Transthoracic echocardiography can significantly change the management of many critical patients, and is being incorporated into many Intensive Care Units (ICU). Very few studies have examined the feasibility and impact of intensivists performing basic transthoracic echocardiography upon the management of critical patients after cardiac surgery. The present study therefore evaluates the quality of acquisition and accuracy of intensivist interpretation of basic transthoracic echocardiograms in the postoperative period of heart surgery.
MethodsOver an 8-month period we prospectively studied 148 patients within 24h after admission to a university hospital ICU following heart surgery. We performed basic transthoracic echocardiography to evaluate ventricular function, pericardial effusion, hypovolemia and mitral regurgitation. Cohen's Kappa was used to compare transthoracic echocardiograms obtained by intensivists with basic versus advanced training. Concordance on image acquisition and interpretation was evaluated.
ResultsWe analyzed data of adequate transthoracic echocardiograms in 148 patients (92.5%). Apical four-chamber view and advanced trainees obtained better quality images. Concordance was good for right and left ventricular function (kappa=0.7±0.14 and 0.87±0.05, respectively), and moderate for the remaining parameters. Interpretation concordance between basic and advanced training intensivists was good (kappa=0.73±0.05).
ConclusionsIntensivists with basic training in echocardiography are capable of performing and interpreting echocardiograms in most patients during the postoperative period of heart surgery.
La ecocardiografía transtorácica puede cambiar significativamente el manejo en muchos pacientes críticos y se está incorporando dentro de muchas unidades de cuidados intensivos (UCI). Pocos estudios han examinado la factibilidad y el impacto de la ecocardiografía transtorácica básica realizada por intensivistas en el manejo de los pacientes críticos después de una cirugía cardíaca. Por ello, nosotros evaluamos la calidad de adquisición y la precisión en la interpretación de la ecocardiografía básica realizada por intensivistas en los pacientes postoperados de cirugía cardíaca.
MétodosDurante 8 meses, estudiamos prospectivamente 148 pacientes postoperados de cirugía cardíaca dentro de las primeras 24h de ingreso en una UCI de un hospital universitario. Realizamos una ecocardiografía transtorácica básica para evaluar función ventricular, líquido pericárdico, hipovolemia y regurgitación mitral. Utilizamos el coeficiente kappa de Cohen para comparar las ecocardiografías transtorácicas realizadas por los intensivistas con formación básica versus avanzada. Evaluamos la concordancia en la adquisición de imágenes y su interpretación.
ResultadosAnalizamos los datos de las ecocardiografías transtorácicas de 148 pacientes (92,5%). La visión apical cuatro-cámaras y los intensivistas con formación avanzada obtuvieron mayor calidad de imagen. La concordancia fue buena para la función ventricular derecha e izquierda (kappa=0,7±0,14 y 0,87±0,05, respectivamente), y moderada para el resto de parámetros. La concordancia de la interpretación entre los intensivistas con formación básica y avanzada fue buena (kappa=0,73±0,05).
ConclusionesLos intensivistas formados en ecocardiografía transtorácica básica son capaces de obtener e interpretar las ecocardiografías en la mayoría de postoperados programados de cirugía cardíaca.
Since more than 25 years, the usefulness of transthoracic echocardiography in the evaluation of critical patients has been established. This noninvasive imaging technique uses real-time dynamic images of the heart to provide morphologic and functional information that can identify the causes of shock, may help to predict the response to fluid replacement therapy, and to guide treatment. Echocardiography can significantly change the management in up to 46% of critical patients, and some groups have developed protocols to optimize the use of transthoracic echocardiography in critical care.1–12 Intensivists are recommended to learn echocardiography, and training in this technique is being incorporated into residency training programs.9,12–20
Various scientific societies are developing guidelines for basic training in echocardiography for physicians other than cardiologists, based on existing consensus.6,12,21 The aim is to expand the use of this tool by teaching physicians to recognize specific parameters that can be useful in clinical practice. In critical care, two levels of competency have been defined: basic and advanced. Basic training includes positioning the transducer to obtain images in the standard echocardiography planes (parasternal for long- and short-axis views, apical for four-chamber view, and subcostal for four-chamber view and visualization of the inferior vena cava). After basic training, physicians should be able to use echocardiography to diagnose severe hypovolemia, left ventricular failure, right ventricular failure, cardiac tamponade, acute massive mitral regurgitation, and the causes of cardiac arrest as well as to determine whether resuscitation has restored normal heart rhythm.22–27
Many studies have shown that it is useful for physicians other than cardiologists to correctly interpret echocardiograms.6,13,15,21,28–38 Although some studies have evaluated the usefulness of intensivists performing transesophageal echocardiography in critical patients,39–42 few studies have evaluated the feasibility and impact of basic transthoracic echocardiography by intensivists in the management of critically ill patients and after cardiac surgery.34,43–45
Transthoracic echocardiographies in intensive care unit are goal-directed. The objectives of transthoracic echocardiographies after cardiac surgery are the diagnosis of postoperative complications and the evaluation of cardiac function. The major difficulties of transthoracic echocardiography after cardiac surgery are due to the presence of chest drains, mechanical ventilation, postoperative inflammation and pain with mobilizations. This study aimed to evaluate the feasibility of basic transthoracic echocardiography in postoperative cardiac patients to analyze the quality and accuracy of acquisition by intensivists.
