To study the characteristics and outcomes of patients in the ICU with severe community-acquired pneumonia (SCAP) over a 15-year surveillance period.
MethodsWe conducted a retrospective cohort study of episodes of SCAP, and assessed the epidemiology, etiology, treatment and outcomes of patients admitted to the ICU, comparing three periods (1999–2003, 2004–2008 and 2009–2013).
ResultsA total of 458 patients were diagnosed with SCAP. The overall cumulative incidence was 37.4 episodes/1000 admissions, with a progressive increase over the three periods (P<0.001). Patients fulfilling the two major IDSA/ATS criteria at admission increased from 64.2% in the first period to 82.5% in the last period (P=0.005). Streptococcus pneumoniae was the prevalent pathogen. The incidence of bacteremia was 23.1%, and a progressive significant reduction in overall incidence was observed over the three periods (P=0.02). Globally, 91% of the patients received appropriate empiric antibiotic treatment, increasing from 78.3% in the first period to 97.7% in the last period (P<0.001). Combination antibiotic therapy (betalactam+macrolide or fluoroquinolone) increased significantly from the first period (61%) to the last period (81.3%) (P<0.001). Global ICU mortality was 25.1%, and decreased over the three periods (P=0.001).
ConclusionsDespite a progressively higher incidence and severity of SCAP in our ICU, crude ICU mortality decreased by 18%. The increased use of combined antibiotic therapy and the decreasing rates of bacteremia were associated to improved patient prognosis.
Estudiar las características y el pronóstico de los pacientes con neumonía grave adquirida en la comunidad ingresados en una unidad de cuidados intensivos (UCI) durante un período de 15 años.
Material y métodosEstudio retrospectivo de una cohorte de pacientes con neumonía grave comunitaria en los que se analizó la evolución en la epidemiología, etiología, tratamiento y pronóstico durante un período de 15 años, comparando 3 períodos (1999-2003, 2004-2008 y 2009-2013).
ResultadosUn total de 458 pacientes fueron diagnosticados de neumonía. La incidencia media global durante el período estudiado fue de 37,4 episodios/1.000 ingresos, encontrándose un incremento progresivo durante los 3 períodos estudiados (p<0,001). Los pacientes que cumplían con los 2 criterios mayores de neumonía grave de la ATS/IDSA aumentaron de un 64,2% en el primer período a un 82,5% en el último período (p=0,005). Streptococcus pneumoniae fue el microorganismo más frecuente aislado. La incidencia de bacteriemia fue del 23,1%, encontrándose una reducción significativa y progresiva en la incidencia a lo largo de los 3 períodos (p=0,02). El 91% de los pacientes recibió tratamiento antibiótico empírico apropiado, encontrándose un incremento entre el primer y el último período del 78,3% al 97,7% (p<0,001). El tratamiento combinado (betalactámico+macrólido o quinolona) aumentó de un 61% en el primer período a un 81,3% en el último (p<0,001). La mortalidad en la unidad de cuidados intensivos durante todo el período fue del 25,1%, encontrándose una disminución progresiva durante los 3 períodos (p=0,001).
ConclusionesA pesar de un incremento progresivo en la incidencia y gravedad de las neumonías ingresadas en unidad de cuidados intensivos, la mortalidad se redujo en un 18%. El incremento en la utilización de tratamiento combinado y la disminución en la incidencia de bacteriemia se asociaron a una mejoría en el pronóstico.
In the United States, community-acquired pneumonia (CAP) affects >5 million adults and accounts for >1 million hospital admissions each year due to the severity of the disease or decompensation of underlying comorbid disease.1,2 Severe CAP (SCAP) requiring critical care affects 10–22% of these.3,4 Morbidity and mortality in patients remain high, despite advances in critical care management and antimicrobial therapy. Mortality in those admitted in to the intensive care unit (ICU), ranges from 21% to 58%.5–7
Early empiric antimicrobial therapy has proven the most effective approach to decreasing mortality in patients with SCAP. Various organizations, most notably the Infectious Diseases Society of America (IDSA)/American Thoracic Society (ATS)8 and the British Thoracic Society (BTS)9 have published guidelines for managing CAP. Adherence to guidelines has resulted in significant benefits for patients with CAP. In addition, other strategies such as lung protective-ventilation strategy10 and Surviving Sepsis Campaign11 recommendations introduced in recent years have improved outcomes in patients with severe sepsis admitted in the ICU.
