To assess the repercussion of the timing of admission to the ICU upon patient prognosis.
DesignA prospective, observational, non-interventional cohort study was carried out.
ScopeA second level hospital with 210 operational beds and a general ICU with 8 operational beds.
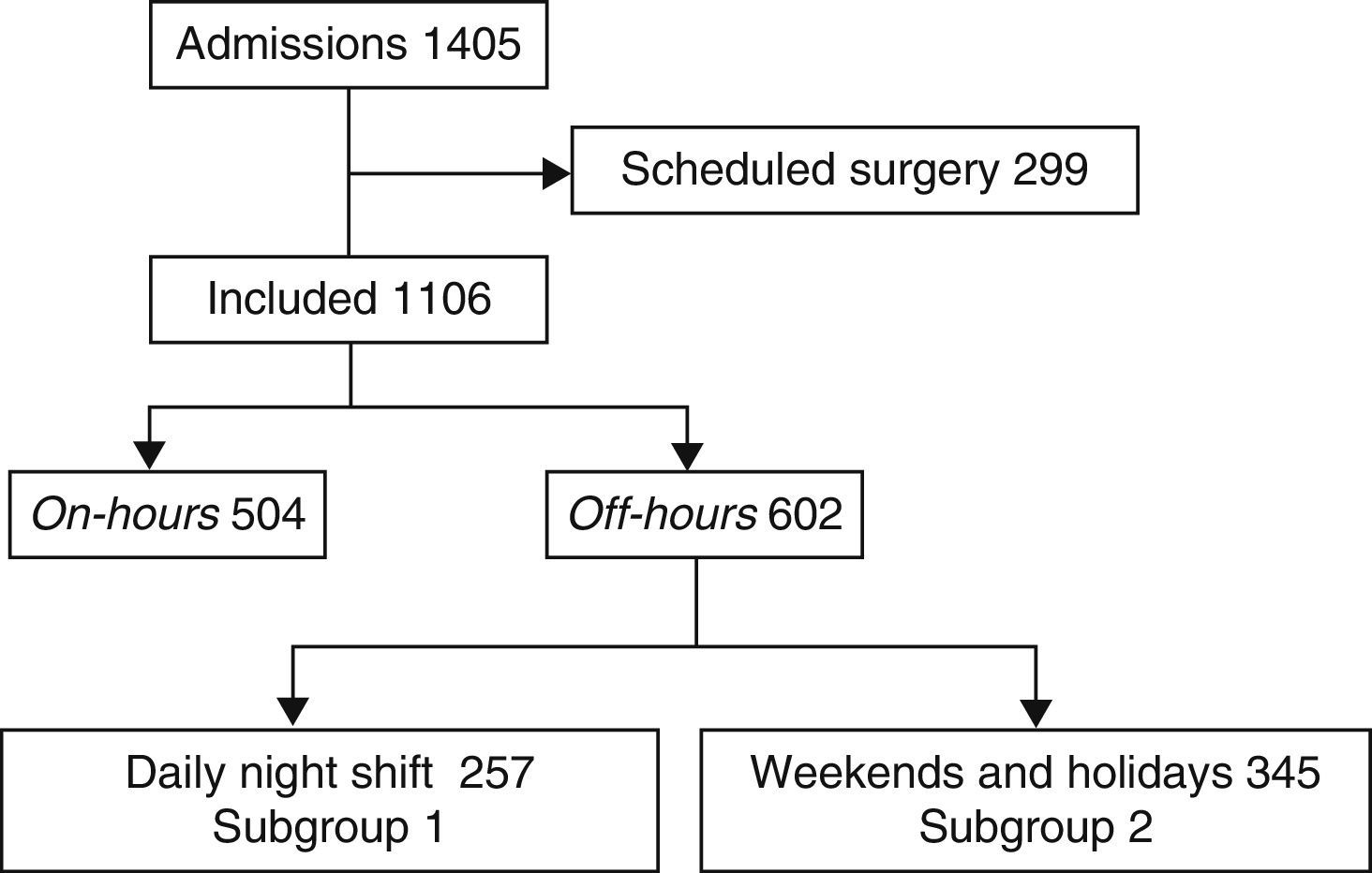
Patients or participantsThe study comprised all patients admitted to the ICU during 3 years (January 2010 to December 2012), excluding those subjects admitted from the operating room after scheduled surgery. The patients were divided into 2 groups according to the timing of admission (on-hours or off-hours).
