To validate a safety tool used in high-risk sectors (safety briefing) in intensive care medicine.
DesignA prospective, observational and analytical study was carried out.
SettingTrauma and emergency intensive care unit in a tertiary hospital.
PatientsPatients with severe trauma (Injury Severity Score ISS≥16).
InterventionDocumentation of incidents related to patient safety (PS).
VariablesPatients characteristics, state of the Unit, patient safety incidents, aspects of the tool (SP) and safety culture impact.
ResultsWe included 441 patients (75.15% males, mean age 39.9±17.5 years), with blunt trauma in 89% and a 10.5% mortality rate. The tool was applied in 586 out of 798 possible shifts (73.4%), and documented 942 events (2.20 incidents per patient). The incidents were more frequently associated with medication (20.7%), devices (placement 4.03%, and maintenance 17.8%) and airway and mechanical ventilation (MV) (17.09%). A correlation was established between the occurrence of incidents and the characteristics of the patient (higher Injury Severity Score, presence of MV, and continuous renal replacement therapies) and the status of the Unit (more than 6 patients per shift out of 8 possible, and holiday period). The tool significantly influenced different aspects of the safety culture of the unit (communication frequency, number of events, punitive loss and active work in PS).
ConclusionsSafety briefing is a tool for the documentation of incidents that is simple and easy to use, and is useful for implementing improvements and in influencing safety culture.
Validar una herramienta de seguridad utilizada en sectores de alto riesgo (briefing de seguridad) en la medicina intensiva.
DiseñoEstudio prospectivo, observacional y analítico.
ÁmbitoUCI de Trauma y Emergencias de un hospital terciario.
PacientesPacientes con trauma grave (Injury Severity Score-ISS≥16).
IntervenciónRecogida de incidentes, relacionados con la seguridad del paciente (SP).
VariablesCaracterísticas de la población, estado de la unidad, incidentes de SP, aspectos de la herramienta e impacto sobre la cultura de seguridad.
ResultadosSe incluyeron 441 pacientes (edad media 39,9±17,5 años), 75,15% hombres, 89% con trauma cerrado y un 10,5% de mortalidad. La herramienta se aplicó en 586 turnos de 798 posibles (73,4%) y se recogieron 942 incidentes (2,20 incidentes por paciente). Los incidentes más frecuentes se relacionaron con la medicación (20,7%), los dispositivos (colocación 4,03% y mantenimiento 17,8%) y la vía aérea y la ventilación mecánica (VM) (17,09%). Se estableció una correlación entre la presencia de incidentes y las características del enfermo (mayor Injury Severity Score, presencia de VM y terapias de reemplazo renal continuo) y con el estado de la unidad (más de 6 pacientes por turno sobre 8 posibles y el periodo vacacional). La herramienta influyó en diferentes aspectos de la cultura de seguridad de la unidad de manera significativa (frecuencia de comunicación, número de eventos, pérdida de carácter punitivo y trabajo de manera activa en SP).
ConclusionesEl briefing es una herramienta para la recogida de los incidentes, simple, fácil de usar, útil para implantar mejoras e influir en la cultura de seguridad.
The complex combination of processes, technologies and human interactions conforming modern healthcare can result in important benefits, but also implies the risk of adverse events.1 For years the medical community has focused much attention on such events that are not directly related to the disease but result from interaction with the healthcare system, all within the concept of patient safety (PS).2,3 The concern about PS became a priority issue in other countries following the publication in 1999 of a classical report in the United States.4
In emergency care medicine and particularly in the intensive care unit (ICU) there are a series of circumstances that cause the system to be even more vulnerable to error (e.g., the complexity and time dependency of the disease processes dealt with in the ICU, prolonged work shifts, drug administration characteristics, and the presence of patients exposed to multiple interactions with both the health professionals and the system). However, the ICU also facilitates research in this field, since the Units are typically compact, accustomed to working as a team, and familiarized with patient severity scales–with expanding influence from the ICU to other hospital localizations and to the pre-hospital setting.5,6
Two key aspects of PS have often been cited in the literature: communication problems7,8 and PS culture.9 In this context, briefing consists of communication among the health professionals involved in a given task, adopting a previously designed protocol comprising both a methodology and a purpose or objective.10–14
The present study was designed to validate a PS instrument directly related to communication in complex systems and risk sectors–safety briefing10–14–and to assess its impact upon safety culture before and after its implementation in a setting characterized by scant experience with its use, namely the trauma and emergency ICU of a tertiary hospital.