We hypothesized that mortality in patients admitted to the ICU with SCAP has decreased even after implementation a higher organ support demand. In the current study we aimed to analyze changes in the epidemiology of SCAP in a large ICU population during 15-years’ surveillance and to determine the evolution of mortality rate and the factors associated with outcome.
Materials and methodsStudy populationWe conducted a retrospective cohort study of episodes of SCAP admitted to the ICU at university hospital in Spain (between January 1, 1999 and December 31, 2013).
Data abstractionThe following information was recorded using standardized methods: sex, age, alcohol use, comorbidities, initially prescribed antibiotic regimen, microbiological findings, and etiologic diagnosis. Intubation and mechanical ventilation requirements, systemic response and patient outcome were also recorded. Patients were observed until death or ICU discharge. Patients’ severity at admission was determined by major criteria of IDSA/ATS score.8
DefinitionsCAP was defined as an acute lower respiratory tract infection characterized by (1) evident acute pulmonary infiltrate compatible with pneumonia on chest radiographs, (2) confirmatory findings on clinical examination, and (3) acquisition of the infection outside of a hospital.
In accordance with criteria reported elsewhere,4 an organism was considered to be a definitive etiologic agent if one of the following conditions were met: (1) blood cultures positive for bacterial pathogens (in the absence of an extrapulmonary source of infection); (2) pleural fluid cultures yielding a bacterial pathogen; (3) in intubated patients, significant quantitative culture growth from respiratory specimens (protected specimen brush cultures ≥103cfu/ml, bronchoalveolar lavage fluid cultures ≥104cfu/ml, or quantitative endotracheal aspirate cultures ≥106cfu/ml); (4) in non-intubated patients a positive expectorated sputum culture with ≤10 epithelial cells and ≥25 polymorphonuclear cells per high power field; (5) detection of Streptococcus pneumoniae or Legionella urinary antigen enzyme immunoassay. Influenza viruses were diagnosed by polymerase chain reaction (PCR) assay. Identification of Pneumocystis jiroveci by direct immunofluorescence or culture of Legionella pneumophila or Mycobacterium tuberculosis from any of the samples was also considered to be sufficient for a diagnosis of CAP.
Cases where two or more pathogens were detected were classified as polymicrobial infection.4 Cases where no pathogens were detected were classified as CAP of unknown origin.
Alcoholism, chronic obstructive pulmonary disease (COPD), diabetes, and other comorbidities were diagnosed according to criteria reported elsewhere.12 Patients were considered immunocompromised when they had primary immunodeficiency or immunodeficiency secondary to radiation treatment, use of cytotoxic drugs or steroids (daily doses of 20mg of prednisolone or the equivalent for 2 weeks), or AIDS. Shock was defined as the need for vasopressors for ≥4h after fluid replacement.
Initial empirical treatment was defined as appropriate if an antibiotic prescribed within 24h of the first encounter with the patient matched the in vitro susceptibility of a pathogen deemed to be the likely cause of infection. Treatment decisions, including antibiotic prescriptions, were taken by attending physicians and were protocolized according to local adapted guidelines.
The ethics committee approved the study and waived the need for informed consent due to the observational nature of the study (Ethics Committee Corporació Sanitaria Universitaria Parc Taulí, 2014/675).
Data analysisTo analyze trends in SCAP, we considered the annual incidence rate and defined tree 5-year periods (1999–2003, 2004–2008, 2009–2013). We did a descriptive analysis of the data. Proportions were compared using the χ2 test with Yates correction or Fisher's exact test, when necessary. Means were compared using Student's t test. Values of P<0.05 were considered significant. We used backward stepwise elimination logistic-regression analysis for multivariate analyses; the dependent variable was ICU mortality and the independent variables were variables registered at ICU admission and that were associated with ICU mortality in the bivariate analysis. SPSS software (version 11.0, SPSS Inc., Chicago, IL, USA) was used for all analyses.
ResultsIncidenceIn the 15-year period, 458 patients were admitted to the ICU for SCAP. The cumulative incidence of patients with SCAP admitted to the ICU over the whole study period was 37.4episodes/1000 admissions, and the incidence progressively increased over the 3 periods, from 29.8episodes/1000 admissions in the first period, to 48.9episodes/1000 admissions in the third period (P<0.001).
