Edited by: Alberto García-Salido - Pediatric Intensive Care Unit, Hospital Infantil Universitario Niño Jesús, Madrid, Spain
Last update: May 2024
More infoThe SARS-CoV-2 pandemic has required the adoption of public health measures aimed at reducing its expansion. These measures, including the mandatory use of facemasks, hand hygiene or social distancing, have also been extended to the pediatric population, and have conditioned the transmissibility not only of SARS-CoV-2 but also of other pathogens. This circumstance has led to fewer infections and hospital admissions.1,2 As described in different countries, in the case of seriously ill pediatric patients, the adoption of such measures appears to be associated with a decrease in infectious conditions of all kinds - with a particularly strong impact upon respiratory infections.3,4
The present study was carried out to quantify the impact of the pandemic, reviewing the admissions to the Pediatric Intensive Care Unit (PICU) of a tertiary hospital during the first year of the SARS-CoV-2 emergency situation. Comparison was made versus the three previous years in order to determine possible differences in the number and characteristics of the attended patients. This retrospective descriptive study was approved by the local Clinical Research Ethics Committee, and covered the period between January 2017 and December 2020. All patients admitted to the PICU were included, and 2020 was compared against the median admissions corresponding to the three previous years. The type of hospital admission, defined by the fundamental cause of admission, was documented, analyzing the main diagnosis of each patient and grouping the subjects according to that diagnosis.
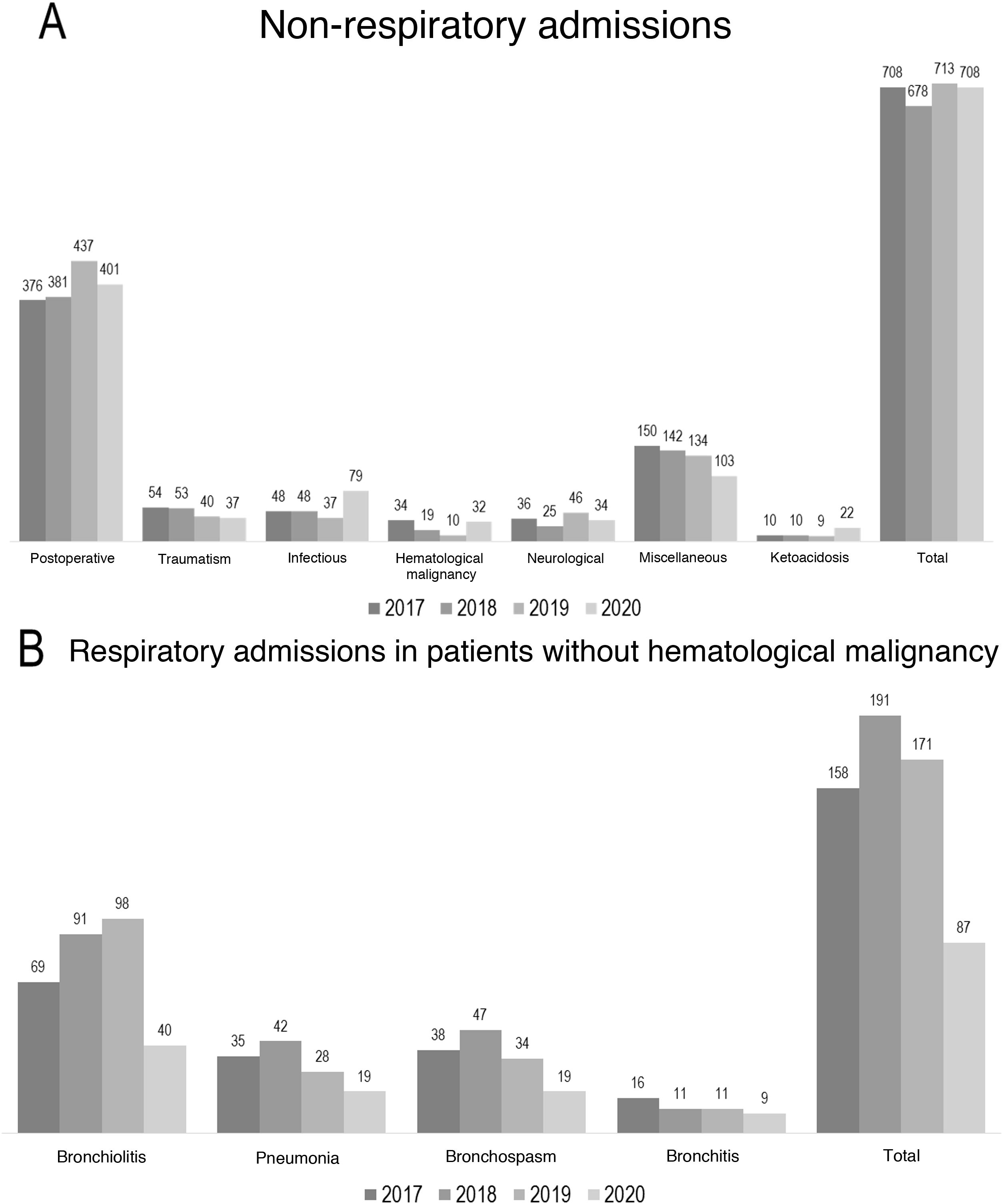
We analyzed a total of 3345 admissions in the four years of the study. The admissions by year were 790 in 2020, 894 in 2019, 874 in 2018 and 877 in 2017. The median number of admissions before 2020 was 877, and a 10% decrease with respect to this figure was recorded in 2020. Considering the number of respiratory admissions, and excluding patients with hematological malignancies, a total of 87 patients were admitted in 2020, 171 in 2019, 191 in 2018 and 158 in 2017 (Fig. 1). La median number of admissions before 2020 was 171, and a decrease of 49% was observed in 2020. The cases of bronchiolitis decreased 56% (40 in 2020, with a median of 91 in the period 2019−2017). In turn, the number of pneumonias decreased 46% (19 in 2020, with a median of 35 in the period 2019−2017). The cases of bronchospasm decreased 50% (19 in 2020, with a median of 38 in the period 2019−2017). We also compared the admissions due to non-respiratory causes (Fig. 1). The admissions by year were: 708 in 2020, 713 in 2019, 678 in 2018 and 708 in 2017. La median number of admissions was 708, and no decrease was observed in 2020. Of note is the increase in admissions due to infectious causes in 2020, excluding pneumonias (79 in 2020, with a median of 48 in the period 2019−2017). This was attributed to the cases of SARS-CoV-2 infection in 2020 (35 in total). We also recorded an increase in diabetic ketoacidosis (22 cases in 2020, with a median of 10 in the period 2019−2017).
(A) Bar chart showing the non-respiratory admissions, establishing comparisons by type of admission and total number. (B) Bar chart showing the respiratory admissions. Comparisons are made by fundamental cause and excluding patients with hematological malignancies. The “Miscellaneous” group comprises those patients in which no single fundamental cause of admission could be specified. Mention is made of the patients with diabetic ketoacidosis in view of the notorious increase in cases observed.
