The information available on the processes of weaning from mechanical ventilation (MV) and extubation after severe neurological injury is scarce.1–4 The strategies used have been extrapolated from researches and protocols obtained from populations of patients without neurocritical conditions1,2 – situations that cannot be compared for several reasons. In the first place, most individuals with a brain injury are not ventilated because of a primary respiratory failure but because they show an altered state of consciousness due to their incapacity to keep their airways patent, meaning that the actual goal of artificial ventilation is to avoid fatal secondary damage factors such as hypoxemia, hypercapnia and hypocapnia.3,4 In the second place, neurocritical patients usually remain long periods of time with MV and artificial airways.2,4 Lastly, because it is not unusual to find, during ventilatory support and artificial airway withdrawal, several degrees of compromise of the state of consciousness followed by an inability to follow commands and move in order to obtain the classical parameters of MV and/or extubation withdrawal.5–8 So, because of all these controversial issues we will be trying to expose our point of view through the following questions.
Question#1. What is the clinical evidence on weaning from MV in the neurocritical patient?The data available today is scarce if we take into consideration the high susceptibility of this population when it comes to developing respiratory complications. Also, the neurocritical condition ranks second on the need for MV.1–3 On the other hand, one universally accepted criterion before initiating MV withdrawal is resolving the condition that triggered it – a situation that in neurocritical patients rarely happens.3,9 One multicenter prospective observational study revealed that neurocritical patients are ventilated for longer periods of time and have higher rates of ventilator-induced pneumonia and mortality compared to the general population.2 MV withdrawal was difficult in almost 50% of the cases, and prolonged in 10% of the cases. Both the methods and duration of withdrawal and the rates of reintubation were similar to those of populations without neurological conditions.2 In the prospective randomized controlled study conducted by Navalesi et al.10 it was determined that approaching the process of withdrawal and extubation from a protocolized, multidisciplinary and controlled fashion reduces the rate of failure.11
Question#2. Do conventional criteria apply when weaning from MV and extubation?There are different approaches here, since most criteria used cannot be obtained through the adequate technique or are impossible to implement because the state of consciousness has been compromised.3–9 Recent studies confirm the systemic failure of the usual criteria of withdrawal/extubation in neurocritical patients.5–7,9,12,13
When analyzing the predictors of failure in the process of withdrawal/extubation, we find that some of them are associated with characteristics of the critically ill patient per se such as age, heart failure, high levels of the b-type natriuretic peptide, or a positive hydric balance8; while others may be considered specific of neurocritical patients such as low scores on the Glasgow scale (GS), inadequate functioning of the cough reflex, weak cough and/or presence of abundant tracheal secretions.5–7,9,12,13 The evidence supporting these predictors is low.8 Recently, one prospective multicenter study determined, through multivariate analyses, the predictors of successful extubations in subjects with severe brain damage, from which they developed the VISAGE score including age (<40 years of age), capacity to swallow, trouble maintaining fixation with both eyes and GS>10. Each item was given one (1) point; 90% of the patients extubated successfully scored ≥3 in this scale.14
Question#3. Is the capacity to respond to simple orders and follow commands indispensable prior to the process of weaning from MV and extubation?Extubation is a controversial issue in individuals with mental disorders or who “do not follow commands”.15 The “incapacity to follow commands” has not been fully described and any assessments conducted among intubated patients using the GS are subject to error. Also, the cut-off point to establish the capacity to be extubated is controversial.5–9,15
Namen et al.12 confirmed that in a heterogeneous neurocritical population of patients who scored ≥8 on the GS, failed extubation happened 25% of the times, and it went up to 63% in those who scored <8. Scoring ≥10 on the GS was associated with successful extubation procedures in another study.14
The actual recommendations suggest that to initiate the withdrawal of MV, the patient should be awake and capable of following commands.8 However, in the case of brain injuries, this parameter is not strictly necessary.3–7,9 Coplin et al.13 reported successful extubation rates in 80% of the patients who scored ≤8 on the GS and in 91% of those who scored ≤4 on such scale. Ko et al.5 used the Four Score to assess the patients’ neurological state, but they did not find any significant differences in the average score between those whose extubation failed and those whose extubation was successful. Similar results were reported by Anderson et al.6 using the GS. McCredie et al.7 confirmed that the GS is not associated with successful extubations.
Question#4. What are factors associated with successful extubation processes?Both the control of the airway and post-extubation complications play a key role in the success or failure of the entire process.
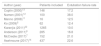
The airway care score (ACS) assesses the capacity to protect and maintain patent airways by checking on the vomiting reflex, the color and number of secretions, and the need for aspirations prior to the extubation procedure13 (Table 1). Scores ≤6 predicted successful extubations; but yet despite the fact that the ACS is very practical, neither the original ACS nor any of its modifications have been validated externally or through a large scale study.11,13 Anderson et al.6 reported that the capacity of coughing effectively and the presence of the vomiting reflex are associated with successful extubation procedures. Spontaneous or provoked cough is an independent predictor factor of successful extubation procedures.7
Airway care score (ACS).
