The validation in critical patients with short-term catheters of a method for diagnosing catheter-related bloodstream infection (CR-BSI), based on the differential time to positivity (DTP) of blood cultures.
MethodsPatients suspected of having CR-BSI were included. Two peripheral vein blood cultures and a catheter hub blood culture were simultaneously carried out. The responsible catheter was removed and tip cultured. Times to positivity of all blood cultures were automatically registered. CR-BSI was diagnosed when all the cultures were positive for the same microorganism and DTP≥120min. This diagnosis was compared with the one obtained using the standard method.
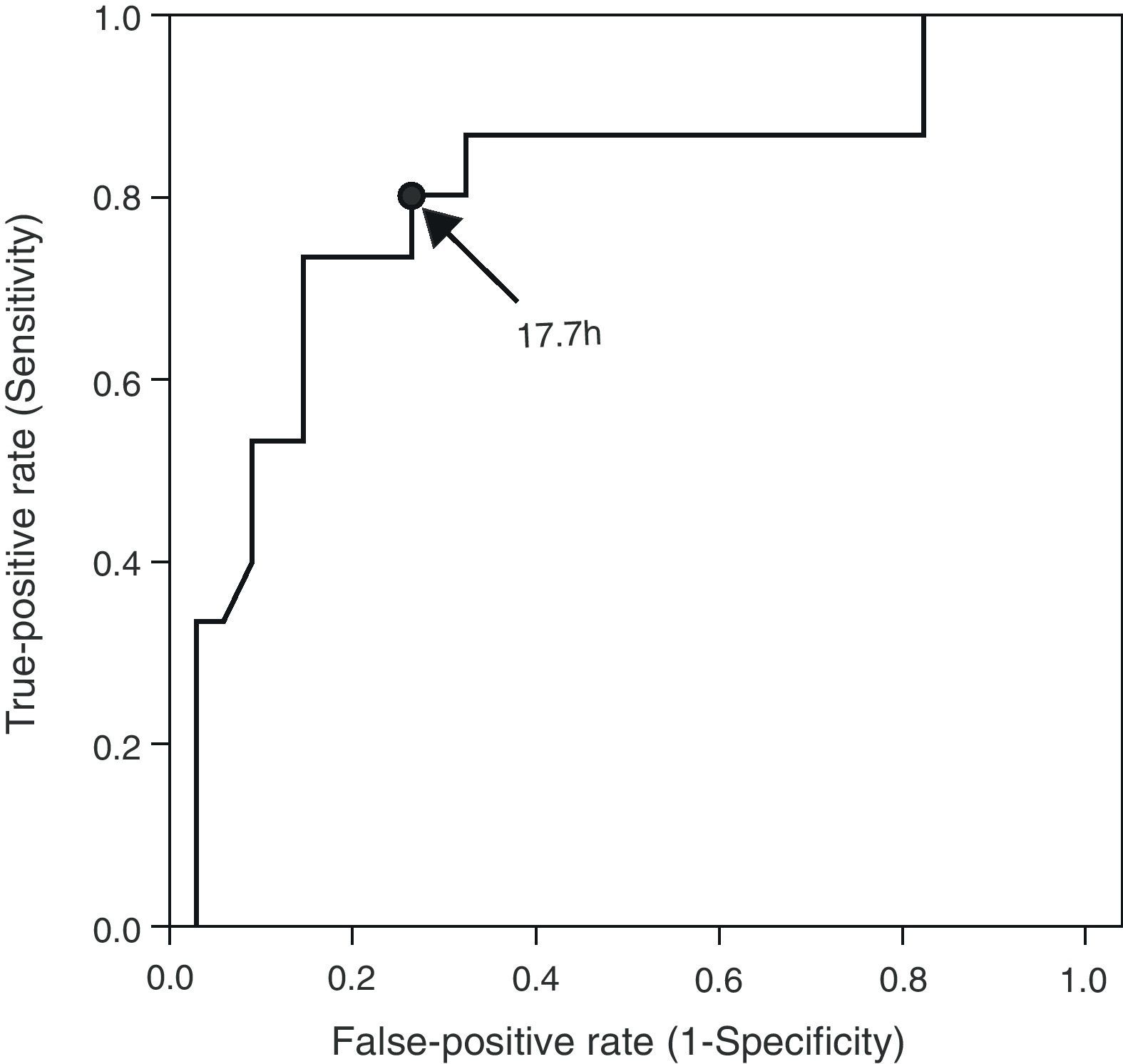
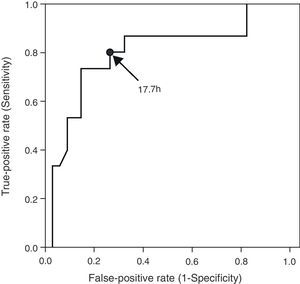
Results226 cases suspected of CR-BSI were analyzed during a 20-month period. A total of 19 removed catheters were associated with CR-BSI. Seven cases of polymicrobial cultures (4 with CR-BSI) were discarded from the final analysis due to the impossibility of determining the time to positivity for each individual microorganism. Using the DTP method, 12 out of 15 CR-BSI cases were diagnosed (sensitivity 80%, specificity 99%, PPV 92%, NPV 98%). In a ROC curve, we found a cut-off value of 17.7h in positivity of hub blood cultures that may be useful for diagnosing CR-BSI.
ConclusionDTP can be a valid method for CR-BSI diagnosis in critically ill patients, avoiding unnecessary catheter withdrawal.
La validación, en pacientes críticos con catéteres de corta duración, de un método diagnostico de la bacteriemia asociada a catéter (BAC) basado en la diferencia en el tiempo de positivización (DTP) de hemocultivos.