InterventionsNon-interventional study.
Variables of interestAn analysis was made of demographic variables (age, sex), origin (emergency room, hospital ward, operating room), comorbidities and SAPS 3 as severity score upon admission, length of stay in the ICU and hospital ward, and ICU and hospital mortality.
ResultsA total of 504 patients were included in the on-hours group, versus 602 in the off-hours group. Multivariate analysis showed the factors independently associated to hospital mortality to be SAPS 3 (OR 1.10; 95%CI 1.08–1.12), and off-hours admission (OR 2.00; 95%CI 1.20–3.33). In a subgroup analysis of the off-hours group, the admission of patients on weekends or non-working days compared to daily night shifts was found to be independently associated to hospital mortality (OR 2.30; 95%CI 1.23–4.30).
ConclusionsAdmission to the ICU in off-hours is independently associated to patient mortality, which is also higher in patients admitted on weekends and non-working days compared to the daily night shifts.
Evaluar la repercusión del momento de ingreso en UCI sobre el pronóstico de los pacientes.
DiseñoEstudio de cohorte prospectivo, observacional y no intervencionista. Se consideró on-hours el turno de mañana y tarde de los días laborables y off-hours el resto de los turnos.
ÁmbitoHospital de nivel 2 con 210 camas en funcionamiento y UCI polivalente con 8 camas.
Pacientes o participantesTodos los pacientes que ingresaron en la UCI durante 3 años, de enero de 2010 a diciembre de 2012, excluyendo aquellos pacientes procedentes de quirófano tras una cirugía programada. Los pacientes se estratificaron en 2 grupos en función de que el momento de ingreso fuera on-hours u off-hours.
IntervencionesEstudio no intervencionista.
Variables de interésSe analizaron las variables demográficas (edad, sexo), la procedencia (urgencias, planta de hospitalización, quirófano), el tipo de paciente (médico, quirúrgico), las comorbilidades y el SAPS 3 como puntuación de gravedad al ingreso, estancia en UCI y hospitalaria, además de mortalidad en la UCI y en el hospital.
ResultadosSe incluyeron 504 pacientes en el grupo on-hours y 602 en el grupo off-hours. En el análisis multivariable los factores asociados de forma independiente con la mortalidad hospitalaria fueron SAPS 3 (OR 1,10; IC 95% 1,08-1,12) y grupo off-hours (OR 2,00; IC 95% 1,20-3,33). En un análisis de subgrupos del grupo off-hours el ingreso de los pacientes en fin de semana o festivo frente a las noches de los días de diario se asoció de forma independiente con la mortalidad hospitalaria (OR 2,30; IC 95% 1,23-4,30).
ConclusionesIngresar en el grupo off-hours se asocia de forma independiente con la mortalidad. El ingreso en festivo se asocia de forma independiente con la mortalidad, independientemente del turno en que se produzca el ingreso los días de diario.
In general, the organization of hospital activity in our setting is based on work shifts. In this regard, the morning and afternoon shifts concentrate most of the medical team and scheduled activities, while the night shift, weekends and holidays are fundamentally attended by teams on duty. In some cases, the way in which hospital activities are organized can lead to changes in the prognosis of some patients, particularly those in critical condition.1–3
A number of hypothesis have been proposed to explain the differences in prognosis conditioned to the timing or circumstances of patient admission. One possible explanation is that a poorer prognosis may result from a lower personnel/patient ratio, less experienced specialists, intensivists on call and not physically present in the Unit, or even tiredness of the medical team in certain work shifts.4–6 Other hypotheses point to possibly greater severity among patients who are admitted during the night or on weekends.7 A relationship has also been described between a poorer prognosis and patient admission during the morning clinical round,8,9 though this has not been confirmed in the study published by Bisbal et al.10
The working hypothesis in this study is that there is a difference in mortality among patients admitted to the Intensive Care Unit (ICU) depending on the time of day at which admission takes place.
Specifically, the present study evaluates the repercussions of the timing of admission to the ICU upon patient prognosis in an ICU based on the “ICU without walls” model11–13 of proactive early detection of patients at risk in hospital but outside the ICU.
Material and methodsA prospective, non-interventional observational cohort study was carried out, involving patients consecutively admitted to an adult polyvalent medical-surgical ICU with 8 beds in a 210-bed second-level hospital.
