To evaluate procalcitonin clearance as a prognostic biomarker in septic shock.
DesignProspective, observational pilot study.
SettingIntensive care unit.
PatientsPatients admitted to the ICU due to septic shock and multiorgan dysfunction.
InterventionsSerum concentrations of procalcitonin were determined within 12h of onset of septic shock and multiorgan dysfunction (coinciding with admission to the ICU), and the following extractions were obtained after 24, 48 and 72h in patients who survived.
Data collectedDemographic data, Acute Physiology and Chronic Health Evaluation II score, and Sequential Organ Failure Assessment score, data on the primary focus of infection, and patient outcome (ICU mortality).
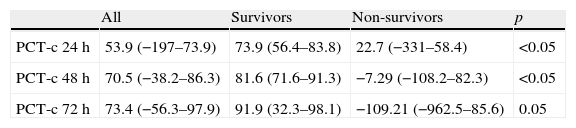
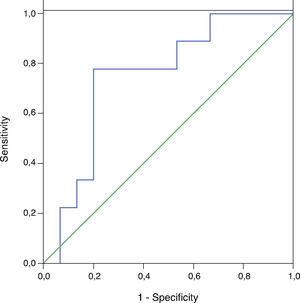
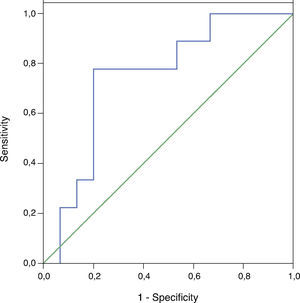
ResultsProcalcitonin clearance was higher in survivors than in non-survivors, with significant differences at 24h (73.9 [56.4–83.8]% vs 22.7 [−331–58.4], p<0.05) and 48h (81.6 [71.6–91.3]% vs −7.29 [−108.2–82.3], p<0.05). The area under the ROC curve was 0.74 (95%CI, 0.54–0.95, p<0.05) for procalcitonin clearance at 24h, and 0.86 (95%CI, 0.69–1.0, p<0.05) at 48h.
ConclusionsICU mortality was associated to sustained high procalcitonin levels, suggesting that procalcitonin clearance at 48h may be a valuable prognostic biomarker.
Evaluar el aclaramiento de procalcitonina como biomarcador pronóstico del shock séptico.
DiseñoEstudio piloto, observacional y prospectivo.
ÁmbitoServicio de Medicina Intensiva.
PacientesEnfermos ingresados en el Servicio de Medicina Intensiva por shock séptico y disfunción multiorgánica.
IntervencionesDeterminación de las concentraciones séricas de procalcitonina en las primeras 12h de evolución del shock séptico (coincidiendo con el ingreso en el Servicio de Medicina Intensiva) y posteriormente a las 24 horas, 48 horas y a las 72 horas en los pacientes supervivientes.
Variables recogidasdatos demográficos, score Acute Physiology and Chronic Health Evaluation II, score Sequential Organ Failure Assessment, datos relativos al foco de sepsis y al resultado del paciente (mortalidad en el Servicio de Medicina Intensiva).
ResultadosEl aclaramiento de procalcitonina fue mayor en los pacientes supervivientes respecto a los no supervivientes, con diferencias significativas a las 24 horas (73,9 [56,4–83,8]% vs 22,7 [−331–58,4], p<0,05) y las 48 horas (81,6 [71,6–91,3]% vs −7,29 [−108,2–82,3], p<0,05). El área por debajo de la curva ROC fue 0,74 (IC del 95%, 0,54 a 0,95, p<0,05) para el aclaramiento de procalcitonina a las 24 horas y 0,86 (IC del 95%, 0,69 a 1,0, p<0,05) para el aclaramiento de procalcitonina a las 48 horas.
ConclusionesLa persistencia de concentraciones elevadas de procalcitonina se asoció a una mayor mortalidad. El aclaramiento de procalcitonina realizado a las 48h puede ser de utilidad como biomarcador pronóstico.