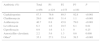
Patient characteristicsTable 1 reports the clinical characteristics of patients with SCAP admitted to the ICU in the three periods. On admission to ICU, a 73% of patients fulfilled at least 1 ATS/IDSA major criterion, and we observed an increase in the incidence of mechanical ventilation over the three periods. We observed a non-significant upward trend in the incidence of septic shock over the 3 periods. The incidence of patients fulfilling the two major IDSA/ATS criteria at admission (mechanically ventilation and need for vasopressors) increased from 64.2% in the first period to 82.5% in the last period (P<0.01).
Characteristics of the patients with severe community-acquired pneumonia.
| Total | P1 | P2 | P3 | P | |
|---|---|---|---|---|---|
| n:458 | n:124 | n:153 | n:181 | ||
| Age (±SD) | 61.3 (16) | 59.5 (18) | 63.3(16) | 60.6(16) | 0.13 |
| Male gender (%) | 69.0 | 70.2 | 70.6 | 67 | 0.21 |
| Severity | |||||
| Apache II (mean±SD) | 19.0±7.9 | 20.8±7.5 | 18.6±8.1 | 18.1±7.7 | 0.03 |
| CURB-65 (mean±SD) | 3.0±1.1 | 2.9±1.1 | 3.2±1.0 | 2.9±1.1 | 0.01 |
| ≥1 major criteria IDSA/ATS (%) | 73.0 | 64.2 | 72.8 | 82.5 | <0.01 |
| Comorbidities (%) | |||||
| COPD | 30.8 | 27.6 | 34.4 | 28.0 | 0.42 |
| Alcoholism | 14.4 | 18.0 | 11.0 | 14.4 | 0.26 |
| Chronic renal failure | 4.8 | 8.9 | 5.2 | 1.6 | 0.01 |
| Cardiovascular disease | 21.0 | 23.4 | 24.8 | 16.0 | 0.10 |
| Cancer | 15.3 | 12.1 | 15.0 | 17.7 | 0.41 |
| Diabetes | 24.1 | 28.5 | 26.8 | 17.1 | 0.04 |
| HIV | 8.1 | 5.6 | 9.2 | 8.8 | 0.50 |
| Immunocompromised | 9.6 | 8.9 | 7.2 | 12.2 | 0.29 |
| Patients with ≥2 comorbidities | 52.3 | 53.7 | 54 | 49.5 | 0.60 |
| Septic shock (%) | 47.2 | 38.2 | 44.8 | 50.0 | 0.54 |
| Mechanical ventilation (%) | 67.2 | 56.9 | 63.0 | 72.0 | 0.02 |
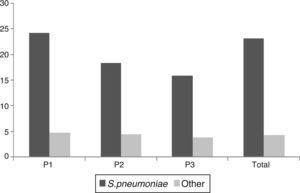
We observed significant variations in the etiology of SCAP over the 3 periods (Table 2). S. pneumoniae was the most frequent pathogen in all 3 periods, with an overall incidence of 41.7%. We observed a non-significant trend toward a progressive reduction in the incidence of L. pneumophila over the 3 periods and a significant increase in polymicrobial episodes and viral pneumonias in the last period. Among patients with viral pneumonia, influenza was diagnosed in 64% of the episodes, all of which occurred in the last period (2009–2013). Among polymicrobial episodes, 35.2% were co-infections of influenza and S. pneumoniae or Staphylococcus aureus and 23.5% were co-infections of S. pneumoniae and Haemophilus influenzae. The overall incidence of SCAP episodes of unknown etiology was 27.5%. The overall incidence of SCAP episodes with bacteremia was 23.1%; S. pneumoniae was the microorganism most frequently responsible for bacteremia in the 3 periods, accounting for 81.1% of all episodes. We observed a progressive decrease in the overall incidence of bacteremia over the 3 periods (P=0.02) (Fig. 1); this decrease was primarily due to the significant decrease in the incidence of S. pneumoniae bacteremia.
Distribution of etiology of severe community-acquired pneumonia over 15 years.
