To determine the diagnostic performance of the clinical evaluation of peripheral tissue perfusion in the prediction of mortality.
DesignSystematic review and meta-analysis.
SettingIntensive care unit.
Patients and participantsPatients with sepsis and septic shock.
InterventionsStudies of patients with sepsis and/or septic shock that associated clinical monitoring of tissue perfusion with mortality were included. A systematic review was performed by searching the PubMed/MEDLINE, Cochrane Library, SCOPUS, and OVID databases.
Main variables of interestThe risk of bias was assessed with the QUADAS-2 tool. Sensitivity and specificity were calculated to evaluate the predictive accuracy for mortality. Review Manager software version 5.4 was used to draw the forest plot graphs, and Stata version 15.1 was used to build the hierarchical summary receiver operating characteristic model.
ResultsThirteen studies were included, with a total of 1667 patients and 17 analyses. Two articles evaluated the temperature gradient, four evaluated the capillary refill time, and seven evaluated the mottling in the skin. In most studies, the outcome was mortality at 14 or 28 days. The pooled sensitivity of the included studies was 70%, specificity 75.9% (95% CI, 61.6%–86.2%), diagnostic odds ratio 7.41 (95% CI, 3.91–14.04), and positive and negative likelihood ratios 2.91 (95% CI, 1.80–4.72) and 0.39 (95% CI, 0.30–0.51), respectively.
ConclusionsClinical evaluation of tissue perfusion at the bedside is a useful tool, with moderate sensitivity and specificity, to identify patients with a higher risk of death among those with sepsis and septic shock.
RegistrationPROSPERO CRD42019134351.
Determinar el rendimiento diagnóstico de la evaluación clínica de la perfusión tisular periférica en la predicción de mortalidad.
DiseñoRevisión sistemática y metaanálisis.
ÁmbitoUnidad de cuidados intensivos.
Pacientes y participantesPacientes con sepsis y shock séptico.
IntervencionesSe incluyeron estudios de pacientes con sepsis y/o shock séptico que asociaron la monitorización clínica de la perfusión tisular con la mortalidad. Se realizó una revisión sistemática buscando en las bases de datos PubMed/MEDLINE, Cochrane Library, SCOPUS y OVID.
Variables de interés principalesEl riesgo de sesgo se evaluó con la herramienta QUADAS-2. Se calcularon la sensibilidad y la especificidad para evaluar la precisión predictiva de la mortalidad.
ResultadosSe incluyeron trece estudios, con un total de 1667 pacientes y 17 análisis. Dos artículos evaluaron gradiente de temperatura, cuatro evaluaron tiempo de llenado capilar y siete evaluaron moteado en la piel. La mayoría de los estudios midieron mortalidad a 14 o 28 días. La sensibilidad agrupada de los estudios incluidos fue 70% y especificidad 75,9% (IC del 95%, 61,6%–86,2%), la razón de probabilidad diagnóstica 7,41 (IC del 95%, 3,91–14,04) y la razón de probabilidad positiva y negativa 2,91 (IC del 95%, IC, 1,80–4,72) y 0,39 (IC 95%, 0,30–0,51), respectivamente.
ConclusionesLa evaluación clínica de la perfusión tisular es una herramienta útil, con sensibilidad y especificidad moderadas, para identificar pacientes con sepsis y shock séptico con mayor riesgo de muerte.
RegistroPROSPERO CRD42019134351.
The alteration of microcirculation in sepsis is one of the main triggers of multiple-organ failure and death.1 Traditionally, monitoring and treatment goals in sepsis and septic shock are based on macrohemodynamic and biochemical variables such as lactate.2 The macrohemodynamic variables have not shown a relationship with mortality and are not always related to changes in microcirculation during treatment.3–5 This dissociation between the macrocirculatory and microcirculatory compartments is known as “loss of hemodynamic coherence”.6 For this reason, it is important to have tools to routinely monitor microcirculation. It is difficult to identify and evaluate microcirculatory alterations at the bedside since the necessary technology is not always available or the output may take time to evaluate.7 However, an organ that is easy to evaluate and quickly accessible, such as the skin, allows noninvasive monitoring of peripheral tissue perfusion and a possible window into microcirculation.