Procalcitonin (PCT) has been proposed as a specific biomarker of bacterial infectious1–3 and has been related to the severity of sepsis.4 In healthy subjects, PCT concentrations are undetectable or very low (0.1–0.5ng/ml). While in colonization, local infection or viral infection PCT levels remain below 2ng/ml, in sepsis levels they often rise above 3ng/ml, and in septic shock (SS), PCT levels are even higher.5
PCT has been widely studied in patients with pneumonia6–13 as a biomarker to reduce the duration of antibiotic treatment,14–16 but no studies have investigated its evolutionary behavior specifically in patients with septic shock (SS) and multiorgan dysfunction (MODS).
The hypothesis of this study was that the evolutionary kinetics of PCT and the persistence of high PCT levels may have prognostic value and may be useful in clinical monitoring of patients with SS and MODS. PCT was determined sequentially in all patients, all with severe sepsis and MODS, in order to study the behavior of PCT levels during SS and MODS, to introduce the concept of PCT clearance (PCT-c) as a tool to assess its kinetics and to analyze its potential value as a prognostic biomarker.
Materials and methodsStudy setting and populationA prospective, observational cohort study of adult patients (over 18years) was performed. The patients were admitted to the ICU for SS and MODS in the first 12h of SS evolution. SS and MODS were defined according to the recommendations of the 2001 International Sepsis Definitions Conference.17 The study was conducted at a single center, the Critical Care Department of the Vall d’Hebron University Hospital (VH-ICU, Barcelona, Spain). VH-ICU is a medical-surgical unit with 36 beds for critically ill patients. Attending physicians are all specialists in Intensive Care Medicine, with a minimum of five years’ specialized training. All patients were admitted to VH-ICU. All patients with SS were resuscitated following our department's protocol, based on the recommendations of the Surviving Sepsis Campaign18 and the American College of Critical Care Medicine guidelines for hemodynamic support of adult patients with sepsis.19 Sepsis management was similar in all patients. A source control was performed within the first 12h of SS development, except in one patient with endocarditis (in whom mitral valve replacement was performed 24h after development of shock). The study was approved by the Clinical Research Ethics Committee of the hospital and the need for informed consent was waived.
Data collectionThe following variables were compiled for all patients: age, sex, Acute Physiology and Chronic Health Evaluation (APACHE)-II score and Sequential Organ Failure Assessment (SOFA), data on the primary focus of infection, and culture results. The APACHE-II score, SOFA and number of dysfunctional organs were calculated on ICU admission, and always within 12h of onset of SS and MODS. Organ dysfunction was defined as a SOFA score of 1 or more.20 Patient outcome (ICU mortality) was assessed retrospectively, without knowledge of PCT levels.
Blood sample collection and analysisSerial blood extractions were performed: the first or baseline was obtained within 12h of onset of SS and MODS (coinciding with the VH-ICU admission) and the following extractions were obtained at 24h, 48h, and on 72h in patients who survived (PCT-initial, PCT-12h, PCT-24h, PCT-48h and PCT-72h). The blood samples were taken from an arterial catheter placed in the radial or femoral artery, after discarding the first 3ml of blood. The blood was then distributed in sterile tubes (Vacutainer Beckton Dickinson, Plymouth, United Kingdom) supplemented with heparin and immediately centrifuged for 15min at 4200rpm and a temperature of 4°C (Laborzentrifugen SIGMA 3K10, Germany). The resulting serum was distributed in different Eppendorf aliquots of 1.5ml, for immediate storage at −80°C in a freezer (Model 825, Forma Scientific, Ohio, USA) until analysis. Patients’ attending physicians did not know the results of the PCT determinations, which were not in fact available during the study period. The PCT was determined by an immunoluminometric method, using the reagent Lumitester PCT (Brahms Diagnostica GMBH, Berlin, Germany). This technique has a functional sensitivity of 0.5ng/ml.