Patients and methodsThe study was done in a 17-bed mixed medical/surgical intensive care unit (ICU) in a general university hospital with approximately 300 ICU admissions/year of cardiac surgery. Our institutional Clinical Research Ethics Committee approved the study protocol, and all participating patients provided written informed consent. We included all adult patients admitted to the ICU after cardiac surgery between November 2013 and July 2014 and a basic and an advanced echocardiography were performed. Intensivists underwent training in basic echocardiography from November 2012 through April 2013, consisting of a teaching program of 10h and performing at least 30 basic transthoracic echocardiograms under the supervision of an expert. Knowledgement and skills were assessed by written and practical examination according to the recommendations of guidelines.6,13,21,28Annex A (supplementary material) describes the teaching program and examinations in detail.6,12,13,21,28
Data collectionWe recorded general demographic information; reason for ICU admission; comorbidities; severity indices (APACHE II, EuroSCORE); presurgical hemodynamic parameters and echocardiographic findings, when available. Mechanical ventilation parameters, use of vasoactive drugs and hemodynamic parameters were determined before the echocardiothoracic examination.
Within 24h of admission, all patients underwent two independent consecutive basic transthoracic echocardiographies by a basic and advanced echocardiography trained intensivist that were interpreted separately. Four senior intensivists with basic training and two senior intensivists with advanced training (level 3 of competence in echocardiography with minimum 5 years of experience)28,46 (AO and OM) participated in the study. All echocardiograms were done using a cardiovascular ultrasound system (Vivid e, GE Healthcare, Chicago, IL, USA) with a 1.5MHz–4.6MHz transducer (M5S-D, GE Healthcare, Chicago, IL, USA).
The basic echocardiography examination included the systematic evaluation of cardiac structure and function in the parasternal long- and short-axis views, apical four-chamber view, and subcostal four-chamber and inferior vena cava views. Intensivists graded the subjective difficulty of image acquisition in each acoustic window as “high” or “low”.
The following parameters were recorded in each examination:
- (1)
Left ventricle: visual size, classified as “normal” or “dilated”; visual systolic function, classified as “normal” (≥50%) or “depressed” (<50%); and contraction pattern, classified as “homogeneous” or “heterogeneous”.
- (2)
Right ventricle: visual size, classified as “normal” or “dilated” and visual systolic function, classified as “normal” or “depressed”.
- (3)
Valves: massive mitral regurgitation, classified as “present” or “absent”.
- (4)
Inferior vena cava: classified as “normal”, “dilated”, or “not visualized”.
- (5)
Pericardial effusion with or without cardiac tamponade, classified as “present” or “absent”.
With echocardiographic findings, we could obtain different echocardiographic patterns, that are exposed in Annex B (supplementary material).
All examinations, performed by basic and advanced trained intensivists, were digitally recorded and later assessed by an intensivist with advanced training in transthoracic echocardiography, who graded image quality as “optimal” (complete identification of the endocardial borders of the left ventricle), “suboptimal” (identification of >50% of the endocardial borders of the left ventricle), or “poor” (identification of <50% of the endocardial borders of the left ventricle). Images graded “optimal” or “suboptimal” enabled a diagnosis to be reached.
We compared the echocardiographic findings and their interpretation between basic and advanced trained intensivists. The interpretation of intensivists with advanced training was considered the gold standard.
Statistical analysisContinuous variables are expressed as means±standard deviations or frequencies and percentages. To determine the degree of concordance between the interpretation of basic and advanced trained intensivists, we used Cohen's kappa coefficient with 95% confidence intervals.
