Traumatic brain injury (TBI) is considered a health problem and one of the main causes of morbidity and mortality. Its overall annual incidence rate is 200 people for every 100,000 inhabitants. In developing countries, the prevalence is higher, and it mainly affects young and male adults who have been the victim of a traffic accident or violence. However, in developed countries, this prevalence is lower, and it affects older individuals with sports traumas, falls, or hit-and-runs. In first-world countries with resources and systems of organized care, the predominant causes of death are refractory endocranial hypertension, and late multiple organ dysfunction syndrome while in low-income countries, the predominant causes are avoidable causes such as lesions associated with bleeding and hypoxemia.1
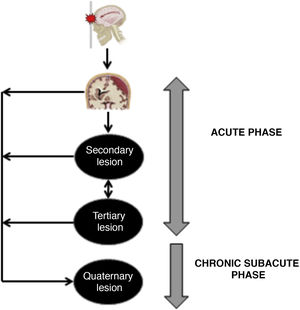
Pathophysiology of severe traumatic brain injurySevere TBI is a heterogeneous, dynamic, and progressive condition.2 It causes different types of damage due to the external energy applied and absorbed by the cranioencephalic structures (scalp, bones, brain parenchyma, CSF, blood vessels).3 The type of injury sustained will basically depend on the location and amount of mechanical load exerted.3 There are different types of mechanical load: hit or direct impact, counter-hit, acceleration and deceleration phenomena, rotation, revolution, angulation, and penetrating injuries with or without expansive waves. The aforementioned mechanisms transmit energy with a static (unmovable) or dynamic (unmovable) skull.3 The nature, intensity, and duration of the energy forces described will determine the pattern and spread of the damage sustained.3 Brain injuries interact among themselves on an ongoing basis from the very moment of the accident and can be maintained along the different evolutionary stages of TBI including subacute and chronic periods that can be categorized into 4 different types of pathophysiological alterations: primary and secondary injuries2,3 whose concepts, etiology, pathophysiology, macro- and microscopic morphology both of primary and secondary injuries have been properly described and are well-known to all of us.2–4 In this manuscript we will be introducing new concepts of tertiary and quaternary injuries whose involvement in the prognosis of TBI has not been fully explained to this date (Fig. 1).
TBI is an entity with a strong systemic impact. It is essential to understand TBI as an evolutionary process emphasizing the impact it has on mortality and the invalidating sequelae of a primary injury and the development and perpetuation of secondary injuries. However, it is essential to consider within the same “continuum” of multifactorial brain damage, the presence and role of what we call “tertiary injury”, which clearly impacts the pathophysiology of TBI with the same or greater importance compared to primary and secondary injuries.
We describe tertiary injuries as those due to the care and assistance provided to the patient who has sustained a TBI.5–7 These lesional mechanisms often occur in the context of treatment and prevention of secondary injuries including, though not limited to: (1) complications associated with prolonged stays at the intensive care unit; (2) adverse events associated with drugs or homoderivatives; (3) mechanical ventilation-induced lesions; (4) infections associated, or not, with invasive devices; y (5) multifactorial complications (critical illness myopathy)5–7 (Table 1).
Description of the spectrum of a potential tertiary injury in traumatic brain injury.