PCT-c was calculated using the following formula: initial PCT minus PCT at 24h, 48h and 72h, divided by initial PCT, and then multiplied by 100 (PCT-c at 24h, 48h and 72h, respectively).
Statistical analysisValues were expressed as mean (standard deviation) (age, APACHE II, SOFA) or as the median and interquartile range (25/75) in case of a skewed distribution (PCT, PCT-c). A comparison of continuous variables that did not follow normal distribution test was done using Mann–Whitney U test. The prognostic accuracy of PCT-c was expressed as the area under the receiver operating characteristic curve (AUC-ROC). Calibration of the model was assessed using the Hosmer–Lemeshow test. The optimal cut-off values were obtained using Youden's Index. Statistical analysis was performed using the SPSS 18.0 software (SPSS Inc., Chicago, IL, USA). The sensitivity, specificity, positive and negative predictive value of PCT-c were calculated from ROC curve analysis by SPSS macro for DT! (SPSS Macro ¡ROC, V2008.06.03, Universitat Autònoma de Barcelona, Spain). A p value<0.05 was considered statistically significant.
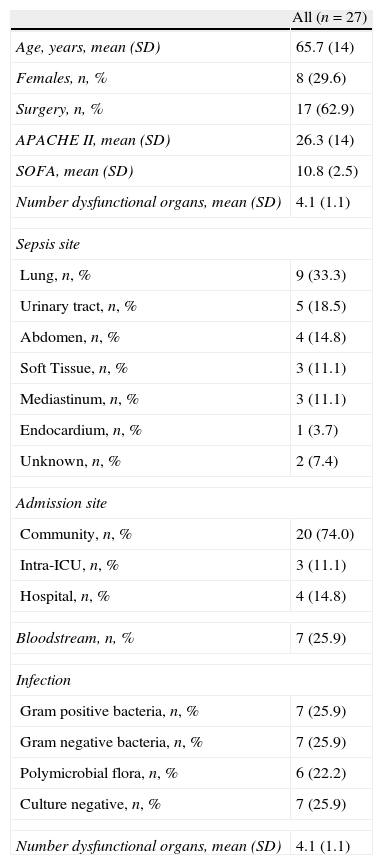
ResultsStudy populationTwenty-seven patients were included in the study. Table 1 shows characteristics of the entire cohort. Seventeen (62.9%) were surgical patients: four had secondary peritonitis, two empyema, three mediastinitis, one endocarditis, two complicated urinary tract infection, three biliary sepsis and two complicated skin and soft tissue infection. All patients had SS and 24 required mechanical ventilation (89%). Overall ICU mortality rate was 66.7% (18 patients).
Characteristics of the study cohort of 27 patients with septic shock and multiorgan dysfunction.
| All (n=27) | |
| Age, years, mean (SD) | 65.7 (14) |
| Females, n, % | 8 (29.6) |
| Surgery, n, % | 17 (62.9) |
| APACHE II, mean (SD) | 26.3 (14) |
| SOFA, mean (SD) | 10.8 (2.5) |
| Number dysfunctional organs, mean (SD) | 4.1 (1.1) |
| Sepsis site | |
| Lung, n, % | 9 (33.3) |
| Urinary tract, n, % | 5 (18.5) |
| Abdomen, n, % | 4 (14.8) |
| Soft Tissue, n, % | 3 (11.1) |
| Mediastinum, n, % | 3 (11.1) |
| Endocardium, n, % | 1 (3.7) |
| Unknown, n, % | 2 (7.4) |
| Admission site | |
| Community, n, % | 20 (74.0) |
| Intra-ICU, n, % | 3 (11.1) |
| Hospital, n, % | 4 (14.8) |
| Bloodstream, n, % | 7 (25.9) |
| Infection | |
| Gram positive bacteria, n, % | 7 (25.9) |
| Gram negative bacteria, n, % | 7 (25.9) |
| Polymicrobial flora, n, % | 6 (22.2) |
| Culture negative, n, % | 7 (25.9) |
| Number dysfunctional organs, mean (SD) | 4.1 (1.1) |
Twenty-seven PCT determinations were made at baseline, 24 at 24h, 23 at 48h and 19 at 72h. The median PCT-initial concentrations were 34.8ng/ml (11.5–110.99), 34.05ng/ml (8.6–157.8) for PCT-24h, 28.1ng/ml (5.3–126) for PCT-48h, and 7.7ng/ml (4–57.9) for PCT-72h.