Parameters such as the temperature gradient of the skin (the surface temperature compared with the core temperature or the ambient temperature), the time of capillary refill, and the extent of skin mottling at the level of the knees have been studied.8 Observational studies have evaluated these clinical parameters of peripheral tissue perfusion in septic patients, suggesting a relationship with organ failure and a constant association with the risk of death.9–11 The ANDROMEDA-SHOCK study, a recent multicenter randomized clinical trial, evaluated whether a resuscitation strategy guided by capillary refill time was superior to a strategy guided by lactate clearance, finding significantly fewer organ failures in the capillary refill time-guided group, with no significant differences in mortality at 28 days between the two groups.12 Later, in a Bayesian analysis, it was found a posterior probability of benefit in mortality using guided resuscitation with capillary refill time.13 Despite the growing evidence of the usefulness of the clinical parameters of tissue perfusion, their role in the monitoring of critical patients is not yet well established in clinical practice guidelines.
The objective of the present study is to determine the diagnostic performance of the clinical evaluation of peripheral tissue perfusion in the prediction of mortality in patients with sepsis and septic shock in the intensive care unit (ICU).
MethodsWe conducted a systematic review and meta-analysis to determine the diagnostic performance of the clinical evaluation of peripheral tissue perfusion, whether measured by skin temperature gradient, capillary refill time, or skin mottling, for the prediction of mortality (independent of time) in adult patients with sepsis or septic shock within the ICU.
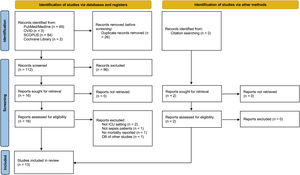
A systematic review was conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement14 and the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy15 and supplemented with the PRISMA statement specifically for study reviews of diagnostic accuracy.16 The protocol was preregistered in the PROSPERO platform (CRD42019134351).
Selection criteriaWe included prospective observational studies, written in English, of adult patients (age ≥18 years) with a diagnosis of sepsis and/or septic shock in the ICU. Those studies combined clinical monitoring of tissue perfusion by skin temperature gradient, capillary refill time, and/or mottling in the knees with mortality independent of follow-up time (mortality in ICU, at 8 days, 14 days, or 28 days). Case series, studies conducted outside the ICU, and those that did not evaluate mortality were excluded. For the meta-analysis, the selected studies had to have the necessary information to construct a 2×2 table.
Search strategyA systematic review of studies published up to December 31, 2022, was performed using the PubMed/MEDLINE, Cochrane Library, SCOPUS, and OVID databases. The search terms were shock, sepsis, septic shock, peripheral perfusion, skin perfusion, microcirculation, capillary time refill, mottling, temperature gradient, and mortality.
Selection processAfter duplicate studies were eliminated, two authors (DGZ and KRS) independently reviewed the title and abstract of every search result. In case of discrepancies over a study, a third author made the inclusion decision.
In a data extraction sheet, two authors (DGZ and KRS) independently extracted the data from the included studies for the analysis. The information extracted was compared, and any discrepancies were resolved by consensus.
Assessment of risk of biasTwo researchers (DGZ and KRS) independently assessed the risk of bias of the included studies using the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool.17 Differences were resolved by consensus. The QUADAS-2 tool is recommended for the evaluation of the quality of studies related to the performance of diagnostic tests. The tool evaluates four areas of potential risk: 1) patient selection, 2) index study, 3) reference standard, and 4) study flow and time.
Diagnostic accuracy measuresSensitivity and specificity were used to evaluate the diagnostic accuracy of mortality for each parameter.
Summary of the resultsThe clinical evaluation parameters of peripheral perfusion were categorized into skin temperature gradient, capillary refill time, and mottling in the skin at the level of the knees. The positivity threshold for each parameter was established by the author of each study. When more than one measurement was performed over time, the data obtained were analyzed independently. For the purposes of the analysis, when a cutoff point was not defined by the authors in the case of the mottling score, the variable was dichotomized as a score ≥2 or <2 according to the mottling score at the knee level described by Ait-Oufella et al.9
The results of the individual studies’ sensitivity and specificity are presented graphically in a 1-dimensional forest plot ordered by sensitivity. To group the results, a hierarchical summary model receiver operating characteristic (ROC) (HSROC) was applied, and the summary of points was obtained by estimating the sensitivity and specificity and their associated confidence range, as well as the diagnostic odds ratio (DOR) and diagnostic likelihood ratio (LR).