We estimated that to distinguish between a kappa coefficient of 0.8 (near perfect concordance) and a kappa coefficient of 0.4 (poor concordance) with two-tailed test with a power of 90% and assuming 90% positive values, we would need to include at least 136 patients. We considered kappa ≤0=poor concordance; kappa 0.01–0.2=slight concordance; kappa 0.21–0.4=minimum acceptable concordance; kappa 0.41–0.6=moderate concordance; kappa 0.61–0.8=good concordance; kappa 0.81–1: nearly perfect concordance.47
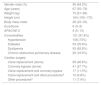
ResultsPatients’ characteristicsA total of 161 patients were admitted to the ICU after cardiac surgery during the study period. One patient refused to participate in the study and 12 of 161 (7.45%) patients were discarded because we could not obtain any image. Finally, we included 148 patients in the study. Table 1 reports the demographic and clinical characteristics and the type of cardiac surgery of the patients included in the study.
Demographic, clinical characteristics and cardiac surgery of patients included in the study (n=148).
| Gender male (%) | 95 (64.2%) |
| Age (years) | 67 (55–79) |
| Weight (kg) | 75 (61–89) |
| Height (cm) | 164 (155–173) |
| Body mass index | 28 (23–33) |
| EuroScore | 6 (3–9) |
| APACHE-II | 9 (5–13) |
| Comorbidities | 121 (81.8%) |
| Hypertension | 108 (73%) |
| Diabetes | 53 (35.8%) |
| Dyslipemia | 93 (62.8%) |
| Chronic obstructive pulmonary disease | 20 (16.5%) |
| Cardiac surgery | |
| Valve replacement (alone) | 69 (46.6%) |
| Coronary bypass (alone) | 41 (27.7%) |
| Valve replacement and coronary bypass | 17 (11.5%) |
| Valve replacement and other proceduresa | 10 (6.8%) |
| Other proceduresa | 11 (7.4%) |
The table express the mean (standard deviation) or frequency (percentage).
All patients underwent preoperative transthoracic echocardiography by a cardiologist. Seventy-eight patients (52.7%) had a hypertrophic left ventricle without dilation and 129 patients (87.2%) had a normal ejection fraction. One hundred forty-three patients (96.6%) had normal right ventricle size and function, and 139 patients (93.9%) had a non-dilated inferior vena cava with collapse >50%.
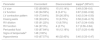
Postoperative transthoracic echocardiographyClinical characteristics at the time of the postoperative transthoracic echocardiography are described in Table 2.
Postoperative characteristics and hemodynamic state in the moment of the echocardiographies.
| Heart rhythm (patients (%)) | |
| Sinus rhythm | 123 (83.1%) |
| Atrial fibrillation | 8 (5.4%) |
| Nodal Rhythm | 2 (1.4%) |
| Complete atrioventricular block | 1 (0.7%) |
| Pacemaker | 14 (9.6%) |
| Heart rate (bpm) | 80 (68–92) |
| Mean arterial pressure (mmHg) | 79 (69–89) |
| Central venous pressure (mmHg) | 9 (5–13) |
| Central venous saturation (%) | 67 (58–76) |
| Lactate (mg/dL) | 17 (6–28) |
| Mechanical ventilation | 25 (16.9%) |
| Volume-controlled | 17 (68%) |
| Pressure support | 8 (32%) |
| Vasoactive drugs | 86 (58.1%) |
| Noradrenaline | 50 (33.8%) |
| Nitroglycerine | 27 (18.2%) |
| Dopamine | 10 (6.8%) |
| Dobutamine | 10 (6.8%) |
| Levosimendan | 5 (3.4%) |
| Pulmonary artery catheter | 26 (17.6%) |
The table expresses the mean (standard deviation) or frequency (percentage).
Only two patients required an intra-aortic balloon pump.
Because all patients had chest drains, many had pain on movement, and some were intubated, 136 (91.9%) echocardiograms were done in the supine position; the remaining (12; 8.1%) were done in the left lateral decubitus position. The mean duration of the examination was 16±5min by basic trained intensivists and 15±5min by advanced trained intensivists.
Advanced trained intensivists obtained adequate images in all patients. The best image quality was obtained in the apical four-chamber view and the worst in the subcostal view of the inferior vena cava. Intensivists with advanced training achieved better image quality.
The results of basic and advanced trained intensivists echocardiographies are shown in Table 3. We could see that basic trained intensivists tended to interpret as normal both size and function of both left and right ventricle in those limit values. Also, we could see that basic trained tended to diagnose more hypovolemia than advanced trained intensivists.