We included all the patients admitted to the Unit in the course of a three-year period from January 2010 to December 2012, excluding those subjects coming from the operating room after scheduled surgery. In the case of patients readmitted to the ICU, we only considered the first admission.
The activity of the intensivists during the study period was distributed as follows:
- 1.
Daily morning shift: from 8 a.m. to 3 p.m., with the presence of the entire Unit personnel members (except those coming off duty and those who worked during the afternoon shift of the previous day). The “ICU without walls” activities are conducted during this shift.
- 2.
Daily afternoon shift: from 3 p.m. to 10 p.m., with the presence of two intensivists.
- 3.
Night shift, from 10 p.m. to 8 a.m., weekends (Saturdays and Sundays) and holidays, with the presence of a single intensivist on duty, along with the usual personnel on duty in the rest of the hospital.
To the effects of analysis, the patients were distributed into two groups:
- 1.
A first group, referred to as on-hours, involving the patients admitted during the daily morning and afternoon shifts (shifts 1 and 2).
- 2.
A second group, referred to as off-hours, involving the patients admitted during the night shift, weekends and holidays (shift 3).
An analysis was made of demographic parameters (age, gender), patient origin (emergency care, hospital admission ward, operating room), patient type (medical, surgical), comorbidities (defined as those comorbidities reflected in the case history, with current or previous treatment for the chronic disorder involved), the SAPS (Simplified Acute Physiology Score) 3 as a measure of severity upon admission, stay in the ICU and in hospital, and in-ICU and in-hospital mortality.
The operation of our ICU incorporates the “ICU without walls” model, which involves the proactive early detection of patients at risk in the hospital, with intervention of the intensivists outside the ICU.11–13 Our secondary objective was to determine whether this model is able to influence the results obtained. With this in mind, we designed a post hoc analysis, differentiating between two subgroups within the off-hours patient group. The subgroups were distinguished on the basis of the “ICU without walls” activities, which only take place in subgroup 1, and not in subgroup 2. However, in both subgroups the general personnel working in the hospital was the same, and lower in number than in the on-hours group:
- 1.
Subgroup 1: patients admitted during the daily night shift
- 2.
Subgroup 2: patients admitted on weekends and holidays
The data are reported as percentages or as the median and interquartile range. In the case of continuous variables we used the Kolmogorov–Smirnov test to determine the presence or absence of a normal distribution. Univariate analysis of continuous and categorical variables was made using the Mann–Whitney U-test and the chi-squared test, respectively. A stepwise multivariate logistic regression analysis was subsequently made, including all the variables evaluated in the univariate analysis. A cutoff point of 0.1 was used in the model, with p=0.10 for exclusion from the model, and an alpha-error of 5%.
In order to avoid possible statistical confounding factors, we performed a multivariate analysis including all the studied variables, stratifying according to the different work shifts (morning, afternoon and night) and holiday or daily shifts. In this regard, we followed the same stepwise multivariate logistic regression model, with exploration of the possible iterations.
The study was approved by the local Ethics Committee, and patient informed consent was not required, in view of the non-interventional nature of the study and the retrospective analysis of the results.
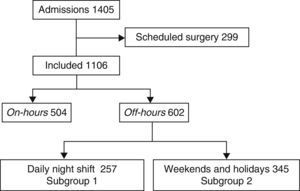
ResultsA total of 1405 patients were admitted to the ICU during the study period. Of these, 299 patients admitted on a scheduled basis due to high-risk surgery were excluded. A total of 504 patients were included in the on-hours group and 602 in the off-hours group (Fig. 1).