Material y MétodosSe incluyeron pacientes con sospecha de BAC en los que se realizaron 2 hemocultivos de sangre periférica y un hemocultivo a través de la luz distal del catéter sospechoso, antes de la retirada y cultivo de la punta del mismo. Se registraron automáticamente los tiempos de positivización de todos los hemocultivos. Diagnosticamos BAC cuando todos los hemocultivos fueron positivos para el mismo microorganismo y el DTP≥120 minutos. La exactitud de este método diagnóstico fue comparada con la obtenida mediante el método estandar.
ResultadosSe analizaron 226 casos de sospecha de BAC durante 20 meses. En 19 de ellos se diagnosticó BAC mediante el método estandar. En 7 casos los hemocultivos fueron polimicrobianos (4 de ellos asociados a BAC) por lo que tuvieron que ser descartados para el analisis final dada la imposibilidad de determiner el tiempo de positivización de cada microorganismo por separado. Siguiendo el método basado en el DTP, 12 de los 15 casos de BAC fueron diagnosticados correctamente (sensibilidad 80%, especificidad 99%, VPP 92%, VPN 98%). En una curva ROC, encontramos un punto de corte de 17.7 horas en el tiempo de positivización del hemocultivo a través de catéter que puede ser útil para el diagnóstico de BAC.
ConclusionLa DTP puede ser un método valido para el diagnostico de BAC monobacteriana en pacientes críticos con catéteres de corta duración, evitando la retirada innecesaria de catéteres.
Catheter-related bloodstream infections (CR-BSI) are among the most common nosocomial infections in critical patients and are associated with significant morbidity and mortality.1–3 Besides a conventional blood culture, the standard method of CR-BSI diagnosis involves withdrawing the infection-suspected catheter to culture the tip.4 Thus, a definitive diagnosis of CR-BSI can be only established retrospectively, when the same pathogen is isolated from both the blood and the catheter tip cultures. Only 15–20% of the catheters withdrawn turn out to be responsible for the bloodstream infection. The need for a reliable method to assess CR-BSI without catheter withdrawal has led to the development of diverse catheter-conserving methods in recent years.5,6
One such method is the differential time to positivity (DTP) between blood cultures obtained from the catheter hub and peripheral blood. This method, which has already been validated for long-term catheters,7,8 is based on the direct relationship between the blood bacterial load and the time required for a positive culture. If the catheter is the source of infection, the blood from the hub will have a higher bacterial load and therefore the time to culture positivity will be shorter compared to that of the peripheral blood culture.
However, when tested in short-term catheters or patients without malignancy, the DTP method has yielded discrepant results.9–12 We aimed to validate the method in short-term catheters, which are commonly used in the intensive care unit.
Materials and methodsWe included prospectively all patients with a central venous catheter in place for more than 72h, admitted to the medical-surgical critical care unit of our institution (Hospital de Sabadell, Barcelona, Spain) between February 2005 and September 2006 and clinical symptoms of infection like fever, leukocytosis or shock, in whom other possible sources of infection, different than a possible CR-BSI, were previously ruled out. The hospital's Ethics Committee approved the study and waived the requirement for patient consent due to the observational nature of the study, the anonymous data collection and because all the clinical procedures, except one single blood culture (the hub-blood one), represented standard of care in these patients since every patient in our unit with a suspected CR-BSI had two peripheral blood cultures and removal of every catheter in place for more than 72h as the standard or care. We excluded patients with long-term (≥30 days) or Swan-Ganz catheters.
For each suspected case, the following samples were collected and processed:
- -
Two serial blood samples (10ml of blood each sample) from a peripheral vein obtained 30min apart. Samples were cultured in aerobic (5ml) and anaerobic (5ml) media.
- -
One blood sample from the distal lumen of the catheter (first 5ml of blood after discarding non-hematological contents), which was cultured in aerobic media, at the same time of the first peripheral blood sample.
- -
The suspected catheters were withdrawn and the tip (3–5cm) was processed for quantitative cultures followed by semi-quantitative ones, as established by guidelines and previous studies.14,16 Positivity was defined as the growth of ≥103 colony forming units (CFU) per catheter segment according to Cleri's modified method for quantitative cultures13 and as ≥15 CFU per segment for semi-quantitative cultures according to Maki's method.14
At the time of sample collection, the nurses had to fill out an application form indicating the amount of blood filled in each culture bottle. When the quantity of blood was not enough to fill 5ml in each culture bottle, samples were discarded for the study and not included in the DTP calculations. All blood samples were simultaneously sent to the laboratory to be processed using an automatic culture detector (BacT/ALERT; bioMerieux, Durham, North Carolina, USA), and the time to positivity of each culture was registered. Differential time to positivity was defined as the difference in the time required for a positive culture between peripheral blood and hub-blood (DTP=time to positivity hub-blood culture−time to positivity peripheral blood culture).
We also recorded demographic data, pathological history, comorbidities, ICU length of stay, duration of antibiotic treatment, immunosuppression, sepsis symptoms, signs of local infection at the catheter insertion site, and evolution after catheter withdrawal.
Some patients had more than one catheter that could be considered responsible of the BSI. For this reason, each catheter was considered as a separate case.
Each suspected case was diagnosed using 2 methods: isolation of the same pathogen from catheter-tip and peripheral blood cultures (the standard diagnosis) and the DTP method. The standard diagnosis was based on the clinical and microbiological criteria defined in the clinical guidelines4,15,16 Due to the results shown in previous studies using a combination of quantitative and semi-quantitative methods13 we consider a sensitivity and specificity of 100%. For this method, we used the following definitions:
- (A)
CR-BSI: a positive peripheral blood culture in which the microorganism isolated is identical in species and antibiogram to the catheter-tip culture by either the quantitative or the semi-quantitative method.