A slight decrease in the number of admissions was recorded in 2020 with respect to the previous years, fundamentally at the expense of respiratory disorders. In this regard, particular mention must be made of acute bronchiolitis, bronchospasm and pneumonias. No decrease in the rest of the admissions was observed, and an increase was noted in the number of admissions due to infectious diseases – this being related to SARS-CoV-2. Lastly, the number of cases of severe diabetic ketoacidosis was seen to increase.5
The PICU in which this study was carried out did not modify the type of care provided during the months of the first wave of the pandemic in the Community of Madrid (Spain). In turn, during the months of March to June 2020, it maintained pediatric care in that Community together with La Paz University Hospital. This circumstance led to a grouping of cases that undoubtedly resulted in a lesser impact upon the total number of admissions. It probably also influenced the greater number of cases of diabetic ketoacidosis treated during the first wave (March to June 2020) and the number of patients admitted in relation to SARS-CoV-2 infection.3,4
Considering the causes of admission, there was a clear decrease in the number of admissions related to respiratory infections. The associated microbiological agents share the same mechanisms and routes of contagion as SARS-CoV-2. The adopted public health measures probably contributed to reduce their community transmission. This was particularly notorious in the case of severe acute bronchiolitis. The decrease was evident and also underestimated. It must be taken into account that the series of 2020 included cases of severe acute bronchiolitis pertaining to the pandemic wave of 2019−2020. This difference probably would have been even greater had we analyzed the epidemic year instead of the natural or calendar year.6 In relation to the infectious causes, we excluded patients with hematological malignancies. This was done in an attempt to more reliably evidence the possible impact of the adopted measures upon the community transmission of pathogens in healthy children.2
The present study has limitations related to the way in which the data were collected or the absence of an etiological diagnosis in the case of the respiratory disorders. Classification according to the main cause of admission does not allow us to draw conclusions regarding the prevalence of the different pathogens. In turn, the pandemic itself introduces bias, since it influences and changes the reasons for admission and affects normal conduction of the different care activities of the hospital.
In conclusion, a modification of the profile of seriously ill pediatric patients was observed in our Unit, affecting respiratory disorders where the causal agents may share forms of contagion with SARS-CoV-2. The impact of the public health measures extended to other infectious agents thus evidences their usefulness in reducing frequent causes of serious illness in childhood.
Financial supportThe present study has received no financial support.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Salido A, Leoz-Gordillo I, García-Teresa MÁ, Iglesias-Bouzas MI, Martínez de Azagra-Garde A, Nieto-Moro M. Análisis descriptivo del impacto de la pandemia por SARS-CoV-2 en los ingresos de un servicio terciario de cuidados intensivos pediátricos. Med Intensiva. 2022;46:350–352.