Ji and colleagues1 plotted COVID-19 mortality against incidence and demonstrated a statistically significant correlation, which highlighted a possible link between mortality and health-care burden; we recently found a similar association between case fatality rate (CFR) and intensive care unit to total inpatient admission rate (ICUAR).2
Extending our previous analysis over time on the cumulative data from February 21st to April 18th, and including COVID-19 incidence, we evaluated CFR and ICUAR on 175,925 cases, 27,740 inpatients, 2733 intensive care unit (ICU) inpatients, 23,227 deaths: the CFR was 13.2%, and the number of patients admitted in ICU varied along time, reaching a peak of 4068 on April 3rd and reducing to 2733 on April 18th (32.8% reduction in 2 weeks).3
The COVID-19 incidence and ICU capability varied widely amongst the Italian Regions: the average incidence was 28.6 per 10,000 people (range 5.2–85.6) and the average ICUAR was 11.8% (range 4.4–22.7).3
There are some particular issues involved in the estimation of CFR in Italy: the high average age of the Italian population, the definition of COVID-19-related deaths, the pharyngeal swab testing strategy employed and the CFR variation in different epidemic time-frame. It has been postulated that the confirmed diagnosis of milder cases could increase with the number of swabs taken.4
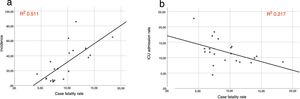
A univariate analysis of Italian regional data showed a strong correlation between CFR and COVID-19 incidence (R 0.715, R2 0.511, p-value 0.000), an inverse correlation between CFR and ICUAR (R −0.466, R2 0.217, p-value 0.033) (Fig. 1). The pharyngeal swab per 10,000 people did not correlate with the CFR (p-value 0.368).
The multivariate analysis showed that CFR was only associated with COVID-19 incidence (p-value 0.001), but neither with ICUAR (p-value 0.172), nor with pharyngeal swab per 10,000 people (p-value 0.221).
The different COVID-19 incidence and ICU capability in the Italian Regions showed that mortality was linked to high incidence and ICU capability.
Our previous analysis was done during the continuous everyday increasing of ICU patients, which peaked on April 3rd, whether now we included two weeks of decreasing pressure on ICU: the association between CFR and ICAR is still present, but in the multivariate regression model only the incidence had a significant effect. Lombardy was the epicenter of the out-break and the region with higher CFR: it was an outlier, probably contributing to reduce the coefficient of determination (R2) in the correlation between CFR and ICUAR.
During different time-frame of such a huge outbreak the key factors associated with CFR may play different roles: the incidence seems to be strongly associated with CFR, but the ICUAR could be associated especially during the increasing of out-break when the ICU capability could be overwhelmed. According to this hypothesis different health-care resources should be implemented in different out-break time-frame.
Conflict of interestOn behalf of all authors, the corresponding author states that there is no conflict of interest.
The author thanks The Italian Civil Protection Department for sharing the data on line and Mrs Barbara Ward for her linguistic advice.