- (B)
Non-catheter-related bloodstream infection (non-CR-BSI): a positive peripheral blood culture in which the pathogen isolated was different from the one isolated in the catheter-tip culture, or when catheter-tip culture was negative.
When the blood cultures are negative but the catheter-tip culture is positive either by the quantitative or semi-quantitative culture method, it is considered as catheter colonization. For the study analysis, we included them in the non-CR-BSI diagnostic group.
This diagnosis was determined by clinicians who were blinded to the DTP status, and the patients were managed according to the standard diagnosis, looking for other source of bloodstream infection in the cases diagnosed as non-CR-BSI with positive blood cultures.
For the diagnosis based on the DTP method definitions were:
- (A)
CR-BSI: a positive peripheral blood culture in which the microorganism isolated was identical in species and antibiogram to the hub blood culture when the hub blood culture yielded positive results at least 120min earlier than the peripheral blood cultures.
- (B)
Non-CR-BSI: a positive peripheral blood culture when the hub blood culture was either negative or positive for the same pathogen but the differential time to positivity of the cultures was shorter than 120min.
We could consider catheter colonization when the hub blood culture was positive but the pathogen isolated was different from the one isolated in peripheral blood cultures or when peripheral blood cultures were negative. For the study analysis, as we did with the standard method, we included these cases in the general non-CR-BSI diagnosis.
Cases with polymicrobial cultures were classified as undetermined and excluded from the analysis due to the impossibility of determining the time to positivity for each individual microorganism since the detector only provides the generic time to positivity of the blood culture without taking into account the presence of colonies from different pathogens.
All clinical and therapeutic decisions were based on the results obtained by the standard diagnostic method.
Statistical analysisSensitivity, specificity, positive and negative predictive values and likelihood ratios were determined for a DTP≥120min compared with the standard diagnosis. Differential times to positivity for CR-BSI cases and non-CR-BSI were compared by the Mann–Whitney test. All P-values were based on two-tailed tests (level of significance, P<0.05). We constructed a receiver-operator characteristic (ROC) curve by plotting the true-positive rate (sensitivity) against the false-positive rate (1 – specificity) over a range of cutoff values for time to positivity of the hub blood cultures in patients with CR-BSI. Spearman's rank correlation coefficient was used to calculate the relationship between the number of positive blood cultures and the time to positivity. Linear regression was used to assess a potential relationship between number or antibiotic days and time to positivity of blood cultures.
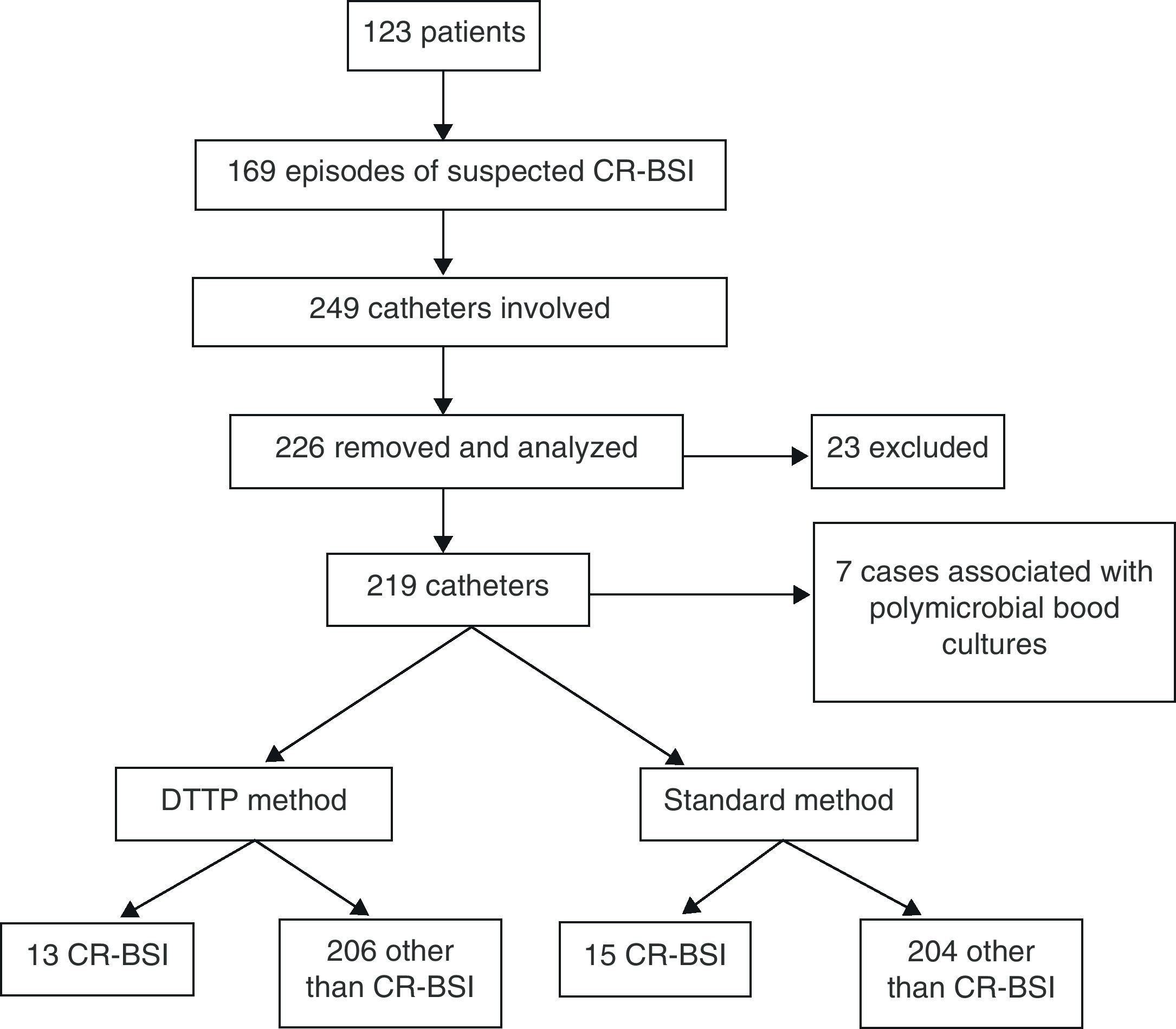
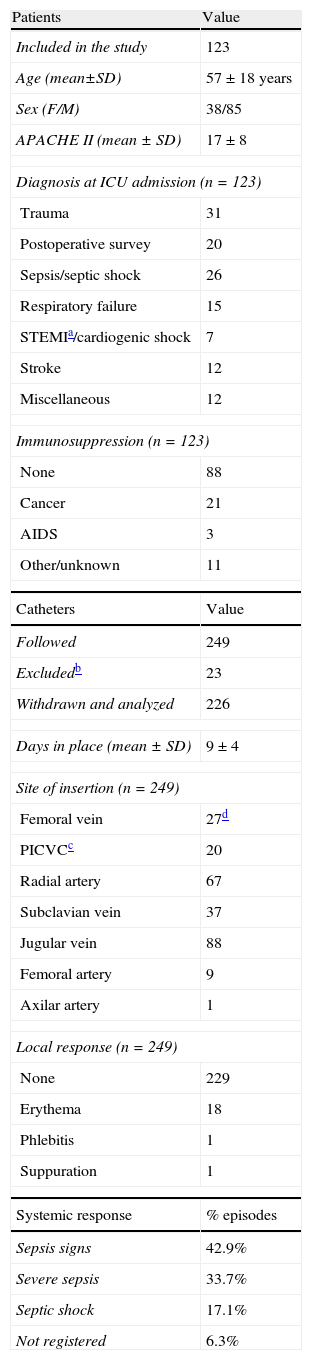
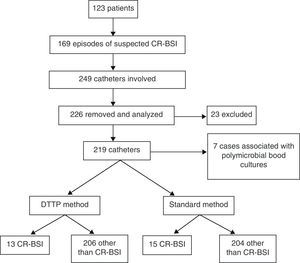