Patients and methodsA prospective, observational and analytical study was made, comprising the registry of incidents related to PS, categorized according to types, severity and avoidability, and using a quality instrument (briefing) in the context of risk management in an ICU specialized in the care of serious traumatisms. A correlation was established with specific aspects referred to the activity of the Unit, the patient characteristics, and severity as defined by the Trauma and Injury Severity Score (TRISS) methodology, and impact in relation to safety culture. The instrument comprises a series of brief communication sessions or meetings among the global health personnel, based on a previously designed protocol related to PS (annex 1), in morning and afternoon shifts (Fig. 1). A PS-related incident was defined as any action or omission causing or potentially causing patient injury or damage, and more closely related to healthcare than to the complications of the background disease process of the patient. We excluded aspects related to nosocomial infection, in view of the characteristics of the instrument, which helps to detect incidents exhibiting a time relationship with the shift in which the meetings took place. The design was established taking into account other tools forming part of risk management in the Unit: the anonymous communication of incidents, analysis for identifying and preventing forms of failure, evaluating severity, frequency and detection through modal analysis of failures and effects (MAFE), the literature review on the subject, and the establishment of nominal groups as a strategy for obtaining information on the possible safety problems in a structured manner among the different professionals involved in applying the instrument (residents and staff physicians, nurses and nursing assistants), taking advantage of the training sessions held. Definitions were established for the study variables (annex 2), with instrument principles for controlling its quality (Table 1). Application of the tool was carried out at the end of the morning and afternoon shifts. As instrumentation for conducting the study, use was made of the following: TRISS methodology,15 the simplified severity classification, considering injury when ascribable to categories I–D or without injury when pertaining to categories A–C of the study «Incidents and Adverse Events in Critical Care Medicine. Safety and Risk in the Critical Patients (SYREC 2007)»,16 and the assessment of avoidability according to a questionnaire adapted to other experiences in similar settings.17,18 In both cases the decision referred to the two categories was made by consensus in the course of the meetings by the different participating professionals (residents, staff physicians and nursing personnel).
Principles of the briefing tool.
| 1. It is a working instrument, not an aim in itself.There must be an immediate objective, which is the introduction of improvements.2. The results should not be used to compare one Department with another.3. The instrument is to be incorporated to the working routine.4. It requires commitment on the part of the Unit supervisors.5. The instrument should be constructive and not of a punitive nature. A comfortable environment is recommendable.6. The findings should be presented openly to the implicated personnel.7. The duration is between 5 and 10min, in order to minimize time away from the patient bedside. The information generated during the sessions is confidential.8. A moderator or facilitator should be selected at the start.As the tool is put into practice, the number of facilitators should be varied.9. The language used should be objective and anonymous.10. The contents should vary according to the needs of the Unit. |
Evaluation of the impact of the tool upon patient safety culture was carried out by means of a safety culture questionnaire recommended by the quality unit of our hospital and validated for the emergency and intensive care setting, assessing different dimensions related to the safety of the patient (management promotional actions and expectations, safety training-continued improvement, teamwork, communication, feedback and communication of the error, non-punitive response to the error, personnel, management support, interdepartmental and interprofessional teamwork, transition between duties),19 according to the Rilke scale, based on the Safety Attitudes Questionnaire.20 We also documented details referred to the quality of the instrument (percentage completion, timing of completion, duration, personnel participating in the meetings out of the total persons present) and degree of activity of the Unit, with a view to evaluating possibilities for application and incorporation to routine clinical activity.
We included all the patients admitted during the 14-month study period. Certain types of patients admitted to the Unit were excluded, such as non-heart beating donors and clinical patients admitted to the ICU in which correlation to the TRISS methodology could not be established, or patients with trauma and a lack of data needed to the effects of calculation.
Nominal data collection was avoided, data presentation was carried out on an aggregated basis, and the study was approved by the Clinical Research Ethics Committee of the hospital.
The SPSS® version 15.0 statistical package was used to analyze the results obtained. We summarized the demographic data, briefing characteristics, condition of the Unit and the events recorded, based on descriptive statistics. Inferential statistical analysis was performed, with the comparison of means for independent samples using the Student t-test, while qualitative variables were contrasted with the chi-squared test, in accordance with previous studies.21 Logistic regression analysis was performed with the primary objective of modeling the influence of the presence or absence of factors related to the characteristics of the patients or Unit upon the probability of incidents. In all cases, statistical significance was considered for p<0.05.