| Pathogen (%) | Total | P1 | P2 | P3 | P |
|---|---|---|---|---|---|
| n:458 | n:124 | n:153 | n:181 | ||
| Streptococcus pneumoniae | 191 (41.7) | 49 (38.7) | 73 (47.7) | 70 (38.6) | 0.18 |
| Legionella pneumophila | 29 (6.3) | 13 (10.4) | 8 (5.2) | 8 (4.4) | 0.08 |
| Virusa | 25 (5.4) | 5 (4.0) | 4 (2.6) | 16 (8.8) | 0.03 |
| Pseudomonas aeruginosa | 12 (2.6) | 4 (3.2) | 8 (5.2) | – | 0.01 |
| Staphylococcus aureus | 10 (2.1) | 3 (2.4) | 4 (2.6) | 3 (1.6) | 0.80 |
| Enterobacteriaceae | 10 (2.1) | 4 (3.2) | 4 (2.6) | 2 (1.1) | 0.40 |
| Pneumocystis jiroveci | 8 (1.7) | 2 (1.6) | 2 (1.3) | 4 (2.2) | 0.80 |
| Haemophilus influenzae | 6 (1.3) | 2 (1.6) | 1 (0.6) | 3 (1.6) | 0.60 |
| Other Gram positive | 4 (0.8) | 1 (0.8) | – | 3 (1.6) | 0.20 |
| Miscellaneousb | 17 (3.7) | 8 (6.4) | 5 (3.2) | 4 (2.2) | 0.10 |
| Polymicrobial | 20 (5.4) | 1 (0.8) | 2 (1.3) | 17 (9.3) | <0.001 |
| Unknown origin | 126 (27.5) | 33 (26.6) | 42 (27.4) | 51 (28.1) | 0.9 |
Of the 332 (72.5%) patients with definitive etiology, 302 (91%) were administered appropriate empiric antibiotic treatment. The proportion of patients administered appropriate empiric antibiotic treatment increased from 78.3% in the first period to 97.7% in the last period (P<0.001). The use of combination antibiotic therapy (betalactam+macrolide or fluoroquinolone) also increased between the first and last periods (61% vs. 81.3%) (P<0.001). Cephalosporins (87.3%), particularly ceftriaxone, were the most widely used antibiotics for treating SCAP, followed by macrolides (75.7%) and quinolones (7.2%) (Table 3). We observed a significant increase in the use of cephalosporins and azithromycin over the three periods in parallel to a decrease in the use of clarithromycin.
Antibiotic treatment over 15 years.
| Antibiotic (%) | Total | P1 | P2 | P3 | P |
|---|---|---|---|---|---|
| n:458 | n:124 | n:153 | n:181 | ||
| Cephalosporins | 87.3 | 76.6 | 89.5 | 92.8 | <0.001 |
| Clarithromycin | 29.0 | 66.9 | 31.4 | 1.1 | <0.001 |
| Azithromycin | 46.7 | 0.8 | 45.8 | 79.0 | <0.001 |
| Levofloxacin | 6.3 | 1.6 | 10.5 | 6.1 | 0.01 |
| Ciprofloxacin | 0.9 | 1.6 | 1.3 | 0 | 0.25 |
| Amoxicillin–clavulanic | 2.2 | 5.6 | 1.3 | 0.6 | 0.008 |
| Othera | 35.1 | 27.1 | 33.4 | 39.5 | <0.001 |
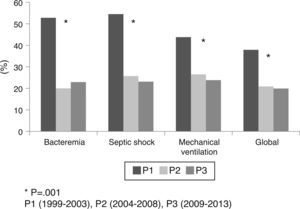
Overall ICU mortality was 25.1%; ICU mortality progressively decreased over the periods from 37.9% in the first period to 19.9% in the last period (P=0.001). This progressive decrease in ICU mortality over the 3 periods also held true for the subgroups of patients with bacteremia, patients with septic shock, and mechanically ventilated patients (Fig. 2). The mortality of patients with combined treatment with cephalosporin and macrolides was 25.6% and the combination with quinolones was 26.7% (P:1.00). Variables significantly associated with death in the bivariate analysis are shown in Table 4. In the multivariate analysis the variable associated with the highest risk of death was admission during the first period (OR 3.59, CI 2.05–6.30; P<0.001). Table 5 shows further details from the multivariate analysis. Repeating the multivariate analysis, only with episodes with etiologic diagnosis, the variables selected but the model were identical, maintaining the appropriate treatment as a protective factor.