ResultsWe included 226 catheters in a total of 163 episodes of suspected CR-BSI. As previously commented, each catheter was cataloged as a case of suspected CR-BSI due to the fact that one episode could involve more than one catheter. Fig. 1 summarizes the flow of patients and cases as a diagram.
Table 1 summarizes patient and catheter characteristics. The insertion sites most commonly associated with suspected CR-BSI were the internal jugular vein followed by the radial artery, which are the two most common insertion sites in our ICU. Among confirmed CR-BSI cases, jugular and subclavian veins were the most frequent catheters sites. The most frequently isolated pathogen was Staphylococcus epidermidis, followed by other coagulase-negative staphylococci and other less frequent bacteria. Table 2 shows the characteristics, times to positivity and differential times to positivity of the 17 cases with positive paired monobacterial blood cultures as well as the standard and DTP diagnosis in each case. Signs of local infection were present in 20 of the 226 withdrawn catheters (erythema in 18 cases). In all cases, local signs of infection improved or completely disappeared within 48h of catheter withdrawal. In 105 of the 163 cases of suspected CR-BSI, patients were receiving antibiotics prior to blood culture sampling (mean length of antibiotic treatment 5.2±6.2 days). We assessed the relationship between antibiotic treatment and blood culture results to exclude potential confounding. We did not find an association between prior antibiotic treatment and blood culture results (the mean length of antibiotic treatment in the subgroup with any positive blood cultures was 4.8±5.3 days and 5.4±6.8 days in the subgroup with negative blood cultures, P=0.9). In addition, the length of antibiotic treatment did not correlate with the time to positivity of blood cultures.
Characteristics of patients and catheters.
| Patients | Value |
| Included in the study | 123 |
| Age (mean±SD) | 57±18 years |
| Sex (F/M) | 38/85 |
| APACHE II (mean±SD) | 17±8 |
| Diagnosis at ICU admission (n=123) | |
| Trauma | 31 |
| Postoperative survey | 20 |
| Sepsis/septic shock | 26 |
| Respiratory failure | 15 |
| STEMIa/cardiogenic shock | 7 |
| Stroke | 12 |
| Miscellaneous | 12 |
| Immunosuppression (n=123) | |
| None | 88 |
| Cancer | 21 |
| AIDS | 3 |
| Other/unknown | 11 |
| Catheters | Value |
| Followed | 249 |
| Excludedb | 23 |
| Withdrawn and analyzed | 226 |
| Days in place (mean±SD) | 9±4 |
| Site of insertion (n=249) | |
| Femoral vein | 27d |
| PICVCc | 20 |
| Radial artery | 67 |
| Subclavian vein | 37 |
| Jugular vein | 88 |
| Femoral artery | 9 |
| Axilar artery | 1 |
| Local response (n=249) | |
| None | 229 |
| Erythema | 18 |
| Phlebitis | 1 |
| Suppuration | 1 |
| Systemic response | % episodes |
| Sepsis signs | 42.9% |
| Severe sepsis | 33.7% |
| Septic shock | 17.1% |
| Not registered | 6.3% |
STEMI: ST-elevated myocardial infarction.
Catheters excluded from the analysis due to the lack of complete data (8 catheters) or because the catheter was not withdrawn due to low-level suspicion of CR-BSI.
PICVC: peripherally inserted central venous catheter.
4 were dialysis catheters.