ResultsThe study included 441 patients with a mean age of 39.9±17.5 years (75.1% males). The study population characteristics are reported in Table 2. The mortality rate in the series was 10.5%. Expected mortality according to the TRISS methodology was 16.9%, with an additive model of effect magnitude (W statistic) of 6.4 additional survivors per 100 patients treated (Z statistic, p<0.05). The theoretical total shifts that could be documented were 798 (two per day during 399 days of study). A total of 586 shifts were actually registered in the study (73.4%) with a similar distribution morning and afternoon (287 and 299 shifts, respectively). The presence of professionals during application of the instrument is shown in Table 3.
characteristics of the study population.
| Mean age | 39.9±17.5 years |
| Gender distribution | 75.1% males |
| Type of trauma | Closed 89% |
| Most frequent cause | Traffic accidents 20.3% |
| Hemodynamic instability upon admission | 34.2% |
| Mechanical ventilation | 48.6% |
| Duration of mechanical ventilation | 7.4±8.6 days |
| ICP monitorization | 12.7% |
| Duration of ICP monitorization | 7.2±5.7 days |
| Nosocomial infection | 16.5% |
| Coagulopathy upon admission | 32.9% |
ICP: intracranial pressure.
The activity of the Unit during the shifts was intense, with an average occupation of 5.6±1.7 patients per shift (ps) referred to a total of 8 beds, 4.2±1.7 patients subjected to mechanical ventilation (ps), 0.4±0.6 admissions (ps), 0.6±0.8 extra-ICU attendances (ps), 0.6±0.8 transfers to the Department of Radiology (ps), and 0.2±0.4 transfers to the operating room (ps). The mean briefing time was 6.1±3.3min (median 5min, interquartile range 4–6). There were statistically significant differences in duration between the meetings with and without the communication of incidents (549 shifts with information on the duration of the meetings), on comparing means with the Student t-test (shifts without incidents: 146; mean duration in these shifts: 4.1±2min; shifts with incidents: 403; duration: 6.5±3.1min; p<0.001), as represented in Fig. 2.
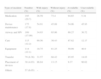
A total of 942 incidents were recorded with the instrument, with the detection of 2.20 incidents per admitted patient. Table 4 summarizes the number, type, severity and avoidability of the incidents detected with the tool.
Type, number, severity and avoidability of the incidents.
| Type of incident | Number (%) | With injury (%) | Without injury (%) | Avoidable (%) | Unavoidable (%) |
| Medication | 195 (20.7) | 26.59 | 73.4 | 94.65 | 5.34 |
| Device maintenance | 175 (17.8) | 54.91 | 45.08 | 54.06 | 45.93 |
| Airway and MV | 169 (17.09) | 34.93 | 65.06 | 69.27 | 30.72 |
| Care | 115 (12.2) | 69.56 | 30.43 | 87.82 | 12.17 |
| Equipment | 114 (12.1) | 18.75 | 81.25 | 59.09 | 40.9 |
| Transfer | 79 (8.38) | 31.57 | 68.42 | 85.95 | 14.03 |
| Placement of devices | 38 (4.03) | 86.84 | 13.15 | 9.37 | 90.62 |
| Others | 57 (6.05) | – | – | – | – |
MV: mechanical ventilation.
Comparisons made with the purpose of determining the possible correlation between shifts with more than 6 patients and the presence of incidents revealed a statistically significant difference (p=0.002). In the multivariate analysis we explored different variables with the aim of assessing the influence of both patient related factors and Unit related factors. The factors that proved to be statistically significant were mechanical ventilation (p=0.022), continuous renal replacement therapy (p=0.035) and the holiday period (p=0.022). In the patients with incidents, the Injury Severity Score (ISS) was significantly greater referred to both the total incidents (28±14 vs 16±13; p<0.001) and the incidents with injury (31±15 vs 17±12; p<0.001).
The response indices of the safety culture questionnaire were 81.8% in the prior survey and 69% in the survey after the study. Statistically significant improvements were recorded in several domains of the questionnaire, as summarized in Table 5.