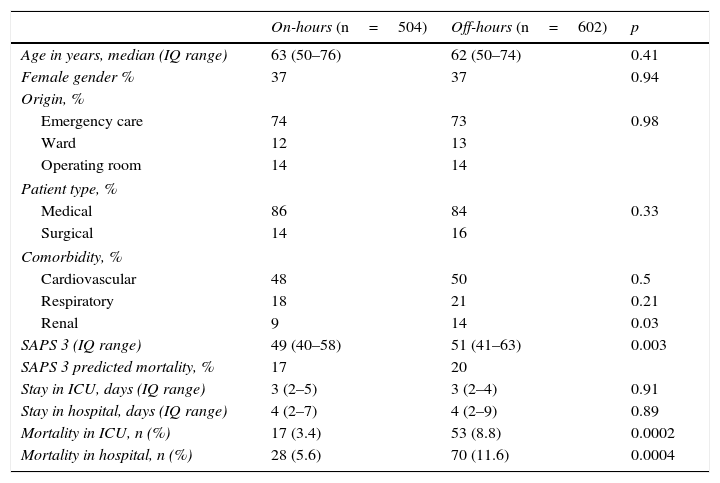
No significant differences were observed in terms of patient age, gender or origin, patient type or mean stay in either the ICU or in hospital after discharge from the Unit. However, the patients in the off-hours group had a greater severity score as measured with the SAPS 3, and a greater presence of renal comorbidity. With regard to the distribution of the patients according to the disease process leading to admission, we recorded no significant differences between medical versus surgical patients, or in terms of the medical disorder on contrasting coronary disease versus other medical disorders (p=0.29). The mortality rate in the ICU was significantly higher in the off-hours group than in the on-hours group, and this difference persisted on analyzing in-hospital mortality. In both groups the in-hospital mortality rate was lower than expected from the predicted mortality rate calculated by the SAPS 3 (Table 1).
Results of the on-hours group versus the off-hours group.
| On-hours (n=504) | Off-hours (n=602) | p | |
|---|---|---|---|
| Age in years, median (IQ range) | 63 (50–76) | 62 (50–74) | 0.41 |
| Female gender % | 37 | 37 | 0.94 |
| Origin, % | |||
| Emergency care | 74 | 73 | 0.98 |
| Ward | 12 | 13 | |
| Operating room | 14 | 14 | |
| Patient type, % | |||
| Medical | 86 | 84 | 0.33 |
| Surgical | 14 | 16 | |
| Comorbidity, % | |||
| Cardiovascular | 48 | 50 | 0.5 |
| Respiratory | 18 | 21 | 0.21 |
| Renal | 9 | 14 | 0.03 |
| SAPS 3 (IQ range) | 49 (40–58) | 51 (41–63) | 0.003 |
| SAPS 3 predicted mortality, % | 17 | 20 | |
| Stay in ICU, days (IQ range) | 3 (2–5) | 3 (2–4) | 0.91 |
| Stay in hospital, days (IQ range) | 4 (2–7) | 4 (2–9) | 0.89 |
| Mortality in ICU, n (%) | 17 (3.4) | 53 (8.8) | 0.0002 |
| Mortality in hospital, n (%) | 28 (5.6) | 70 (11.6) | 0.0004 |
IQ: interquartile; SAPS 3: Simplified Acute Physiology Score; ICU: Intensive Care Unit.
In the multivariate analysis referred to hospital mortality, the risk factors found to be independently associated to mortality were the SAPS 3 (OR 1.10; 95%CI 1.08–1.12; p<0.01) and belonging to the off-hours group (OR 2.00; 95%CI 1.20–3.33; p<0.01).
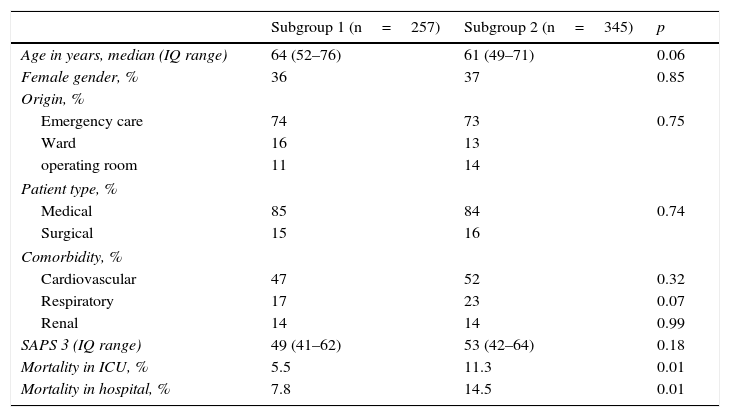
The post hoc analysis of the off-hours subgroups yielded the following results:
The patients included in subgroup 1 (n=257) and in subgroup 2 (n=345) (Fig. 1) showed no differences in terms of age, gender, origin, patient type or SAPS 3. However, mortality in the ICU was higher in those admitted to subgroup 2 than in those admitted to subgroup 1. This same difference was observed on considering in-hospital mortality (Table 2). In the multivariate analysis, the variables found to be independently associated to in-hospital mortality were the SAPS 3 (OR 1.09; 95%CI 1.07–1.11; p<0.01) and belonging to subgroup 2 (OR 2.30; 95%CI 1.23–4.30; p<0.01).