An analysis by subgroups was planned to look for heterogeneity between the studies, according to the type of tissue perfusion parameter, mortality at 14 and 28 days, the inclusion of only patients with a diagnosis of septic shock, and the use of the definition of Sepsis-3 or the International Sepsis Definition Conference (ISDC) criteria.
Review Manager software version 5.4 was used for the meta-analysis, and Stata version 15.1 (StataCorp LLC) was used to build the HSROC model.
ResultsSearch resultsA total of 138 papers were yielded by the systematic search. After eliminating duplicates, 112 titles and abstracts were reviewed. Of these, 16 articles were selected for full-text review, of which five were excluded because they did not meet the selection criteria. Two articles were added later from the references of the selected articles, for a total of 13 articles (1667 patients) included in the final analysis (Fig. 1).
Characteristics of the studiesTable 1 describes the characteristics of the included studies. Nine of the studies were conducted in France9,10,18,19,21,23,25,26 and four in Latin America, including the multicenter cohort of the ANDROMEDA-SHOCK clinical trial.20,22,24,27 The majority of the population had septic shock; two patients with sepsis and severe sepsis were also included.11,25 One study included only patients with sepsis,26 and another included only patients with liver cirrhosis plus septic shock.23 The definition of sepsis used in six studies9–11,19,23,27 was from the ISDC,28 and in five studies 18,20,22,24,25 the definition was Sepsis-3.29 In two studies, the definition used was not specified. Two articles evaluated the temperature gradient,11,18 four the capillary refill time,10,20,22,24 and seven the mottling in the skin.9,19,21,23,25–27 In most studies, the outcome was mortality at 14 or 28 days9,10,19,26,27; one study evaluated mortality at 8 days,18 and one evaluated mortality in the ICU.11 The reference standard varied between studies, but in 62% of the studies they used serum lactate.9–11,19,20,22,24,27 The most common site of infection reported was pulmonary, in 62% of studies,9–11,19,23,25–27 followed by abdominal in 23%,18,20,24 while in 15% it was not reported.21,22 The mean mortality of all patients was 36%.
Characteristics of all the studies included for the final analysis.
| Author | n | Characteristics of the study | Country | Type of patients | Sepsis definition | Most common site of infection | Peripheral perfusion method | Anatomic site | Cutoff | Standard reference | Time at measurement | Outcome | Overall mortality, % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bourcier et al.25 | 37 | Prospective observational study | France | Sepsis and septic shock | Sepsis-3 | Lung | Skin mottling | Knee and/or forearm | Presence | Transdermal iontophoresis of Ach | At 6h of resuscitation | 14-day mortality | 22 |
| Ait-Oufella et al.9 | 38 | Prospective observational study | France | Septic shock | ISDC | Lung | Skin mottling | Knee | Not decrease | Arterial lactate and urinary output | Mottling score changes during resuscitation between baseline and at 6h in patients with a score ≥2 | 14-day mortality | 45 |
| Galbois et al.23 | 42 | Prospective observational study | France | Liver cirrhosis and septic shock | ISDC | Lung | Skin mottling | Knee | Mottling score >1 | Laser Doppler | Mottling score at 6h of resuscitation | 14-day mortality | 71 |
| Ferraris et al.21 | 46 | Prospective observational study | France | Septic shock | NR | NR | Skin mottling | Knee | Mottling score ≥1 | Infrared thermography | At the time of inclusion and 6h after resuscitation | 28-day mortality | 30 |
| Ait-Oufella et al.19 | 52 | Prospective observational study | France | Septic shock | ISDC | Lung | Skin mottling | Knee | Mottling score ≥2 | Arterial lactate, urinary output and central venous saturation | At 6h of resuscitation | 14-day mortality | 48 |
| Ait-Oufella et al.10 | 59 | Prospective observational study | France | Septic shock | ISDC | Lung | Capillary refill time | Index finger | (IF) 2.4 seg (K) 4.9 seg | Arterial lactate and urinary output | At 6h of resuscitation | 14-day mortality | 37 |
| Knee | |||||||||||||
| Amson et al.18 | 61 | Prospective observational study | France | Septic shock | Sepsis-3 | Abdomen | Temperature gradient | Core-to-index finger | >7°C | Infrared thermography | At the time of inclusion | 8-day mortality | 16 |