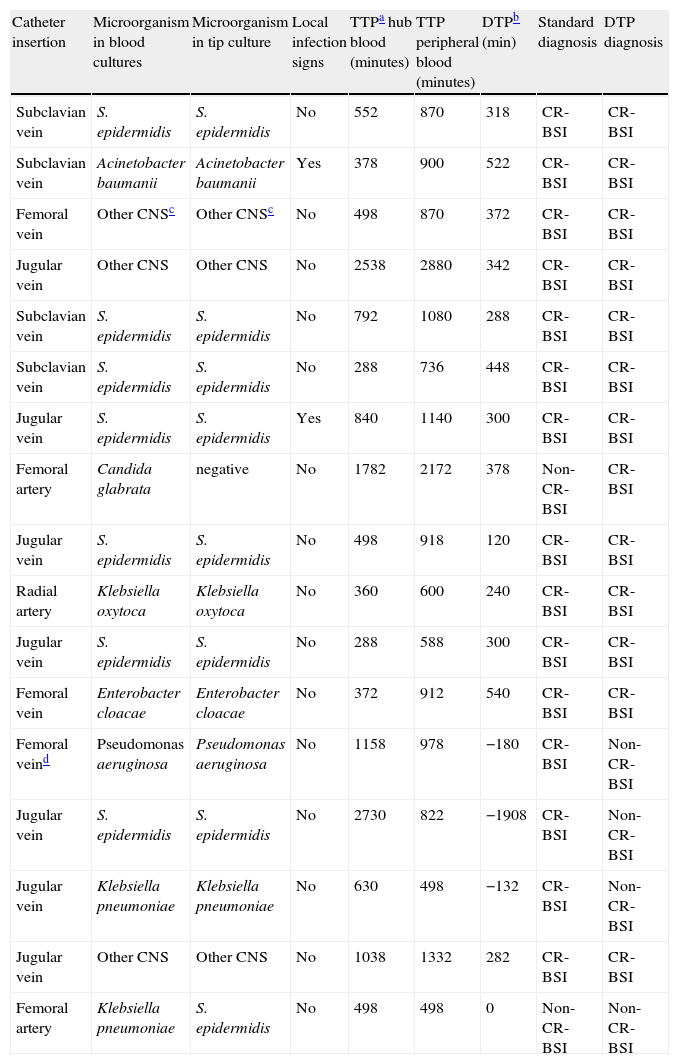
Positive paired monobacterial blood cultures.
| Catheter insertion | Microorganism in blood cultures | Microorganism in tip culture | Local infection signs | TTPa hub blood (minutes) | TTP peripheral blood (minutes) | DTPb (min) | Standard diagnosis | DTP diagnosis |
| Subclavian vein | S. epidermidis | S. epidermidis | No | 552 | 870 | 318 | CR-BSI | CR-BSI |
| Subclavian vein | Acinetobacter baumanii | Acinetobacter baumanii | Yes | 378 | 900 | 522 | CR-BSI | CR-BSI |
| Femoral vein | Other CNSc | Other CNSc | No | 498 | 870 | 372 | CR-BSI | CR-BSI |
| Jugular vein | Other CNS | Other CNS | No | 2538 | 2880 | 342 | CR-BSI | CR-BSI |
| Subclavian vein | S. epidermidis | S. epidermidis | No | 792 | 1080 | 288 | CR-BSI | CR-BSI |
| Subclavian vein | S. epidermidis | S. epidermidis | No | 288 | 736 | 448 | CR-BSI | CR-BSI |
| Jugular vein | S. epidermidis | S. epidermidis | Yes | 840 | 1140 | 300 | CR-BSI | CR-BSI |
| Femoral artery | Candida glabrata | negative | No | 1782 | 2172 | 378 | Non-CR-BSI | CR-BSI |
| Jugular vein | S. epidermidis | S. epidermidis | No | 498 | 918 | 120 | CR-BSI | CR-BSI |
| Radial artery | Klebsiella oxytoca | Klebsiella oxytoca | No | 360 | 600 | 240 | CR-BSI | CR-BSI |
| Jugular vein | S. epidermidis | S. epidermidis | No | 288 | 588 | 300 | CR-BSI | CR-BSI |
| Femoral vein | Enterobacter cloacae | Enterobacter cloacae | No | 372 | 912 | 540 | CR-BSI | CR-BSI |
| Femoral veind | Pseudomonas aeruginosa | Pseudomonas aeruginosa | No | 1158 | 978 | −180 | CR-BSI | Non-CR-BSI |
| Jugular vein | S. epidermidis | S. epidermidis | No | 2730 | 822 | −1908 | CR-BSI | Non-CR-BSI |
| Jugular vein | Klebsiella pneumoniae | Klebsiella pneumoniae | No | 630 | 498 | −132 | CR-BSI | Non-CR-BSI |
| Jugular vein | Other CNS | Other CNS | No | 1038 | 1332 | 282 | CR-BSI | CR-BSI |
| Femoral artery | Klebsiella pneumoniae | S. epidermidis | No | 498 | 498 | 0 | Non-CR-BSI | Non-CR-BSI |
TTP: time to positivity of blood cultures.
DTP: differential time to positivity.
CNS: coagulase negative staphylococci.
Dialysis catheter.
Using the standard diagnostic method, we determined that catheters were the cause of bloodstream infection in 19 cases (8.4% of withdrawn catheters), including 4 cases of polymicrobial infection. CR-BSI was ruled out in 207 cases, 3 of them associated to polymicrobial cultures. In 55% of the catheters withdrawn, all cultures were negative and no bloodstream infection was demonstrated, so it was unnecessary to withdraw the catheter. As Table 3 shows, the DTP method correctly identified 12 of the 15 cases of non-polymicrobial CR-BSI diagnosed by the standard method. The 3 missed cases were diagnosed as non-CR-BSI because the DTP was lower than 120min. On the other hand, only one of the cases diagnosed as CR-BSI according to the DTP method was classified as non-CR-BSI with the standard method, because the catheter-tip culture yielded a negative result.