Results of subgroup 1 (daily night shift) versus subgroup 2 (weekends and holidays).
| Subgroup 1 (n=257) | Subgroup 2 (n=345) | p | |
|---|---|---|---|
| Age in years, median (IQ range) | 64 (52–76) | 61 (49–71) | 0.06 |
| Female gender, % | 36 | 37 | 0.85 |
| Origin, % | |||
| Emergency care | 74 | 73 | 0.75 |
| Ward | 16 | 13 | |
| operating room | 11 | 14 | |
| Patient type, % | |||
| Medical | 85 | 84 | 0.74 |
| Surgical | 15 | 16 | |
| Comorbidity, % | |||
| Cardiovascular | 47 | 52 | 0.32 |
| Respiratory | 17 | 23 | 0.07 |
| Renal | 14 | 14 | 0.99 |
| SAPS 3 (IQ range) | 49 (41–62) | 53 (42–64) | 0.18 |
| Mortality in ICU, % | 5.5 | 11.3 | 0.01 |
| Mortality in hospital, % | 7.8 | 14.5 | 0.01 |
IQ: interquartile; SAPS 3: Simplified Acute Physiology Score; ICU: Intensive Care Unit.
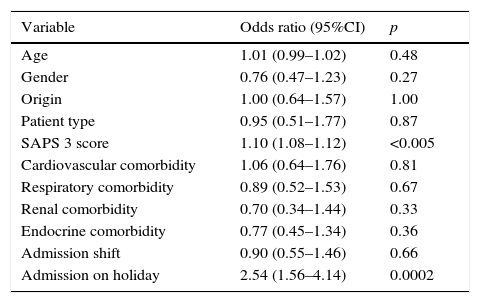
On analyzing all the variables, the only two factors associated to in-hospital mortality were the SAPS 3 (OR 1.10; 95%CI 1.08–1.12) and admission on a holiday (OR 2.54; 95%CI 1.56–4.14). The full results of the multivariate analysis are reported in Table 3.
Results of the multivariate analysis.
| Variable | Odds ratio (95%CI) | p |
|---|---|---|
| Age | 1.01 (0.99–1.02) | 0.48 |
| Gender | 0.76 (0.47–1.23) | 0.27 |
| Origin | 1.00 (0.64–1.57) | 1.00 |
| Patient type | 0.95 (0.51–1.77) | 0.87 |
| SAPS 3 score | 1.10 (1.08–1.12) | <0.005 |
| Cardiovascular comorbidity | 1.06 (0.64–1.76) | 0.81 |
| Respiratory comorbidity | 0.89 (0.52–1.53) | 0.67 |
| Renal comorbidity | 0.70 (0.34–1.44) | 0.33 |
| Endocrine comorbidity | 0.77 (0.45–1.34) | 0.36 |
| Admission shift | 0.90 (0.55–1.46) | 0.66 |
| Admission on holiday | 2.54 (1.56–4.14) | 0.0002 |
95%CI: 95% confidence interval; SAPS 3: Simplified Acute Physiology Score.
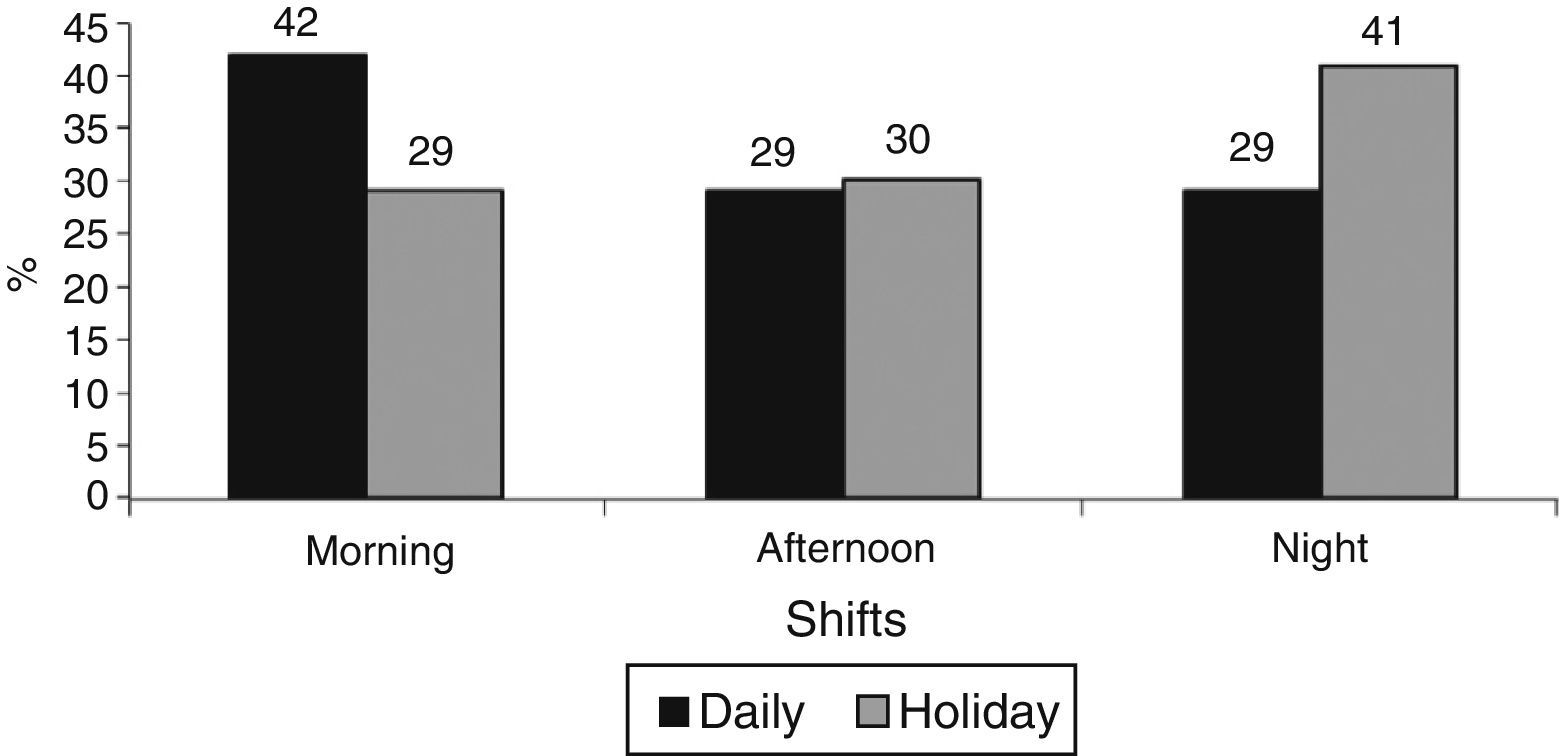
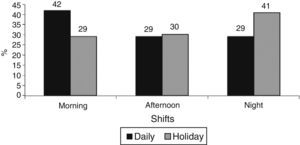
On the other hand, a significant difference was observed on analyzing the timing of admissions histogram, with a greater percentage of admissions during the daily morning shifts (scheduled surgery patients were excluded) versus a greater percentage of admissions during the night shift on weekends and holidays (Fig. 2).