| de Moura et al.27 | 97 | Retrospective analysis of observational data prospective collected | Brazil | Septic shock | ISDC | Lung | Skin mottling | Knee | Mottling score ≥2 | Arterial lactate and urinary output | On the day of septic shock onset | 28-day mortality | 52.6 |
| Bourcier et al.11 | 103 | Prospective observational study | France | Severe sepsis and septic shock | ISDC | Lung | Temperature gradient | Toe-to-room | <1.75°C | Arterial lactate and urinary output | At 24h | ICU mortality due to multiple-organ failure | 19 |
| Preda et al.26 | 109 | Prospective observational study | France | Sepsis | NR | Lung | Skin mottling | Knee | Mottling score ≥2 | NR | At 6h of resuscitation | 28-day mortality | 11 |
| Morocho et al.22 | 175 | Prospective observational study | Ecuador | Septic shock | Sepsis-3 | NR | Capillary refill time | Index finger | (H0) 4.5 seg (H6) 3.5 seg | Lactate, delta CO2 and central venous saturation | At admission at 6h | 28-day mortality | 40 |
| Hernández et al.20 | 424 | Post hoc analysis of the ANDROMEDA-SHOCK study | Multicentric in Latin America | Septic shock | Sepsis-3 | Abdomen | Capillary refill time | Index finger | >3 seg | Arterial lactate | At the time of inclusion | 28-day mortality | 39 |
| Kattan et al. 24 | 424 | Post hoc analysis of the ANDROMEDA-SHOCK study | Multicentric in Latin America | Septic shock | Sepsis-3 | Abdomen | Capillary refill time | Index finger | >3 seg | Arterial lactate | At 2h of resuscitation | 28-day mortality | 39 |
IF=index finger, ISDC=International Sepsis Definition Conference, K=knee, NR=not reported.
The evaluation of quality using the QUADAS-2 criterion is summarized in Fig. 1 of the supplement. The index test had an unclear risk of bias in 20% of the studies because they did not have a preestablished cutoff point. For the reference standard, four studies had an unclear risk of bias because the reference standard may identify alterations in skin perfusion but does not identify patients as alive or dead, and one study had a high risk of bias by not specifying a reference standard.
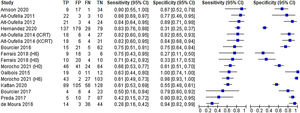
Summary of the resultsTwo studies took measurements at two different times: the time of inclusion of the patient in the study (H0) and at 6h (H6).21,22 In one study, two measurements of capillary refill time were performed: at the level of the knee and in the index finger.10 This is how the parameters to be analyzed came to 16. Fig. 2 shows the forest plot of sensitivity and specificity for the clinical evaluation of tissue perfusion reported in the 15 studies included. Table 2 describes the precision measures obtained from all the studies and the analyses by subgroups. The pooled sensitivity of the included studies was 70% (95% CI, 61%–77.7%), the specificity was 75.9% (95% CI, 61.6%–86.2%), the DOR was 7.41 (95% CI, 3.91–14.04), and the pooled positive and negative LRs were 2.91 (95% CI, 1.80–4.72) and 0.39 (95% CI, 0.30–0.51), respectively (Fig. 3).
Analysis of diagnostic accuracy grouped by the total and by subgroups.
| Analysis | Sensibility, % (95% CI) | Specificity, % (95% CI) | DOR (95% CI) | PLR (95% CI) | NLR (95% CI) |
|---|---|---|---|---|---|
| Overall | 70.0 (61.0–77.7) | 75.9 (61.6–86.2) | 7.41 (3.91–14.04) | 2.91 (1.80–4.72) | 0.39 (0.30–0.51) |
| Capillary refill time | 71.2 (62.2–78.8) | 73.1 (46.1–89.6) | 6.75 (2.31–19.74) | 2.65 (1.18–5.97) | 0.39 (0.28–0.54) |
| Skin mottling | 65.4 (48.0–79.5) | 79.5 (57.4–91.7) | 7.37 (2.68–20.29) | 3.20 (1.47–6.94) | 0.43 (0.28–0.66) |
| 14-day mortality | 77.8 (67.9–85.3) | 82.4 (74.3–88.3) | 16.5 (8.70–31.31) | 4.43 (2.98–6.57) | 0.26 (0.18–0.39) |
| 28-day mortality | 63.1 (49.6–74.8) | 69.8 (41.8–88.2) | 3.97 (1.64–9.60) | 2.09 (1.04–4.19) | 0.52 (0.40–0.69) |
| ISDC | 73.7 (56.7−85.7) | 83.2 (74.3−89.5) | 14.0 (7.66−25.54) | 4.41 (3.06−6.34) | 0.31 (0.18–0.52) |
| Sepsis-3 definition | 68.7 (58.2–76.9) | 71.0 (44.6−88.2) | 5.40 (2.02−14.44) | 2.37 (1.13−4.97) | 0.44 (0.32−0.60) |
| Septic shock | 73.0 (62.4–81.5) | 71.3 (52.6–84.8) | 6.75 (30.8–14.79) | 2.55 (1.47–4.40) | 0.37 (0.26–0.53) |
DOR=diagnostic odds ratio, ICSD=International Sepsis Definition Conference, NLR=negative likelihood ratio, PLR=positive likelihood ratio.