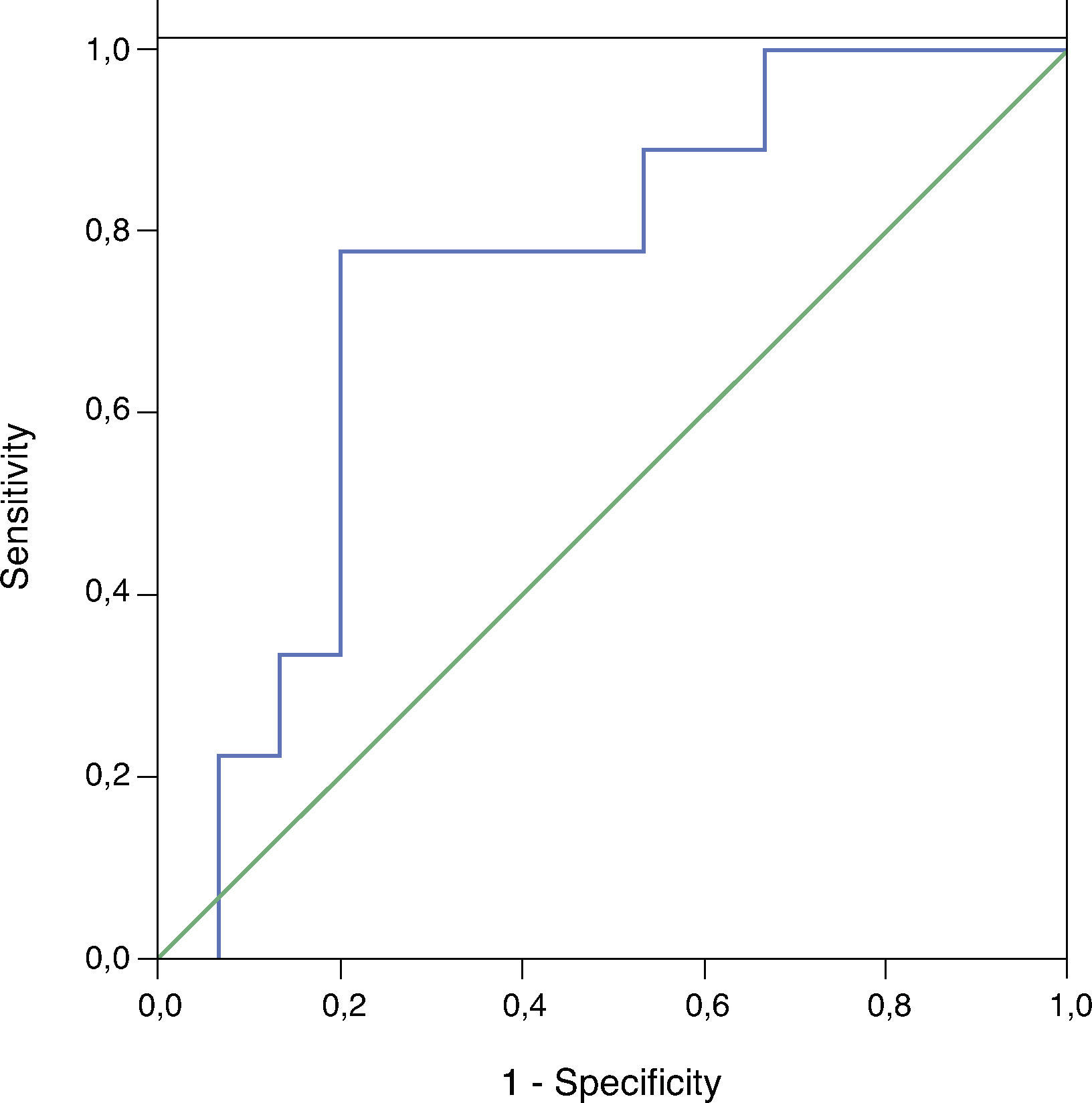
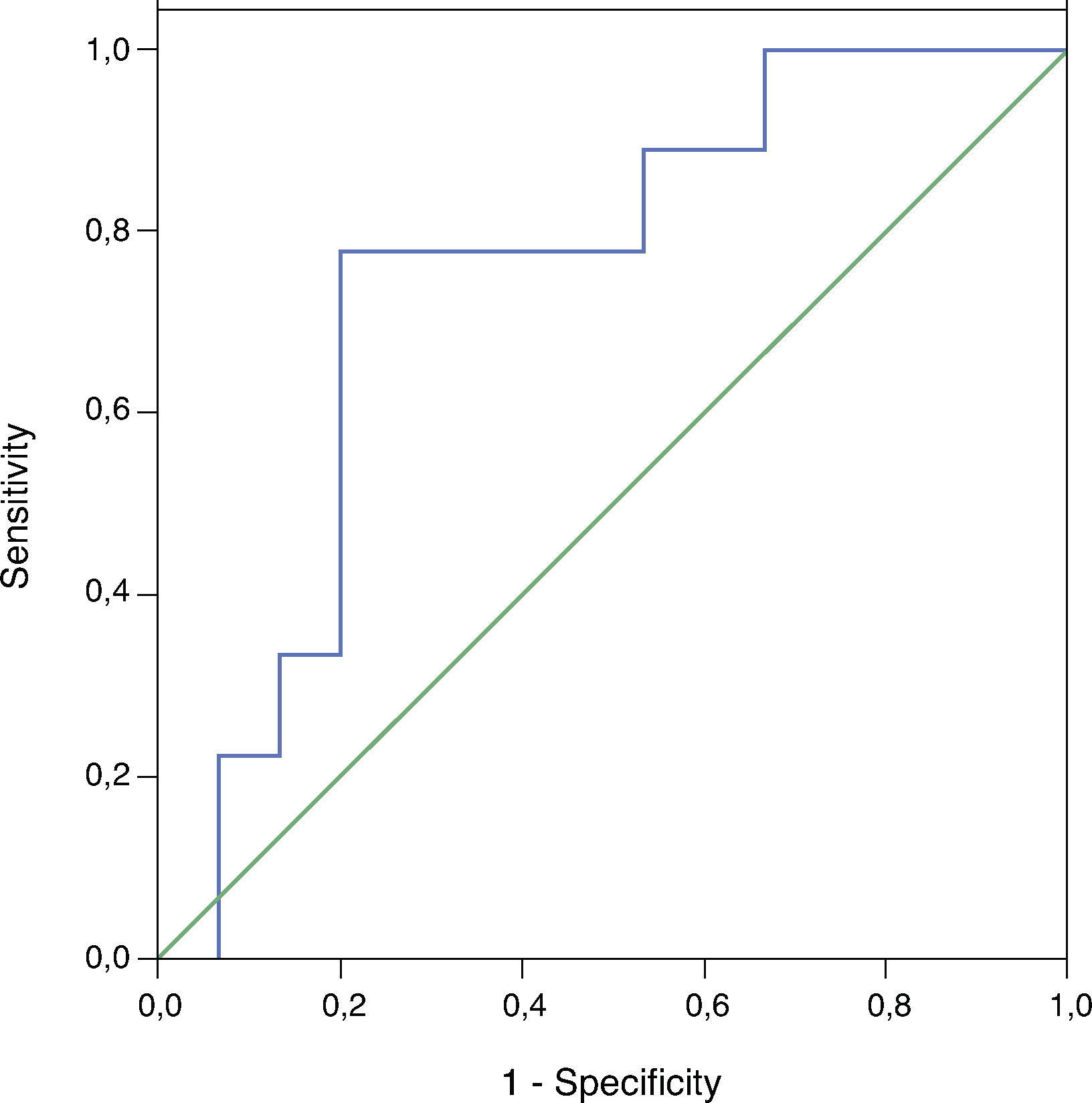
PCT-c was higher in survivors than in non-survivors, with significant differences at 24 and 48h (Table 2). PCT-c increased during the development of SS and MODS in survivors, but decreased in non-survivors. The AUC-ROC was 0.74 (95% CI, 0.54–0.95, p<0.05) for PCT-c 24h (Fig. 1) and 0.86 (95% CI, 0.69–1.0, p<0.05) for PCT-c 48h (Fig. 2). The Hosmer–Lemeshow test showed good calibration (PCT-c 24h p=0.28, PCT-c 48h p=0.78). The best cutoff for PCT-c 24h was 30%, while the best for PCT-c 48h was 50%. A cut-off value above 30% of PCT-c 24h was associated with sensitivity of 78% (95% CI, 45–94), specificity of 60% (95% CI, 36–80), positive predictive value of 54% (95% CI, 29–77), negative predictive value of 82% (95% CI, 52–95) and efficiency of 67% (95% CI, 47–82) for identifying survivors. Otherwise, a cut-off above 50% of PCT-c 48h had 89% (95% CI, 45–88) sensitivity, 71% (95% CI, 56–98) specificity, 67% (95% CI, 62–98) predictive positive value, 91% (95% CI, 39–86) negative predictive value and 78% (95% CI, 28–90) efficiency.
