Edited by: Rosario Amaya Villar - Unidad de Cuidados Intensivos, Hospital Universitario Virgen del Rocio, Sevilla, España
Last update: December 2023
More infoIn patients undergoing mechanical ventilation (MV), patient-ventilator asynchrony (PVA) is a common phenomenon associated with poor clinical outcomes including increased mortality and longer duration of MV.1,2,3 Our group have previously shown that proper identification and management of PVA at the bedside, using waveform analysis, is very challenging for health care professionals (HCPs) regardless of profession and clinical experience.4,5 Although, some studies have shown the effects of a specific training program on the ability of HCPs to identify PVA,4,5,6,7 no studies have currently explore the effect of a training program on the ability of HCPs to determine potential causes and management of PVA.
The aim of the scientific letter is to communicate the effect of a specific training program on the ability of HCPs, with less than one year of clinical experience, to identify and determine potential causes and management of PVA. This pilot study was approved by the Ethics committee of the Hospital Clínico de la Universidad de Chile (File N° 1097/20).
We conducted a quasi-experimental study in which an invitation was sent to HCPs from 20 hospitals in Latin America to participate in a specific online training program designed to assess the effect on proper recognition, management, and determine the potential causes of PVA. The inclusion criteria for HCPs were: 1) less than one year of experience proven by a certificate validated by their hospitals; 2) HCPs without formal training on PVA; 3) Currently experience working in the ICU and mechanically ventilated patients.
The program included 6 h of live streaming using the ZOOM® platform in which HCPs could interact with the instructor. Subsequently, HCPs had access to interact with the instructor for a period of one month after they completed the program using an online direct contact. An assessment tool was designed and validated by three experts with an inter-observer agreement of 100%. The assessment tool included 30 multiple choice questions divided into three sections: Fifteen questions