Hierarchical summary receiver-operating characteristic curve and bivariate summary points and their 95% confidence regions for all included analysis (Sensibility 70% [95% CI, 61%–77.7%] and specificity 75.9% [95% IC, 61.6%–86.2%]).
HSROC, Hierarchical summary receiver-operating characteristic.
The results of the subgroup analysis (divided by type of tissue perfusion parameter, reporting of mortality at 14 or 28 days, inclusion of only patients with septic shock, and the use of the Sepsis-3 definition or the ISDC) are presented in detail in the supplement. The HSROC model was not performed individually for the temperature gradient since only two studies with this form of evaluation were included. In the analysis of capillary refill time, the pooled sensitivity was 71.2% (95% CI, 62.2%–78.8%), and specificity 73.1% (95% CI 46.1%–89.6%). In the analysis of skin mottling, the pooled sensitivity was 65.4% (95% CI, 48%–79.5%), and specificity 79.5% (95% CI 57.4%–91.7%). For the analysis of mortality at 14 days, the number of interactions was only 30, with a pooled sensitivity of 77.8% (95% CI, 67.9%–85.3%), and specificity of 82.4% (95% CI 74.3%–88.3%). In the analysis of mortality at 28 days, the pooled sensitivity was 63.1% (95% CI, 49.6%–74.8%), and specificity 69.8% (95% CI, 41.8%–88.2%). In the analysis of studies that used the ISDC definition, the pooled sensitivity was 73.7% (95% CI, 56.7%–85.7%), and specificity 83.2% (95% CI, 74.3%–89.5%). In the analysis of studies that used the definition of Sepsis-3, the pooled sensitivity was 68.7% (95% CI, 59.2%–76.9%), and specificity 71% (95% CI, 44.5%–88.2%). For the analysis of studies that included only patients with a diagnosis of septic shock, the pooled sensitivity was 73% (95% CI, 62.4%–81.5%), and specificity of 71.3% (95% CI, 52.6%–84.8%).
DiscussionThis systematic review and meta-analysis evaluated the ability of the clinical methods of tissue perfusion evaluation described in the literature to predict mortality in adult patients with sepsis and septic shock. In summary, grouping the three methods evaluated, both the sensitivity (70%) and specificity (76%) were moderate for the prediction of death. For capillary refill time, the sensitivity (71.2%) and specificity (73.1%) were again moderate for the prediction of death. Skin mottling had the worst sensitivity (65.4%) but the highest specificity (79.5%).
In our extensive review of the literature, we did not find any systematic review or meta-analysis that evaluated the diagnostic accuracy of these clinical methods of tissue perfusion evaluation.
It is not new to try to objectify the clinical evaluation as a diagnostic tool and the evaluation of the state of shock. In 1969, doctors Joly and Weil demonstrated that the temperature gradient in patients with shock is correlated with cardiac output and discriminates patients with worse outcomes.30 Lima et al.31 demonstrated that the subjective evaluation of peripheral perfusion (touching the skin and measuring capillary refill time) can identify patients with greater organ dysfunction and higher levels of lactate. More recently, Hiemstra et al.32 found that the clinical data predicted death at 90 days about as well as other severity scores, such as Simplified Acute Physiology Score (SAPS) II and Acute Physiology and Chronic Health Evaluation (APACHE) IV, and bested the SOFA score in a prospective cohort of critically ill patients. In recent years, there has been particular interest in the clinical evaluation of tissue perfusion in sepsis and septic shock as a way to identify patients at risk of death and organ deterioration, with a performance comparable to traditional measures of tissue perfusion such as serum lactate. The serial measurement of lactate and its clearance has been associated with a reduction in the mortality rate and global resolution of associated tissue hypoxia in patients with septic shock, so it has been included within the definitions and guidelines of the resuscitation of patients with sepsis and septic shock.33 Ryoo et al. 34 compared the prognostic value for mortality at 28 days between lactate concentration and its clearance at 6h in septic shock patients, finding that lactate >2mmol/L at 6h had good sensitivity (85.3%) but poor specificity (35.1%). Lactate clearance greater than 10% had poor sensitivity (46.4%) but moderate specificity (74%), an inferior performance compared to the clinical evaluation done by the studies included in our meta-analysis.
