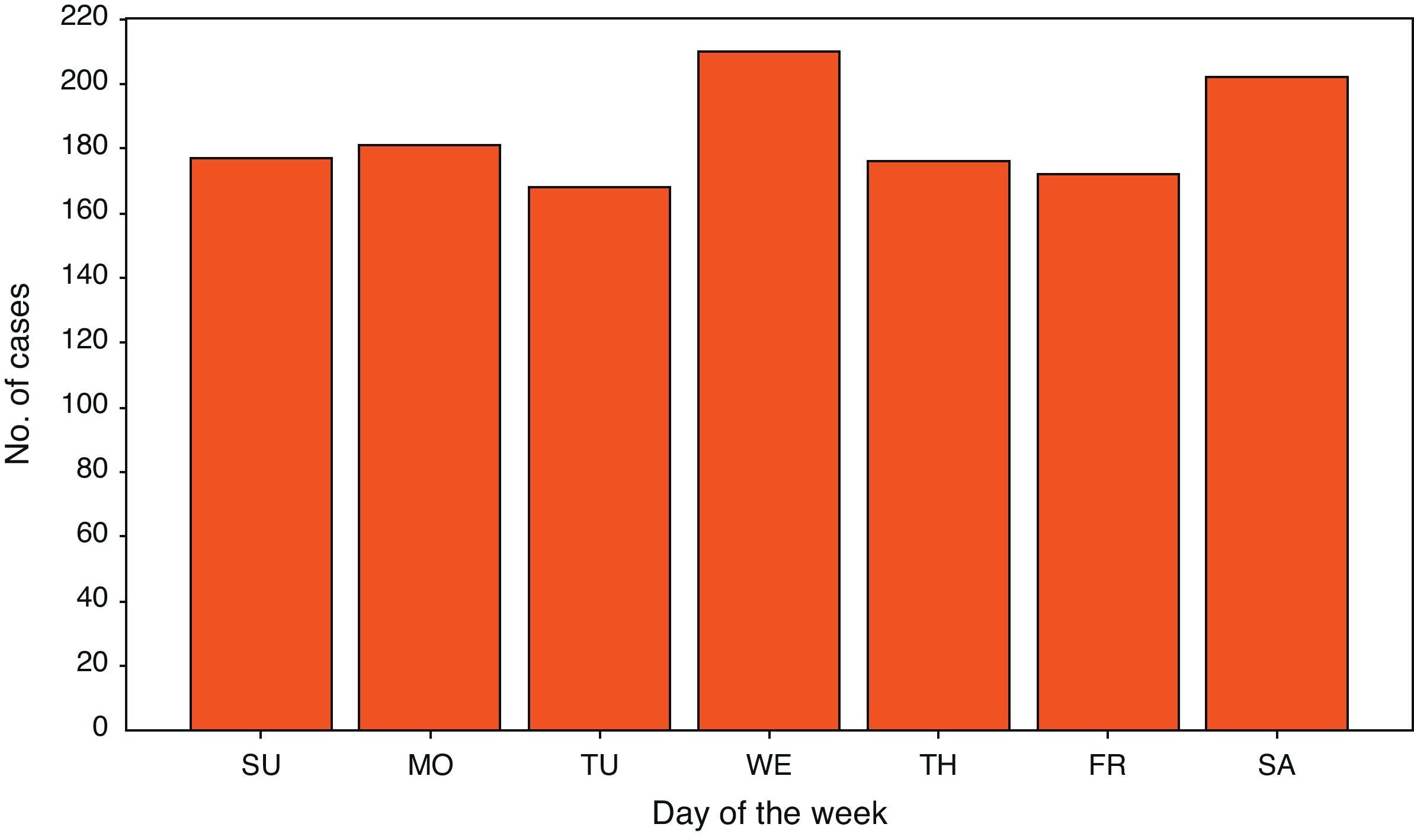
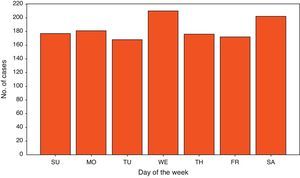
The chronobiological analysis based on the simple cosine test in seek of 7-day rhythms revealed a global acrophase on the third day of the week (Wednesday), and a batyphase on day 7 (Sunday). This was concurrent to the demonstration of a statistically significant 7-day or circaseptan rhythm (p=0.019). The grouping of cases over the days of the week showed two peaks with a greater number of events, corresponding to Wednesday and Saturday (Fig. 4).