Comparison between the gold standard diagnoses and differential time to positivity-based diagnoses in monobacterial cultures.
| STANDARD DIAGNOSIS | |||
| DTP-BASED DIAGNOSIS | CR-BSI | Other than CR-BSI | |
| CR-BSI | 12 | 1 | |
| Other than CR-BSI | 3 | 203 | |
Sensitivity 80% (95% CI 56–100) +LR 163.
Specificity 99% (95% CI 98–100) - LR 0.2.
Negative predictive value 98% (95% CI 96–100).
Positive predictive value 92% (95% CI 73–100).
These data yielded 80% sensitivity (95% CI 56–100), 99% specificity (95% CI 98–100), 92% positive predictive value, and 98% negative predictive value, positive likelihood ratio of 163 and negative likelihood ratio of 0.2 for the DTP method in the diagnosis of CR-BSI (see Table 3).
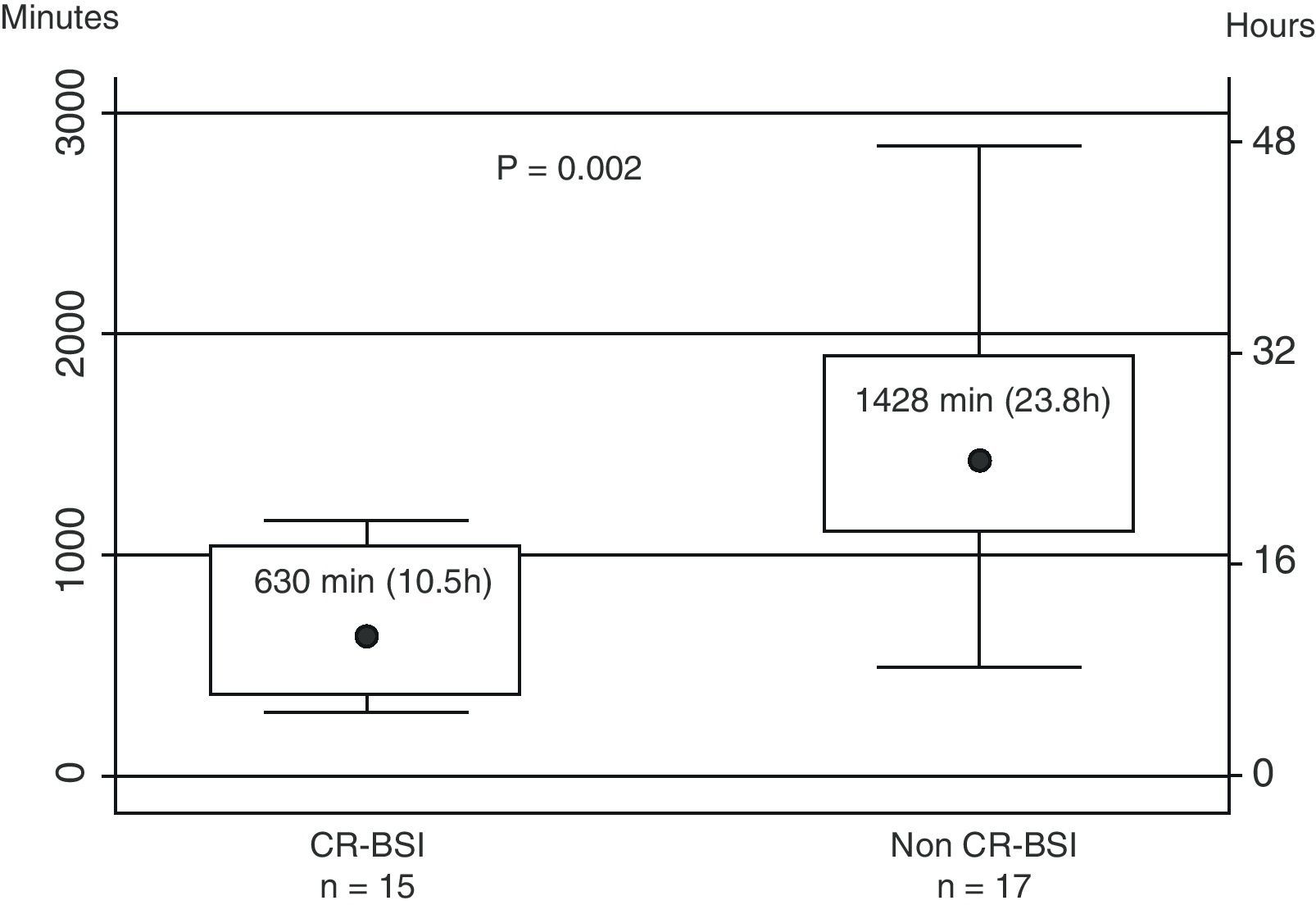
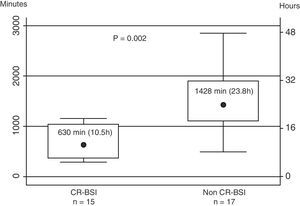
The median time to positivity of the catheter hub cultures was 630min for CR-BSI cases and 1428min for non-CR-BSI cases (P=0.002) (Fig. 2). The time to positivity of the blood culture was longer than 24h in only one CR-BSI case.