Although some papers have been published emphasizing the importance of measuring PCT kinetics, rather than just absolute values,4,6–7,21–24 to the best of our knowledge, this is the first study focusing exclusively on patients with SS and MODS to sequentially analyze PCT concentrations and to establish the concept of PCT-c as a biomarker for prompt evaluation of prognosis of patients with SS. PCT-c 48h quantifies the change in PCT concentrations and, in our series, a value greater than 50% is associated with good prognosis.
The initial absolute peak of PCT in the inflammatory process induced by sepsis occurs early on; it reaches a plateau value at 6–24h and has a half-life of around 24–35h.25 Significant changes induced by the therapeutic measures taken may be seen even in patients with very high initial concentrations of PCT, so high baseline concentrations are not always associated with poor prognosis. Then, the prognostic ability of the initial PCT concentrations in sepsis is controversial and while some studies find higher initial concentrations in non-survivors5–7,26–28; others find no differences.22–24,29–30
The prognostic value based on the evolution of PCT levels may be more useful than the individual evaluation of initial PCT levels. In patients with sepsis secondary to ventilator-associated pneumonia (VAP), community-acquired pneumonia (CAP) or bloodstream infection, reductions in PCT concentrations above 30% between days 2 and 3 are considered an independent predictor of survival, with an odds ratio of 2.9 (23). Surviving patients with meningococcal disease had significantly lower PCT concentrations at 6h and 12h after the onset of sepsis.29 In addition, in patients with VAP, survival was directly related to decreasing delta PCT (days 4–0) with odds ratio 4.43.6 In CAP patients the decrease of PCT from day 1 to day 3 was related to survival, with 89% specificity, 82% negative predictive value, 56% sensitivity and 71% positive predictive value.7 In patients with systemic inflammatory response syndrome and suspected infection the slow decrease or no decrease in PCT levels 48h after admission was consistently associated with a poor outcome.2 Recently, Karlsson et al.24 showed that mortality in patients with severe sepsis is lower in those in whom PCT concentrations at 72h fell by more than 50% with respect to initial values. In patients with SS, Claeys et al.22 showed that during the first 48h after admission, PCT levels significantly decreased only in surviving patients but not in non-survivors. Our results are compatible with these studies and show that a decrease in PCT during SS evolution was significantly associated with survival.