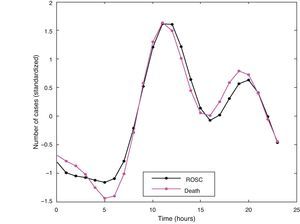
There were no statistically significant differences in the chronobiological analysis of daily rhythm, distinguishing between the cases of ROSC and death (Fig. 5): ROSC, acrophase 11:28h, batyphase 5:03h; death, acrophase 11:12h, batyphase 5:24h (p=0.963). The chronobiological analysis of weekly rhythm likewise revealed no significant differences (p=0.879).
DiscussionIn the present study, based on a large population database, circadian variation was observed in the occurrence of OHCA, with no differences in relation to the initial outcome of the cases. A prevalent peak was recorded in the first hours of the morning, with another peak in the afternoon, as well as a clear decrease in the nighttime hours–in coincidence with the observations of other authors.
Regarding the analysis of the time variations in the presentation of OHCA, it should be noted that although a circadian rhythm had been described in 1987,6 very few further studies have been published,7,8,11–14 and none have been conducted in our particular setting to date. In a recently published study in Asia,18 a daily rhythm in appearance of the disorder has been reported–with two peak incidences (at 8:00h and at 19:00h).
Other publications on time variations in cardiovascular events have examined the hypotheses proposed to explain such variations. In this context, certain triggering physiopathological factors have been suggested to intervene at certain times of the day, including sympathetic tone or platelet activity.19,20 Other purported triggering factors comprise different types of physical activity, and changes in environmental temperature.9,10
On the other hand, a recent study21 whose results have not been confirmed in our work reports that OHCA survivors–in contrast to non-survivors–present a circadian rhythm in the appearance of the disorder, with an increased frequency between 18 and the 22h.
Thus, a large morning peak is noted, with a less marked afternoon peak, confirming the need to adopt preventive and therapeutic measures (“chronotherapy”) fundamentally in patients at risk, and suited for adjustment in time to attenuations in the triggering phenomena.
Regarding the time analysis of the differences observed in the course of the days of the week, our data do not coincide with the results of Brooks et al.22 and Gruska et al.23, who reported an increased incidence on Mondays and Saturdays, respectively, while in our series the peak incidence corresponded to Wednesdays. On the other hand, there were no differences in relation to outcome according to the day of the week on which OHCA occurred. This lack of agreement among the different studies referred to the weekly variations of OHCA points to the need for larger and more specific studies capable of clarifying this issue.
The more frequent presentation of OHCA in the home of the victims, witnessed by relatives or cohabitants during the nighttime period (between 0h and 8h), would justify the lesser tendency towards ROSC, probably due to a lesser availability of people trained in life support or of medical resuscitation teams in this particular scenario.
The data referred to the time intervals between the alerting call, activation of the EMS team, and the time of care at the alert site coincide with those published elsewhere.16 Although there were no significant differences among the three time periods analyzed, the intervals were longer in the period between 0h and 8h. This fact, and the observation of a lesser ROSC rate in that same period, suggest that delays in processing the alert call, in activating the EMS team, and in providing care at the alert site could have an influencing effect, along with other factors such as the known lesser incidence of rhythms amenable to defibrillation in OHCA occurring in the home.24 In this context, studies comparing the intervals of different EMS involving similar settings and characteristics would be needed to establish guiding references.
Our study offers information on the EMS activation circuits in cases of OHCA and on the time variations in the appearance of the disorder and in the times to intervention. Such data can be used to analyze and project new strategies for dealing with OHCA; in this context, specific registries are absolutely necessary in our setting,25 in order to confirm the results obtained. Emphasis also should be placed on the need to implement the first two links in the survival chain. In Spain, the response system has been developed in a generalized manner through the EMS, offering demonstrated quality and competence.26 However, much work remains to be done in reference to early activation of the EMS and to the provision of basic life support on the part of witnesses of the event.27 In this context, increased social awareness is needed, with the development of comprehensive training programs targeted to the general population.28
Lastly, regarding the limitations of the study, mention must be made of the lack of information on the previous health condition of the patients, the time interval between the event and the alert call (dial 112), the performance or not of resuscitation maneuvers by the witnesses, patient survival and neurological condition at hospital discharge, and possible data introduction errors, and the observational and retrospective nature of the study.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: López-Messa JB, et al. Ritmo circadiano y variaciones temporales en el paro cardiaco súbito extrahospitalario. Med Intensiva. 2012;36:402–9.