Prognostic factors associated with mortality (bivariate analysis).
| Variables | Patients, n (%) | Death (%) | P |
|---|---|---|---|
| Age | |||
| <65 yrs | 246 (53.7) | 20.2 | 0.001 |
| ≥65 yrs | 212 (46.3) | 33.5 | |
| Sex | |||
| Male | 316 (68.9) | 26.2 | 0.399 |
| Female | 142 (31.1) | 23.2 | |
| Acute Physiology and Chronic Health Evaluation II Score | |||
| ≥15 | 301 (65.7) | 31.2 | 0.001 |
| <15 | 157 (34.3) | 17.2 | |
| Period of admission | |||
| P1 (1999–2003) | 124 (27.0) | 37.9 | 0.001 |
| P2 (2004–2008) | 153 (33.4) | 20.9 | |
| P3 (2009–2013) | 181 (39.5) | 19.9 | |
| Comorbidities | |||
| COPD | 141 (30.7) | 27.7 | 0.415 |
| Alcoholism | 69 (15.0) | 24.6 | 1.000 |
| Chronic renal failure | 22 (4.8) | 31.8 | 0.455 |
| Cardiovascular disease | 96 (20.9) | 26.0 | 0.793 |
| Cancer | 70 (15.2) | 40.0 | 0.003 |
| Diabetes | 88 (19.2) | 18.2 | 0.102 |
| VIH | 37 (8.0) | 27.0 | 0.843 |
| Immunocompromised | 44 (9.6) | 45.5 | 0.003 |
| Bacteremia | 106 (23.1) | 32.1 | 0.073 |
| Septic shock | 216 (47.1) | 31.9 | 0.002 |
| Mechanical ventilation | 308 (67.2) | 29.9 | 0.001 |
| Appropriate empiric antibiotic treatmenta | 302 (90.9) | 25.5 | 0.009 |
Multivariate analysis for independent factors associated with ICU mortality.
| Variables | Odds ratio | 95% Confidence interval | Variables |
|---|---|---|---|
| Admission in the period 1 (1999–2003) | 3.59 | 2.05–6.30 | <0.001 |
| Immunosuppression | 2.11 | 0.98–4.50 | 0.05 |
| Bacteremia | 1.75 | 1.01–3.02 | 0.04 |
| Mechanical ventilation | 1.68 | 1.00–2.83 | 0.04 |
| Age≥65 yrs | 1.03 | 1.01–1.04 | <0.001 |
| Appropriate empiric antibiotic treatment | 0.472 | 0.23–0.95 | 0.03 |
This study provides a comprehensive picture of the clinical and microbiologic epidemiology of SCAP over 15-year periods in a large ICU population. The main findings were the progressively higher incidence of SCAP in patients admitted to ICU and the 18% reduction in crude ICU mortality.
Although the definition of SCAP remains somewhat subjective and imprecise, in practice, SCAP is often defined by respiratory and/or circulatory failure requiring admission to the ICU.13 The IDSA/ATS Joint Guidelines list two major criteria for SCAP, septic shock and the need for mechanical ventilation, either of which is sufficient for the diagnosis.8 Although for various reasons, such as local policies and resource availability, not all patients admitted to ICUs meet the aforementioned criteria, the patients included in the present study had a high incidence of septic shock and need for mechanical ventilation. In fact, the incidence of patients admitted to our ICU with SCAP who had septic shock or required mechanical ventilation increased over the three periods. However, despite the increase in the incidence of shock and need for mechanical ventilation, we observed a progressive reduction in Apache II scores at admission. This reduction was attributed in part to a reduction in the incidence of preexisting comorbidities such as chronic renal failure, diabetes, and cardiovascular disease in the last period.
In recent years, hospital admissions for pneumonia have increased in the United States, Denmark, and the Netherlands.14–17 Our study found a progressive increase in the incidence of SCAP in patients admitted to our ICU over a 15-year period (15.7% between the first and second periods and 41.7% between the second and third periods). The overall increase of the incidence of SCAP between 1999 and 2013 was 64%; these results are in line with those reported in the largest multicenter study of admissions to the ICU for CAP published in 2006 where the incidence between 1995 and 2004 rose 128%.18 This increase in the number of patients with pneumonia admitted to ICUs could be attributed to an increase in the incidence of pneumonia patients admitted to the hospital or to an increase in the availability of ICU beds, which would allow more hospitalized patients to be admitted to the ICU. However, the number of beds in our ICU remained unchanged throughout the study period, so the increase in the number of patients with SCAP admitted to ICU is most likely due to other factors. Our results suggest that the main reason for the progressive increase in the incidence of SCAP was the increased severity of patients admitted with CAP. Indeed, the proportions of patients admitted with septic shock and of those requiring invasive mechanical ventilation increased over time (64.2% fulfilled≥1 major criteria of ATS/IDSA at admission in the first period, 72.8% in the second period, and 82.5% in the third period; P<0.01).