DiscussionAlthough our study showed survival in both groups to be greater than predicted by the severity indicators employed, the patients who were admitted to the ICU in the course of the daily shifts showed a better prognosis than those admitted on weekends or holidays.
Our results coincide with those of earlier studies that analyzed the timing of admission and the prognosis of patients admitted to the ICU. Bhonagiri et al.1 recorded a lower in-ICU mortality rate in the 6 p.m. to 5:59 a.m. interval than in the 6 a.m. to 5:59 p.m. period (9.1% versus 10.8%; p<0.001), and Kuijsten et al.2 observed a greater mortality risk on weekends than during the daily shifts. However, although Ju et al.14 described a difference in mortality between the night shift and the day shift (OR 1.72; 95%CI 1.118–2.74), no such difference was recorded on comparing weekends versus daily shifts. Nwosu et al.15 in turn reported a difference in mortality in patients admitted to the ICU on weekends versus daily shifts, though statistical significance was not reached. Laupland et al.16 likewise recorded no differences regarding in-hospital mortality among patients admitted to the ICU at night or on Saturdays or Sundays versus the daily shifts of the working week. The metaanalysis conducted by Cavallazzi et al.17 found an association referred to admission to the ICU on weekends, but not to admission at night.
Differences in results are also found in other settings. Freemantle et al. observed greater in-hospital mortality when the patients were admitted to hospital on weekends than on the working week days3 also in patients with acute coronary syndrome and ST-segment elevation,18 patients undergoing elective surgery,19 and patients admitted to the emergency room20–though no association could be demonstrated between the timing of admission and mortality as in the study published by Fonarow et al.21 in patients admitted due to heart failure, or by Carr et al.22 in trauma patients.