Significant improvements in safety culture.
| Section | Domain | Significance |
| A: Hospital work area/Unit | • Active work done to improve safety | (p=0.002) |
| • Loss of punitive character | (p=0.005) | |
| • Reduction of safety problems | (p=0.046) | |
| • Good preventive systems are available | (p=0.046) | |
| D: Frequency of reported events | • Reporting of errors detected before causing injury | (p=0.000) |
| • Reporting of errors detected without the possibility of injury | (p=0.000) | |
| • Reporting of errors capable of causing injury | (p=0.000) | |
| G: Number of reported events | • Number of events reported in a year | (p=0.024) |
The findings of the instrument were used to establish the following improvements: detection of disposable material with alterations, definition of a protocol for orotracheal tube placement and maintenance, control of prescribed treatment by shifts, reduction of variability in the management of bed sores, and the creation of a communication protocol with the laboratory for the reporting of laboratory test data by telephone.
DiscussionHealthcare comprises a chain of processes with the global objective of improving patient health; however, each process can be associated to variation, failure or even error, with an important impact for the individual, society and the institutions. It is a professional and ethical imperative to recognize these situations and reduce their incidence and importance. This is particularly relevant in Emergency and Critical Care Medicine, where the similarities with high risk sectors (nuclear energy, aeronautics, petrochemical industry) are greater,22,23 the risk of error is higher, and its impact can be more serious.17,24,25
The present study describes a risk management tool referred to emergency care and the treatment of serious trauma patients. Similar experiences have been described in other settings.10,26,27
The epidemiological data of our population coincide with those contained in other trauma registries in our setting, involving young and predominantly male populations with closed traumatisms.28 The applied severity scales, the need for mechanical ventilation, the patient hemodynamic condition upon admission, and the incidence of complications all point to important severity and complexity in these subjects. The results of the TRISS methodology warrant the quality of the care provided, with improvement of the expected mortality data.
The percentage of registries with the described instrument is high, taking into account that during the study period there were several holiday periods, with an important presence of temporary personnel. Although we cannot establish comparisons, the activity of the Unit has been intense, as reflected by the occupation ratio and activities outside the ICU (transfer to the operating room, risk of falls, administration of drugs associated with risks, etc.). The instrument application time was short, thereby minimizing distraction, and could be performed at the patient bedside, with an important presence of those professionals directly implicated in patient care–thereby ensuring its incorporation to the routine of the organization. In our Department of Intensive Care Medicine we have incorporated this and other similar tools to routine practice (list of healthcare objectives, organizational goals, etc.).
The number of incidents detected with the instrument was high, probably as a result of the intense interaction with the system required in the care of critically ill and particularly seriously traumatized patients. The types of incidents detected were similar to those published in other studies (i.e., referred to medication, devices, airway, etc.).29
The present study has a number of limitations, such as the partial coverage of the instrument in registering incidents, the coexistence of this initiative with others referred to risk management and which can complicate interpretation of the impact of the results in relation to safety culture, the validation of the questionnaires in this setting, the quasi-experimental design of the study, and the Hawthorne effect. Likewise, during implementation of the instrument we experienced difficulties such as the maintenance of objective language during the meetings, and reduction of the anonymous communication of incidents. Despite these limitations, however, we consider that the tool is useful for obtaining a description of the existing safety problems of an organization, for their analysis using other types of methods such as cause-root analysis and modal analysis of failures and effects (MAFE) referred to certain techniques that may pose safety problems (e.g., renal replacement therapy), and even for explaining how barriers to incidents operate, as in the case of drug prescription in the ICU. Briefing has been shown to exert a positive influence by reinforcing the safety culture in the Unit in those aspects where it could be expected to exert a greater influence (communication of errors, loss of individual punitive character, etc.).
The study shows the feasibility of using validated tools for improving safety in certain high risk sectors such as Emergency and Critical Care Medicine. Briefing is an instrument for registering incidents that is simple, easy to use, useful for implementing improvements, and capable of exerting a positive influence upon patient safety culture.
Confidentiality and informed consentThe authors obtained informed consent from the personnel implicated in this study. The consent document is filed by the corresponding author.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Thanks are due to Dr. Abelardo García de Lorenzo and Dr. Manuel Quintana-Diaz for guidance in the development of this Doctoral Thesis.
Please cite this article as: Chico Fernández M, et al. Desarrollo de una herramienta de comunicación para la seguridad del paciente (Briefing). Experiencia en una unidad de cuidados intensivos de trauma y emergencias. Med Intensiva. 2012;36:481–7.
The results of this study have been presented as a Doctoral Thesis in the Department of Surgery of Madrid Autonomous University, receiving the qualification Apt Cum laude. Partial results have been presented at the Congress on Healthcare Quality and have been prized by the General Board of Patient Care and the Healthcare Quality Association of Madrid (Spain).