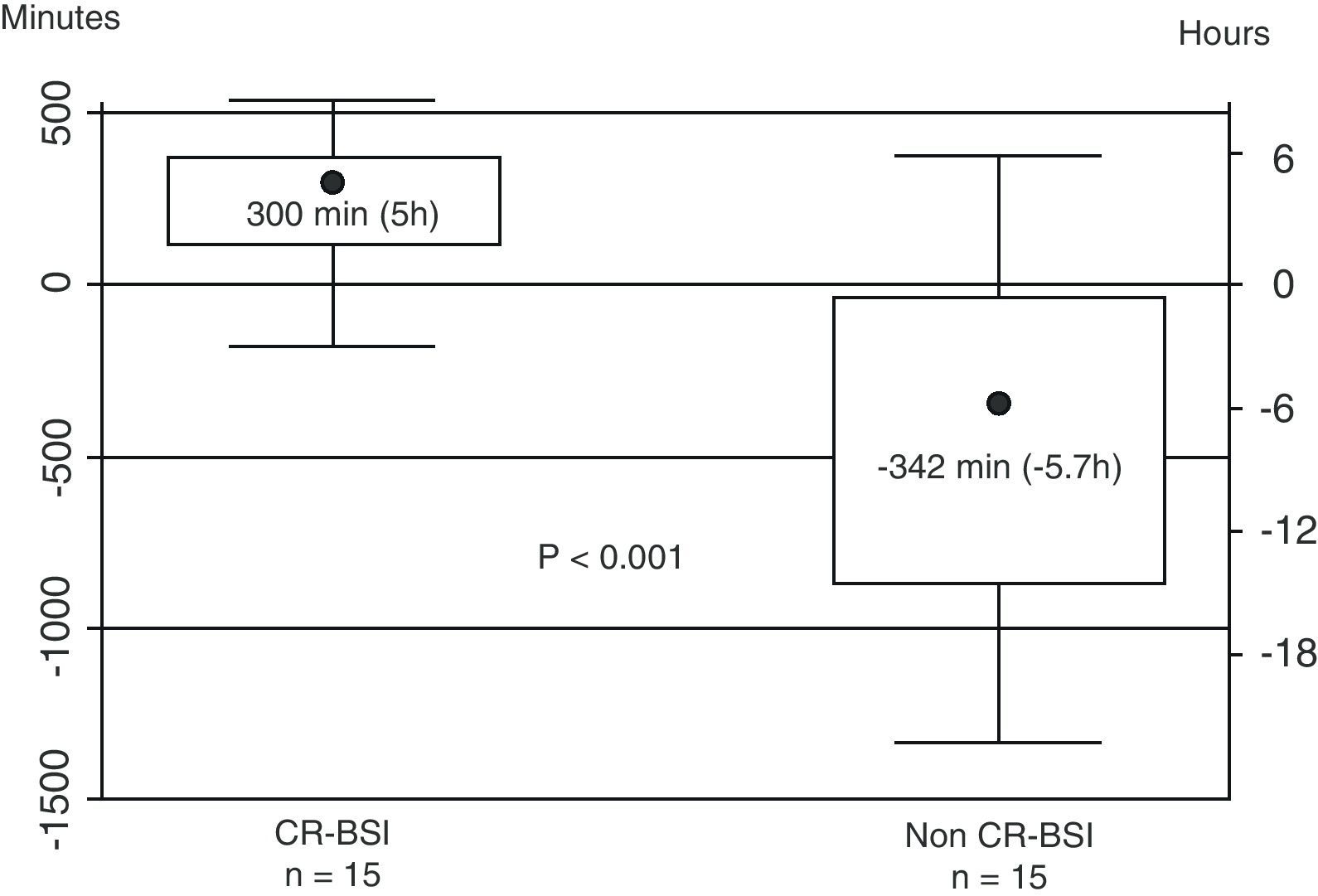
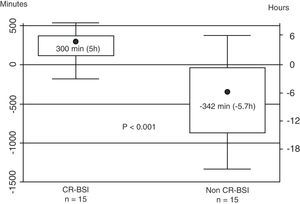
The median DTP for CR-BSI (300min) was significantly higher than the DTP for non-CR-BSI (−342min) (P<0.001) (Fig. 3).
Median differential time to positivity of blood cultures. Data are depicted as box plots: black circles indicate medians, boxes show the IQRs (25-75%), and the whiskers extend to 1.5 times the IQRs. Only in 15 non-CR-BSI cases, the microorganism isolated in hub blood cultures and peripheral blood cultures was identical in species and antibiogram so DTP could be calculated.
We found a significant correlation between the number of positive peripheral blood cultures and the time to positivity of the hub blood cultures (r=0.397, P=0.002). We were unable to find a DTP threshold with a higher sensitivity than 120min (data not shown).
The ROC curve shows that a cut-off value of 17.7h for positivity of the hub blood culture in CR-BSI cases yields 80% sensitivity and 73% specificity (see Fig. 4).
DiscussionOur study aimed to validate the utility of DTP of blood cultures for CR-BSI assessment in short-term catheters.
We found a low prevalence of CR-BSI, 8.4% of all suspected cases included in our study. The use of chlorhexidine for prophylaxis against CR-BSI in our unit could explain this low incidence of CR-BSI. Only 19 of the 226 catheters withdrawn were found to be the source of the bloodstream infection; thus, catheter withdrawal was unnecessary in the remaining 207 cases. These results strongly corroborate the need for a reliable diagnostic method to avoid unnecessary catheter withdrawal in cases of suspected CR-BSI.