A number of hypotheses have been proposed to explain these differences in mortality, based fundamentally on differences in the organization of the work shifts, with or without the presence of intensivists, or based on the experience of the intensivist on duty (resident in training versus staff physician), in units assisting seriously ill patients upon admission. A metaanalysis carried out by Wilcox et al.5 showed a significant difference on comparing high intensity staffing, where the patient is moved to an ICU supervised by an intensivist, versus low intensity staffing, where no intensivist is present–with greater in-ICU survival in the high intensity staffing group (RR 0.81; 95%CI 0.68–0.96). However, on examining the 24-h intensivist model versus intensivist coverage only during the day shift, no decrease in mortality was found (RR 0.88; 95%CI 0.7–1.1). Another hypothesis is based on patient severity upon admission, which is greater in patients admitted at night, as in the study published by Ju et al.,14 where a high APACHE II score (>8) versus a low APACHE II score (<8) was found to be an independent predictor of mortality (OR 1.113; p<0.001).
In our study, the patients admitted off-hours had greater severity upon admission as determined by the SAPS 3, with less medical personnel available for care (a single intensivist on duty). This is consistent with the abovementioned hypotheses.
One element that distinguishes us from other units is our “ICU without walls” activity, based on the early detection of patients at risk in the hospital, outside the ICU, and which allows us to intervene before organ failure occurs. In a before-after study published by our group,11 we demonstrated benefit in terms of clinical outcome among the intervened patients, with a better management of the available healthcare resources, and a decrease in mortality in the ICU among the patients admitted during the period in which the project was implemented (OR 0.42; 95%CI 0.18–0.98; p=0.04).
For this reason, our secondary objective in this study was to determine whether an increased probability of a favorable prognosis could be due to the earlier identification of patient severity and earlier admission to the ICU. In order to identify a possible relationship between the “ICU without walls” activity and the outcomes, we compared the two subgroups within the off-hours group: subgroup 1 (daily night shifts) and subgroup 2 (weekends and holidays), where in both instances only the intensivist on duty is present–the sole difference between the two subgroups being the “ICU without walls” activity during the daily morning shifts but not on weekends or holidays. We found that for the same patient severity as evaluated by the SAPS 3, the in-ICU mortality rate was significantly higher in the patients belonging to subgroup 2. Likewise, the multivariate analysis showed the variables independently associated to in-hospital mortality to be the SAPS 3 and belonging to subgroup 2.
These results support the idea that the early detection of potentially critical patients and their consequent improved survival rates11,23–26 could (among other factors) influence the lesser mortality found in subgroup 1 versus subgroup 2, since there is no “ICU without walls” activity on weekends and holidays–the patients in the latter case being admitted later, and therefore with a poorer prognosis. This circumstance is reflected by the timing of admissions histogram, where a greater percentage of admissions in observed in the course of the daily morning shifts (scheduled surgery patients being excluded) versus a greater percentage of admissions during the night shifts on weekends and holidays (Fig. 2).
The present study has the limitations inherent to its single-center nature. On the other hand, its non-interventional design does not allow us to confirm the hypothesis referred to our secondary objective. In this regard, we can only support the possibility of a relationship between the “ICU without walls” activity (among other factors) and lesser mortality in the analyzed subgroups. Likewise, we are unable to determine whether there is a real difference in the time between the detection of patient severity and admission to the ICU. However, our observations could support the hypothesis that extending the “ICU without walls” system to the weekends could result in improved patient outcomes.
Another limitation has been the use of the SAPS 3 as a patient severity indicator upon admission to the ICU, since in patients with few failed organs the SAPS 3 overestimates predicted mortality–this possibly explaining the great difference between predicted and actual hospital mortality.27
ConclusionsAdmission to the off-hours group is independently associated to mortality. Admission on weekends is likewise independently associated to mortality, regardless of the daily shift involved.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Thanks are due to Dr. Alvaro Castellanos for his help in preparing the manuscript.
Please cite this article as: Abella A, Hermosa C, Enciso V, Torrejón I, Molina R, Salinas I, et al. Efecto del momento de ingreso sobre el pronóstico de los pacientes en la Unidad de Cuidados Intensivos: on-hours vs. off-hours. Med Intensiva. 2016;40:26–32.