Follow-up of PCT concentrations has been used in several studies to guide antibiotic therapy. In the PRORATA trial, investigators were encouraged to discontinue antibiotics when PCT concentration was less than 80% of the peak concentration or when an absolute concentration below 0.5μg/L was reached.15 In a clinical trial of CAP, in patients with very high PCT levels on admission (e.g., greater than 10μg/L) the discontinuation of antibiotics was encouraged if levels fell to below 10% of the initial value compared with levels at days 4, 6 and 8.26 Hochreiter discontinued antibiotic therapy if PCT dropped 25–35% of the initial value over 3days.31
To our knowledge, this is the first study to develop the concept of PCT-c as a tool for assessing the evolution of PCT concentrations during the course of SS and MODS. PCT-c is an innovative concept that reflects PCT dynamics. A positive value indicates a decrease or clearance of PCT and a negative value shows an increase in PCT and persistence of its synthesis and release. In our study, PCT-c increased progressively in surviving patients but decreased in non-survivors, with significant differences at 24 and 48h. PCT-c 48h was the value that best identified the favorable evolution of our SS patients; a PCT-c 48h higher than 50% had a negative predictive value of 91%. This finding may have an impact on the management of patients with SS and MODS. The persistence of elevated PCT levels is indicative of poor prognosis. Measurement of PCT could be of great value in management of these patients, and therefore should be incorporated into the laboratory tests available in hospitals.
Our study has several limitations. The first and most important is the small sample size. The small sample size of our study could have made difficult the estimation of the AUC value with a correct accuracy. However, the result obtained with the PTC-c 48h, 0.86 with 95% CI ranging from 0.69 to 1.0 (p<0.05), is precise enough to indicate that this value is at least very close to 0.70. We consider this as an acceptable minimum value required for the AUC of any new test under investigation, so we believe that it is justified to continue working on this hypothesis. Second, these results cannot be applied to patients with localized or mild infections or those who do not have shock or do not require ICU admission. In our series, 100% of patients presented SS and APACHE II, SOFA and mortality were very high. Third, this is a prospective study of consecutive patients at a single center, and large prospective multicenter studies are necessary to confirm our results. Fourth, we did not collect information regarding the appropriateness (i.e., correct antibiotic for the pathogen causing infection) or timeliness (antibiotics administered within 3h of diagnosis of sepsis) of antimicrobial therapy. The strength of this study was that all patients included were in critical condition with SS and severe MODS, as indicated by the SOFA score and APACHE II. This consideration eliminates the bias that might have been caused by the inclusion of patients with less serious bacterial infections.
ConclusionsIn this prospective pilot study, a sustained high concentration of PCT in SS and MODS patients was associated with significantly lower survival. PCT-c appears to be a useful tool for monitoring the evolution of PCT levels during SS and MODS. The prognosis of SS and MODS can be assessed by PCT-c 48h. These findings will be useful for the design of large prospective studies including a broad case-mix.
Conflict of interestWe declare that we have no conflict of interest to disclose. No financial support was provided. The study was not funded. Atom SL donated PCT kits and facilitated the testing device without any access to data management. The company had no roles in the study design, manuscript writing or decision to submit the manuscript for publication.
We acknowledge Atom SA for providing the technical resource to carry out this study.
Prior presentation: Reported in part in abstract form at the 23rd Annual Congress of European Society of Intensive Care Medicine (October, 2010, Barcelona, Spain).