The DTP method is based on the assumption that hub-blood has a higher bacterial load than peripheral blood in CR-BSI cases and therefore the time required to yield a positive culture is shorter. Our study favors this hypothesis: we found statistically significant differences in the median times to positivity for CR-BSI hub blood cultures compared to non-CR-BSI (Fig. 2), and the correlation found between the time to positivity of blood-hub cultures and the number of positive peripheral blood cultures also proves the methodological basis of the diagnostic method. The fact that the DTP was significantly longer in CR-BSI than in non-CR-BSI (Fig. 3) supports the usefulness of this method for short-term catheters used in critically ill patients without malignancy. The median values of DTP in our study are similar to those reported by Blot et al. in long-term catheters.7
Our data do not allow us to determine the relationship between different pathogens and the time to positivity as other studies did,17 probably because of the low prevalence of CR-BSI in our sample. Unlike other authors,11 we had no difficulties in obtaining samples via central venous catheters.
Previous studies about the DTP method have yielded disparate results. Rijnders et al.9 found no differences between mean DTP in blood cultures in patients with and without CR-BSI, but their only criterion for positivity was quantitative cultures from the tip of the central venous catheter. Conversely, using quantitative and semi-quantitative catheter-tip cultures in short-term catheters, Raad et al.8 reported similar sensitivity and specificity to ours. In a more recent study, Bouza et al.12 found higher sensitivity (96.4%) for DTP than we did (80%). On the other hand, the specificity and positive predictive value are higher in our study (99% vs 90.3% and 92% vs 61.4%, respectively) even when the prevalence of CR-BSI in their sample was higher than in ours (13.7% vs 8.4%, respectively). The same study evaluated the accuracy of other conservative techniques for the diagnosis of CR-BSI like the semi-quantitative cultures from hub and superficial skin, reporting a lower specificity and predictive values when comparing to our results; or the differential quantitative blood cultures, also with lower sensitivity, specificity and predictive values.
To our knowledge, none of the previous studies excluded samples with polymicrobial cultures, and this might account for the higher specificity in our study. Indeed, the impossibility of applying DTP in cases with polymicrobial cultures is, in our opinion, the major drawback of this approach, because it requires withdrawing the catheters from all patients with polymicrobial cultures for safety reasons given that the technique clearly fails in these cases, because the detector only provides the generic time to positivity of the blood culture. However, the number of cases with polymicrobial cultures in our study was low (7 cases out of 226 catheters, 4 of which were associated with CR-BSI). Furthermore, most cultures become positive within the first 24h, enabling the catheter to be withdrawn early enough in cases with polymicrobial cultures.
We suggest an initial approach to the diagnosis of CR-BSI in ICU patients using the DTP method. When a positive non-polymicrobial blood culture is found in a stable patient, it is advisable to wait until all cultures reach positivity, then determine the differential time to positivity, and finally proceed to immediate catheter withdrawal when both blood cultures are positive for the same microorganism and DTP≥120min. When both peripheral and catheter-hub bood cultures are positive for the same pathogen but the DTP is less than 120min or when hub blood culture are negative, which suggests non-CR-BSI, we see no need for catheter withdrawal. If any blood culture is polymicrobian, we recommend removal of the suspected catheter, because we cannot reliably use the DTP diagnosis in this case. The high negative predictive value of the DTP method (98%) and the low prevalence of CR-BSI suggest a low probability of CR-BSI in cases with negative hub blood cultures within the first 24h. The ROC curve analysis yielded a cut-off point of 17.7h for positivity of hub blood cultures; thus, a suspicious catheter can be removed if its hub blood culture is positive before this time and the peripheral blood samples are still negative 120min later. This means that, in most cases, within 20h after sampling, we either have a diagnosis of CR-BSI and remove the catheter or we can safely leave it because the probability of CR-BSI is very low. The very high specificity and positive likelihood ratio encourage immediate removal of the catheter once the diagnosis of CR-BSI has been made. This approach suggests that in those cases with only the hub blood culture positive catheter is going to be removed, even when it could be catheter colonization and, in some units, the management could be only antibiotic treatment without catheter removal.
We believe it is reasonable in immunosuppressed or unstable patients with suspected CR-BSI to remove the catheter without waiting for the DTP result; however, in our sample, signs of hemodynamic instability were present in only 17.1% of cases, similar to other studies conducted in our country.18
Our study has important limitations. First, being a single-center study, our findings may not be generalizable to other hospital settings. Second, the fact that hub blood cultures were obtained from the distal lumen of the catheter could decrease the sensibility to detect CR-BSI and favor detection of endoluminal infections, as described elsewhere.19 Furthermore, one of the limitations of the DTP method is that it applies better when both (hub an peripheral) blood cultures are positive and DTP can be calculated. Cases with only one positive blood culture could be harder to interpret, as mentioned before. Finally, in cases involving coagulase negative staphylococci, even an identical case in species and antibiogram may not be enough to affirm that the microorganism is the same. As described above, decision-making in our study was based on clinical findings and, for a routine use, the phenotypical criteria are simple, fast and affordable for all the laboratories, allowing to know the result in a few hours. The more advanced genotypical techniques are reserved for special or discrepancy situations.
ConclusionsOur study shows that the application of the method based on the DTP of hub blood and peripheral blood cultures might be useful in clinical practice to assess CR-BSI in suspected short-term catheters used in critically ill patients. Despite the above-mentioned limitations, the application of this method can help avoid unnecessary catheter withdrawal in patients with suspected CR-BSI.
Further prospective studies could be useful to demonstrate the usefulness of the DTP method without increasing patient risk in clinical practice.
FundingThis study was supported with a grant of the Institutional Research Committee 2004, Fundació Parc Tauli, Sabadell, Spain. The preliminary results of this study were communicated on the ESICM 20th Annual Congress in Berlin, October 2007.
Conflict of interestThe authors have no conflict of interest to declare.
Authors want to thank Jaume Mesquida for his helpful comments and Florian B. Mayr for his careful review of this manuscript and helpful comments.