Echocardiographic findings.
| Basic trained intensivist | Advanced trained intensivist | |||
|---|---|---|---|---|
| Left Ventricle | Size | Normal | 133 (89.9%) | 130 (87.8%) |
| Dilated | 15 (10.1%) | 18 (12.2%) | ||
| Function | Normal | 109 (73.6%) | 105 (70.9%) | |
| Depressed (<50%) | 39 (26.4%) | 43 (29.1%) | ||
| Right Ventricle | Size | Normal | 135 (91.2%) | 134 (90.5%) |
| Dilated | 13 (8.8%) | 14 (9.5%) | ||
| Function | Normal | 143 (96.6%) | 139 (93.9%) | |
| Depressed | 5 (3.4%) | 9 (6.1%) | ||
| Pericardial fluid | Presence | 16 (10.8%) | 16 (10.8%) | |
| Absence | 132 (89.2%) | 132 (89.2%) | ||
| Tamponade | No | 148 (100%) | 148 (100%) | |
| Hypovolemia | Yes | 16 (10.8%) | 12 (8.1%) | |
| No | 85 (57.4%) | 91 (61.5%) | ||
| Not valorable | 47 (31.8%) | 45 (30.4%) |
The table expresses the number of patients and frequency (percentage).
The concordances of echocardiography findings by the two observers (basic and advanced) are shown in Table 4. A good concordance was observed in the evaluation of right and left ventricular function (kappa 0.7; 0.56–0.84 and kappa 0.87; 0.82–0.92, respectively). The echocardiographical diagnosis interpretation between both observers was concordant in 85.1% of the cases (kappa 0.73; 0.68–0.78). The concordance of diagnosis is shown in Table 5.
Concordance of echocardiography findings between intensivists with basic and advanced training.
| Parameter | Concordant | Disconcordant | kappaa (95%CI) |
|---|---|---|---|
| LV size | 133 (89.86%) | 15 (10.14%) | 0.49 (0.38–0.6) |
| LV function | 140 (94.59%) | 8 (5.41%) | 0.87 (0.82–0.92) |
| LV contraction pattern | 109 (73.64%) | 39 (26.35%) | 0.42 (0.34–0.50) |
| Kissing walls | 138 (93.24%) | 10 (6.75%) | 0.58 (0.46–0.70) |
| RV dilation | 135 (91.22%) | 13 (8.78%) | 0.47 (0.34–0.60) |
| RV function | 144 (97.3%) | 4 (2.7%) | 0.7 (0.56–0.84) |
| Pericardial fluid | 130 (87.84%) | 18 (12.16%) | 0.37 (0.25–0.49) |
| Signs of tamponadea | 148 (100%) | ||
| Hypovolemia | 100 (67.57%) | 48 (32.43%) | 0.40 (0.33–0.47) |
CI=confidence interval; LV=left ventricle; RV=right ventricle.
Concordance of interpretation of echocardiography findings between intensivists with basic and advanced training.
| Diagnosis | n | Concordant | Discordant | kappa (95%CI) |
|---|---|---|---|---|
| Ventricular dysfunction | 46 | 38 (82.6%) | 8 (17.4%) | |
| Hypovolemia | 15 | 11 (73.33%) | 4 (26.67%) | |
| No abnormalities | 87 | 77 (88.51%) | 10 (11.49%) | |
| Total | 148 | 126 (85.14%) | 22 (14.86%) | 0.73 (0.68–0.78) |
CI=confidence interval.
We have performed a subanalysis of ventilated patients and chronic obstructive pulmonary disease (COPD) patients and we have found no differences respect the global concordances.
DiscussionThis study demonstrates that a basic TTE training in intensivists let them to evaluate postoperative cardiac surgical patients with a moderate-good concordance in findings and interpretation within 24h after cardiac surgery. To date, few studies have evaluated the feasibility of transthoracic echocardiography in the postoperative period in patients undergoing cardiac surgery. André et al.,43 included 51 patients and found that echocardiography was possible in 82%. In our study, no images could be obtained in 12 cases (7.5%). Thus, echocardiography provided important information in 148 (92.5%) patients. This difference can be due to the number of patients included in the studies (51 versus 148) and the no availability of the echocardiograph in André case.