related to PVA identification, seven on PVA management, and eight question related to the potential PVA cause. The assessment tool was applied at the beginning of the program, immediately after the 6 h live session, and one month after the live session. The clinical cases used on the assessment tool were shown by the instructor, and a link with the multiple-choice sheet was sent to HCPs to register their answers. In order to avoid any answer bias, no feedback regarding correct answers was given until the one-month evaluation was completed. The sphericity assumption (equal variance hypothesis) was tested using the Mauchly test. A comparison of participants’ performance between the three measurement periods was performed using the ANOVA test for repeated measures. Post hoc analysis was performed using the Bonferroni correction. The JASP statistical software (JASP Team 2020. Version 0.14.1) was used.
Thirteen of the 30 study participants completed all three assessments. Seven were physical therapists/respiratory therapists, and six were physicians. Four professionals were from Chile, three from Brazil, two from Ecuador, and one from Mexico, Argentina, Spain, and Colombia.
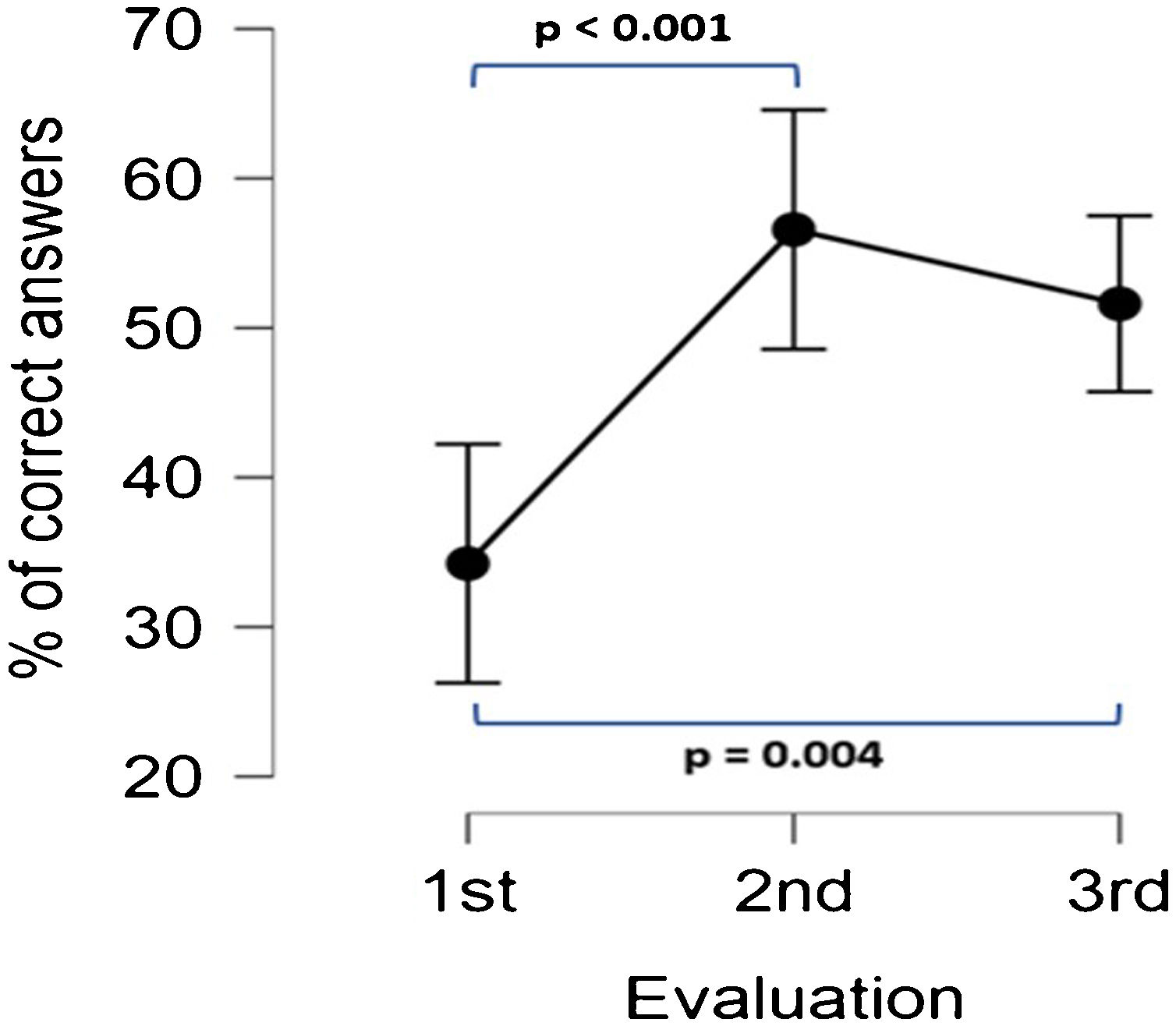
Compared to the baseline evaluation, the mean percentage of correct answers for all questions significantly increased from 34.24% (SD 20.72) to 56.58% (SD 22.95) and 51.61% (SD 23.15) immediately after the training program and one-month follow-up (ANOVA (F = 12.07; p < 0.001; post hoc; p < 0.001 and p < 0.004 respectively). No significant difference was observed between the assessment immediately after the training program and the one-month follow-up (p = 0.927) (Fig. 1).
Overall, there was a statistically significant difference in the percentage of correct responses in the identification of PVA, the determination of the possible cause of PVA, and the management of PVA. In addition, when comparing different time points, a statistically significant difference in the percentage of correct responses in the identification of PVA (F = 8.56, p = 0.002), the determination of the possible cause of PVA (F = 6.01, p = 0.008), and the management of PVA (F = 5.31, p = 0.012) was observed.