| Grade | Cough during the aspiration maneuver | Number of secretions (need for passes) | Color of secretions | Viscosity of secretions | Interval of aspiration of secretions | Vomiting reflex |
|---|---|---|---|---|---|---|
| 0 | Vigorous | 0 | Clear | Aqueous | More than 3h | Vigorous |
| 1 | Moderate | 1 | Clear brown | Frothy | Every 2–3h | Moderate |
| 2 | Weak | 2 | Yellow | Dense | Every 1–2h | Weak |
| 3 | Absent | ≥3 | Green | Sticky | <1h | Absent |
Source: adapted from Coplin et al.13
When it comes to post-extubation complications, the incidence of stridor is between 1.5 and 26.3% while the rates of laryngeal swelling are somewhere between 5 and 54.4%, which can be explained by the lack of clear diagnostic criteria for this situation.16,17
In general, the rates of reintubation in critically ill patients are between 18 and 69% for stridor and 15% for laryngeal swelling.10 Such complications can be predicted very accurately using the Cuff Leak Test. Different systematic reviews and clinical guidelines confirm this.17–22 The actual recommendations suggest using steroids whenever the Cuff Leak Test is positive.21
Question#5. What is the extubation failure rate?In one (1) out of every five (5) patients the extubation procedure fails. Table 2 shows data from the extubation failure rates in neurocritical patients available today at the actual medical literature.
Question#6. Tracheostomy: is it necessary? If so, when and how?Controversial issue with uncertain benefits. Two retrospective database studies conducted on severe brain trauma, one of them with associated thoracic trauma recommend conducting early tracheostomy procedures based on fewer pneumonias, days on MV and stay at the intensive care unit (ICU). Nevertheless, the mortality rate was similar in the group that underwent late tracheostomy procedures.23,24 Other than the limitations of the methodological design of both studies per se, the reason why the tracheostomy was indicated was not specified.23,24 In another open randomized controlled study with a small sample of ischemic and hemorrhagic stroke victims, early tracheostomies did not reduce the stay at the ICU, but they did reduce the mortality rate, although this was a secondary outcome measure.25 One recent systematic review and one meta-analysis including 10 studies with 503 patients with acute brain injuries showed that early tracheostomies did reduce the long-term mortality rate, the duration of the MV, and the stay at the ICU; however, in the sensitivity analysis conducted, when excluding one biased study, statistical significance went down.26 Even though the Panamerican Iberian consensus does not deal with neurocritical patients, it does not recommend conducting early tracheostomies because, even though this shortens the duration of MV, it does not reduce the rates of pneumonia, days at the ICU, or long-term mortality.27 The percutaneous tracheostomy is preferred to the surgical one due to its lower rate of infections.27 Certain situations favor conducting early tracheostomies: (a) severe cervical spine injuries; (b) infratentorial severe injuries; (c) repeated failed extubations; (d) prolonged MV and (e) poor neurological state.3,27 The role played by primary tracheostomies is still controversial.23–28 In our own opinion, most individuals meet the necessary conditions to be extubated before attempting primary tracheostomies. This is why we firmly believe that conducting one tracheostomy procedure with an organized protocol and team work is a valid option.
Question#7. Early mobility: does it really help?Traditionally, neurocritical patients used to remain at rest during the acute phase of their disease. One binational multicenter study backs up this statement, since 84% of individuals could not move during such phase.29 We are standing at the doors of what will be a change of paradigm and cultural approach when it comes to the early mobility of critically ill patients.30–32 The available evidence today states that this new therapeutic approach is safe and feasible if conducted under controlled multidisciplinary programs.30–32 One recent meta-analysis conducted among individuals who required prolonged intensive care confirmed that implementing early mobility protocols reduced the duration of MV, the stay at the hospital and mortality rate, and improved the functional state.30 Specific programs implemented among patients who have not moved for long periods of time confirm their positive effect on the final outcomes.31 These results are encouraging and require large-scale validation among different populations of patients.
As far as we know no study today has been able to establish a correlation between early mobility and MV/extubation withdrawal, let alone among neurocritical patients. In patients with brain injuries, one prospective randomized observational uncontrolled Italian cohort reported better clinical and functional outcomes after implementing programs of early mobility, which opens promising approaches in the future.33
ConclusionWe need to conduct large scale studies that will allow us to make recommendations with a higher degree of certainty. In the meantime, we hereby present that:
- •
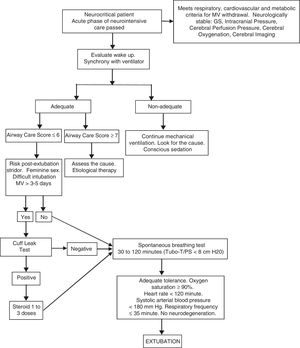
Since we need one protocolized organized multidisciplinary algorithm for every neurocritical patient based on their individual needs when it comes to MV and extubation withdrawals, we hereby propose an algorithm we can use when having to deal with all these issues (Fig. 1).
- •
The usual criteria to initiate the withdrawal of MV and extubation cannot be extrapolated to neurocritical patients.
- •
Not answering to verbal commands or low scores on the GS does not mean delaying or contraindicating MV and/or extubation withdrawal.
- •
The airway care score (ACS) is a useful tool to predict the capability of keeping an open airway safely.
- •
The Cuff Leak Test predicts the odds of postoperative swelling and stridor.
- •
Conducting one primary tracheostomy is advisable in groups at risk.
None declared.
Conflicts of interestThe authors declare no conflicts of interest associated with this article whatsoever.
Please cite this article as: Jibaja M, Sufan JL, Godoy DA. Controversias en la retirada de la ventilación mecánica y extubación en el paciente neurocrítico. Med Intensiva. 2018;42:551–555.