Olmos et al.,44 studied the interobserver agreement in the evaluation of right ventricular function in the early postoperative period of cardiac surgery. They demonstrated that they could obtain interpretable images in 92% of patients, that it is similar to our results. The principal differences respect our study are that in their case both explorers were cardiologist with experience in echocardiography and they only analyzed right ventricular function. In our case, both explorers were intensivist with basic or advanced training and we analyzed all parameters.
Vezzani et al.,45 studied the value of chest ultrasound after cardiac surgery in comparison with chest X-ray and auscultation. They demonstrated that with chest ultrasound we can detect some postoperative abnormalities and complications in patients admitted to intensive care after cardiac surgery without needing to perform a chest X-ray. They used chest ultrasound, so they could see pericardial effusion or cardiac tamponade, but they did not performed echocardiography, so they could not see other abnormalities like cardiac disfunction, that it is one of the parameters that we analyzed in our study.
We also sought to determine the degree of concordance in the echocardiography findings and their interpretation between examinations done by intensivists with basic training in the technique and those done by intensivists with advanced training. Other studies in medical critically ill patients analyzed the degree of concordance between both intensivists. They concluded that providing intensivists with basic training in echocardiography was useful for critical care.15,31–35,48,49 However, many of these studies excluded cardiac surgery patients, and no information was available about the feasibility and usefulness of echocardiography by intensivists in this group of patients. Olmos-Temois et al.,44 recently evaluated the interobserver variability in echocardiography parameters of the right ventricle in 52 stable patients without tamponade or active bleeding 6–8h after heart surgery. In our study, we excluded only patients who declined to participate and those without images, and we analyzed all basic echocardiography parameters. Interobserver concordance in our study was moderate. Concordance on left ventricular function, right ventricular function, and the final echocardiographic diagnosis was good or nearly perfect. Our results are a better than in other studies,15,32,33 probably because of patients’ characteristics. We had only analyzed postcardiac surgical patients and they analyzed medical and other than postcardiac surgical patients. It is important to remark that right and left ventricular function are two of the most important parameters in postcardiac surgical patients because of the repercussion of this kind of surgery. Thus, we conclude that intensivists with basic training in echocardiography are capable of correctly carrying out and interpreting basic transthoracic echocardiography examinations in most postcardiac surgical patients.
It is important to demonstrate the feasibility of basic echocardiography in ruling out the most extreme and most severe patterns during postoperative cardiac surgery period (as severe ventricular dysfunction, severe hypovolemia, severe mitral regurgitation, and tamponade). But that this does not obviate the need for advanced echocardiography by duly trained intensivists or cardiologists when necessary.
We have found with some limitations during our study. This is a single center study undergoing scheduled cardiac surgery by the same surgical team, and we cannot extrapolate our results to other centers. No patients undergoing urgent surgery were included and the number of complications was low. Therefore we are unable to confirm a good interobserver concordance in acute postsurgical patients that normally presents a higher number of severe complications.
Some of the basic patterns, in particular hypovolemia, might not be sufficiently validated in populations like ours that have structural disease such as ventricular hyperthrophy, dilation of cardiac chambers, valvular heart disease. Finally, the evaluation of the presence of hypovolemia by basic transthoracic echocardiography in the postoperative cardiac surgery patients needs further studies.
Finally, we did not measure the end-diastolic diameters of the ventricles, and this could make it difficult to identify some cases of ventricular dilation. This short coming could explain the discordance between some examinations done by intensivists with basic and advanced training.
ConclusionsIntensivists with basic training in echocardiography are capable of performing and interpreting echocardiograms in most scheduled postoperative cardiac surgery patients.
Authors’ contributionConception and design: Dr. Olga Moreno, Dr. Ana Ochagavía, Dr. Antonio Artigas, Dr. Francisco Baigorri.
Acquisition, analysis and interpretation: Dr. Olga Moreno, Dr. Ana Ochagavía, Dr. Cristina Espinal, Dr. Roser Tomás, Dr. Maria Dolores Bosque, Dr. Cristina Fortià.
Drafting the manuscript for important intellectual content: Dr. Olga Moreno, Dr. Ana Ochagavía, Dr. Antonio Artigas, Dr. Francisco Baigorri.
Conflict of interestsThe authors have no conflicts of interest.
The authors are grateful to Cristina Mora, Maria Luisa Martinez, Susana Millan and Eva Torrents (Hospital Universitari General de Catalunya) for their contribution in data collect, and David Suárez (Parc Tauli Hospital Universitari) for his contribution in statistical analysis. This paper is part of a Thesis of the Medicine Department of Universidad Autónoma de Barcelona, Barcelona, Spain.