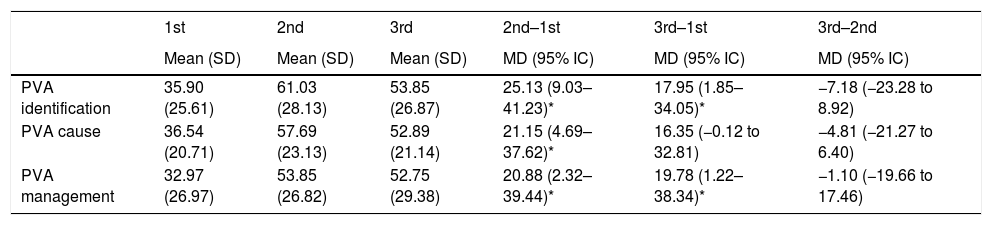
Post hoc analysis showed that there was no difference in participants' performance for any type of question between the assessments at the end of the training program and at the one-month follow-up (column "3rd–2nd" in Table 1). For questions related to establishing the potential cause of PAV, there was no difference between the assessments at the one-month follow-up and the baseline (column "3rd–1st" in Table 1).
Percentage of correct answers by type of question and mean differences between the three evaluation moments.
| 1st | 2nd | 3rd | 2nd–1st | 3rd–1st | 3rd–2nd | |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | MD (95% IC) | MD (95% IC) | MD (95% IC) | |
| PVA identification | 35.90 (25.61) | 61.03 (28.13) | 53.85 (26.87) | 25.13 (9.03–41.23)* | 17.95 (1.85–34.05)* | −7.18 (−23.28 to 8.92) |
| PVA cause | 36.54 (20.71) | 57.69 (23.13) | 52.89 (21.14) | 21.15 (4.69–37.62)* | 16.35 (−0.12 to 32.81) | −4.81 (−21.27 to 6.40) |
| PVA management | 32.97 (26.97) | 53.85 (26.82) | 52.75 (29.38) | 20.88 (2.32–39.44)* | 19.78 (1.22–38.34)* | −1.10 (−19.66 to 17.46) |
1st: baseline; 2nd: End of the training program; 3rd: 1-month follow-up.; 2nd–1st: difference between the first and second evaluation; 3rd–1st: difference between the first and third evaluation; 3rd–2nd: difference between the second and third evaluation; SD: standard deviation; MD: mean difference.
As mentioned above, PVA detection is a challenging task that requires specific training. In a recent study, an interesting alternative to improve PVA detection was proposed. Nurses and non-medical practitioners were trained to establish if there were PVA or not by using pressure and flow time waveforms along with a pressure-flow loop. The results showed that the non-medical subjects performed similarly to the experienced nurses for both the waveform-based and pressure/flow loops. Also, the sensitivities of the overall group improved after switching from the waveform-based classification to the Pressure-flow approach.7
Although some studies have shown the importance of a training program on proper PVA recognition and management,4,5,6,7 this is the first report that has shown the effect of a 6-hour, online, training program on the ability to identify and manage PVA, but also to determine the potential causes of PVA.
Understanding the potential causes of PVAs constitutes, also, a key factor in properly identifying and managing them. This is a crucial point because there are some PVA like double-triggering that might have different causes for example high respiratory drive, larger neural inspiratory time compared to the inspiratory time set on the MV, reverse triggering, and auto triggering.5 Furthermore, establishing the cause of PVA requires specific knowledge about the clinical and pharmacological context along with understanding the feedback obtained by monitorization from different devices.1,8
In this pilot study, we have shown that an online training program on PVA is feasible and is associated with better HCPs performance in the identification, management, and determination of potential causes of PVA. Although, the study has limitations such as the low number of HCPs and the short timeline between the second and the third assessment, these results represent the starting point for a larger study, which will continue to be conducted in the upcoming months. Whether specific training programs on PVA may impact patient-center outcomes requires further investigation.
Funding sourcesThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors declare that they have no conflict of interest.
We thank to the members of the International Asynchrony Group: Francisco A Salinas Barahona (Instituto Nacional del Tórax, Chile), Juan Martín Núñez Silveira (Hospital Italiano, Argentina), Angelo Roncalli M Rocha (Universidade Estadual de Ciências da Saúde, Maceió, Brazil) for helping with the promotion of the pilot study among their hospitals.