Since the publication of the ANDROMEDA-SHOCK clinical trial, the current paradigm of lactate-guided resuscitation began to be questioned, highlighting clinical evaluation as a fundamental element in the management of patients with septic shock. The same capillary refill time has been studied in other settings outside the ICU. Lara et al.35 demonstrated its association with hospital mortality and adverse events in septic patients in the emergency room. On the other hand, Sebat et al.36 used capillary refill time as part of the early warning score, and they demonstrated its association with mortality independently only below hypoxemia.
Both the capillary refill time and skin mottling were the most frequently used methods in the included studies, and although it seems that the temperature gradient had a better diagnostic performance, since only two such studies included, we did not perform the HSROC model to compare it with the other methods. The temperature gradient has the advantages of being able to be used in patients with dark skin and providing quantitative information with good reproducibility, but its disadvantage is that it requires specialized equipment to measure skin temperature, which limits its availability.8
One strength of our study is that we conducted an extensive analysis of the literature of the main methods of clinical evaluation of tissue perfusion, resulting in the first systematic review and meta-analysis of this type. An important limitation is the quality of the included studies. First, in 40% of the studies, we identified a risk of bias for the reference standard because the reference standard was not identified or because it only evaluated the presence or absence of tissue hypoperfusion but lacked the ability to identify patients at risk of death. This is partly because there is no consensus reference standard for tissue hypoperfusion that also can identify patients at risk of death. The evaluation of microcirculation at the sublingual level may be ideal, but its applicability to the bedside is a limitation to consider.7 On the other hand, although lactate is more widely practicable than the evaluation of microcirculation at the sublingual level, it has numerous limitations for interpreting in sepsis.37 Second, the definition of sepsis has varied over time, which is why both the definition of the ISDC, and the definition of Sepsis-3 were used. In the analysis by subgroups, the diagnostic performance, separating the studies depending on the definition used yielded similar results. Third, the type of patients included was not homogeneous, although the majority were patients with septic shock. Three studies also included patients with sepsis or severe sepsis, and one study included a specific population of patients with liver cirrhosis, which we included in the subgroup analysis. The diagnostic performance of these was comparable to the pooled analysis of all studies. Finally, the follow-up time for mortality was different, with a better diagnostic performance when mortality was measured at 14 days than 28 days.
ConclusionsAccording to the results of this systematic review and meta-analysis, the clinical evaluation of tissue perfusion at the bedside is a useful tool, with moderate sensitivity and specificity, in patients with sepsis and septic shock to identify those with a higher risk of death. Studies with better methodological quality and with a clear reference standard that can determine the preponderant value of clinical parameters in the evaluation of tissue perfusion are needed.
Authors’ contributionDamián Gutiérrez-Zárate: Conceptualization, project administration, data curation, writing-original draft preparation.
Karina Rosas-Sánchez: Data curation, investigation, visualization, writing-review and editing.
José J Zaragoza: Formal analysis, software, validation and editing.
FundingNone.
Conflict of interestsThe authors declare that they have no competing interests.










![Hierarchical summary receiver-operating characteristic curve and bivariate summary points and their 95% confidence regions for all included analysis (Sensibility 70% [95% CI, 61%–77.7%] and specificity 75.9% [95% IC, 61.6%–86.2%]). HSROC, Hierarchical summary receiver-operating characteristic.](https://static.elsevier.es/multimedia/21735727/0000004700000012/v1_202312020012/S2173572723000693/v1_202312020012/en/main.assets/thumbnail/gr3.jpeg?xkr=1dZuESKpnCAWr3yCSGZ24A==)