The most frequently isolated pathogen was S. pneumoniae, and there were no significant differences between the 3 periods. This finding is not surprising, as S. pneumoniae continues to be the leading microorganisms causing SCAP despite widespread pneumococcal vaccination programs.8 The second most frequently isolated pathogen responsible of SCAP in our study was L. pneumophila. However, most of the L. pneumophila cases accounted in the first period and the incidence remained stable over the last decade. These findings corroborate those of a recent study about L. pneumophila CAP in a university hospital, which found similar stability in the incidence of ICU admission over a 15-year period.19 Unexpectedly, the third most common cause of SCAP in our study was viral, mainly due to the increase in the incidence of influenza pneumonia in the last period. The 2009 influenza A H1N1 pandemia significantly increased the incidence of viral pneumonias and created the need for the use of rapid techniques that have improved the diagnosis of viral pneumonia. A similar increase in the incidence of viral pneumonia has been reported in different ICUs and countries since the 2009 pandemia.20,21
The overall incidence of bacteremia was 23%; however, we found a progressive decline in the incidence of bacteremia, largely due to the reduction in pneumococcal bacteremia. A plausible explanation for these findings could be the widespread use of pneumococcal vaccination in general and the introduction of the 23-valent vaccine in particular. This vaccine protects against invasive pneumococcal disease, but not against less invasive infections that do not cause bacteremia as it has been suggested elsewhere.22 A study in patients older than 65 years published in 200323 found that the 23-valent vaccine was effective against invasive pneumococcal disease in immunocompetent patients, but did not decrease the risk of developing any type of pneumococcal pneumonia. In our region, a pneumococcal prevention vaccination program was launched in October 1999, and a multicenter case–control study of the effectiveness of this program published in 2005 found the vaccine was 76% effective in preventing disease in immunocompetent elderly adults.24
Our results show a gradual change in the treatment of patients with SCAP. The use of combination antibiotic therapy increased gradually, from 61% in the first period to 81.3% in the third (P<0.001). The combination of a cephalosporin with a macrolide predominated in every period, but azithromycin gradually replaced clarithromycin in the last decade. These changes were associated with a progressive increase in the effectiveness of empirical antibiotic treatment. A recent article25 reported a similar evolution in the use of antibiotics in a study comparing prescribing practices for patients with pneumococcal SCAP between 2000 and 2013, where combination antibiotic therapy increased from 66.2% to 87.5% and the use of azithromycin progressively increased.
In our study, we also found a progressive increase in the use of other antibiotics (carbapenems, aminoglycosides, cotrimoxazole, antivirals, and tuberculostatics). This increase can be explained by two factors. First, the publication of guidelines26 which recommended empiric antibiotic treatment in patients with healthcare-associated pneumonia in 2005 (toward the beginning of the second period) recommended empiric combination therapy with broad-spectrum antibiotics due to an increased risk of multiresistant microorganisms; second, from 2009 antiviral treatment was often included to empirically cover influenza pneumonia.
Our results show that appropriate empiric antibiotic treatment is associated with lower ICU mortality. As in other studies,27,28 the decrease in ICU mortality can be explained in part by the increase use of combination antibiotic therapy. We also found a decrease in mortality in patients with septic shock and mechanical ventilation, corroborating the results of a recent study.25 The decline in mortality in our study is probably also related with the progressive decrease in the incidence of bacteremia; although the influence of bacteremia on the prognosis of patients with pneumococcal pneumonia is controversial,29 invasive pneumococcal infection has been associated with increased mortality.30 In addition, other strategies such as lung protective-ventilation strategy13 and Surviving Sepsis Campaign14 recommendations introduced during the study period may be also influenced the outcome in our patients.
Our study has some limitations. First, due to the epidemiological nature of the study, antibiotic treatment, hemodynamic support and mechanical ventilation were not standardized. However, since the study was performed in a single ICU, significant variations in these aspects of patient management among physicians are unlikely. Second, the incidence of pneumococcal vaccination and pneumococcal serotypes was not recorded. Moreover, we did not distinguish between CAP and healthcare-associated pneumonia throughout the study period; nevertheless data from a recent Spanish multicenter study suggest that the prognosis among critical patients with CAP and healthcare-associated pneumonia is similar.31
In summary, our study shows that the incidence and mortality of SCAP have changed dramatically over the last 15 years. Despite a higher incidence of SCAP in patients admitted in the ICU, there was an 18% reduction in crude ICU mortality. This improvement in prognosis was associated with increased use of combination antibiotic therapy and a reduction in the incidence of bacteremia.
Conflict of interestThe authors do not have potential conflicts of interest with any companies/organizations whose products or services may be discussed in this article.