| Therapeutic measure | Indication and reason for implanting the measure | Potentially associated tertiary injury |
|---|---|---|
| Cervical immobilization | Stabilization of lesions of the spinal column, prevention of falls | Increased ICP due to compromised venous drainage at the expense of jugular compression. |
| Analgesia and sedation | Control anxiety, agitation, and pain as contributors to an increased ICP | Propofol: propofol infusion syndrome. |
| Control of the patient-ventilator asynchrony | Dexmedetomidine: bradycardia, hypotension, reduced CPP. | |
| Fentanyl: respiratory depression, increased ICP, secondary compromise of cerebral oxygenation. | ||
| Midazolam: hypotension, reduced CPP, exacerbation of delirium. | ||
| Neuromuscular relaxants | Control ECH | Masked epileptic seizures, pneumonia, association with critical illness myopathy |
| Activation of mechanical ventilation, intense agitation, and protocols for the management of hypothermia | ||
| Hyperosmolar solutions (mannitol, hypertonic saline solution) | First level measures to control elevated ICP | Mannitol: acute kidney injury, volume overload, electrolytic alterations, hypovolemia, kidney failure, rebound edema cerebral |
| Hypertonic SS: phlebitis, coagulopathies, hyperchloremia, hypernatremia, acute kidney injury, volume overload, pontine myelinolysis (rare) | ||
| Hyperventilation | Control elevated ICP | Secondary cerebral ischemia (vasoconstriction, high-affinity cerebral hypoxia) |
| Systemic effects (myocardial, intestinal ischemia) | ||
| Barbiturates | Second level measure as “metabolic suppression”, control refractory ECH | Myocardial depression, sepsis |
| Ileus and intestinal obstruction | ||
| Catheters and intraventricular devices, SjvO2, PtiO2, microdialysis, central, vesical | Multimodal monitorization of the neurocritical patient with TBI | Catheter-related infections (ventriculitis, meningitis, cerebral abscess, pneumonia, urinary tract infections). Bleeding, thrombosis |
| Mechanical ventilation | Secure airway and control ECH and cerebral hypoxia | Mechanical ventilator-induced lung injury |
| Barotrauma, biotrauma, volutrauma. Associated pneumonias. Damage to artificial airway | ||
| Transfusion of hemoderivatives | Treatment of anemic cerebral hypoxia, hemodynamic stabilization, and damage control in acute traumatic bleeding | Associated/induced pulmonary injury and cardiovascular overload, transfusion. Sepsis. Hemolysis. Transfusion reactions. Transmission of infections. |
| Stay at the intensive care unit | Comprehensive and multidisciplinary management of the patient with TBI | Digestive bleeding, pressure ulcers, venous thromboembolism, exposure to nosocomial germs, critical illness myopathy, neuropathy, and malnutrition |
CPP, cerebral perfusion pressure; ECH, endocranial hypertension; ICP, intracranial pressure; PtiO2, brain tissue oxygen pressure; SjvO2, jugular venous bulb hemoglobin oxygen saturation; SS, saline solutions; TBI, traumatic brain injury.
The potentially damaging impact of therapeutic measures implemented for the management of TBI has still not been determined fully. However, this new concept of tertiary injury should not be underestimated. As a matter of fact, it is very useful to assess the possible complications and risk associated with a certain therapy administered, at one time or another, during the comprehensive process of managing a TBI. The Hippocrates premise “primun non nocere” becomes very important here since it would be paradoxical to “hurt while caring”.
Similarly, it is essential to establish protocols and specific prevention measures to control the appearance and progression of this type of lesions.
Quaternary injuriesWe describe quaternary injuries as those events that occur during the subacute and chronic period of the TBI. Overall, they cause tissue loss and exacerbate the primary injury. The lesional pathophysiological mechanism of quaternary injuries is still operative even after the acute phase when the process of cellular damage seems to have stopped. Adult reparative neurogenesis appears as a process that tries to counteract or ameliorate the damage.8 Experimental studies have confirmed the proliferative capacity of the nervous tissue.8 Certain specific lesional biological markers of the central nervous system like the S100β protein and the neurotrophins stimulate endogenous neurogenesis. However, the efficacy and presence of this reparative phenomenon are variable and controversial, and to this date its true impact remains unknown.8,9
During this period, the following lesional mechanisms are operative:8
- •
Persistence of the inflammatory phenomenon.
- •
Lack of mitigation of the processes of cellular death (necrosis, apoptosis).
- •
Incomplete clean of detritus or debris generated during the lesional process. For example, beta-amyloids, molecular patterns of damage, and myelin compromise the glial function and activate proinflammatory phenotypes. Also, the myelin that is not eliminated causes an autoimmune response capable of triggering demyelination.
- •
Aberrant immune response. For example, different signals originated on the neuronal surface that activate the phagocytosis of these by the glia.
- •
Glial neurotoxicity: on experimental trials it has been observed that the glia releases inflammatory mediators that “corrupt” the astrocytes, which, in turn, trigger neuronal toxicity.
In our own opinion, quaternary injuries have a strong genetic influence, which would explain why 2 individuals with the exact same injury, demographic factors, and comorbidities, among other characteristics, evolve differently and on an individual basis. Some authors have proven that patients who are carriers of the isoform e4 of apolipoprotein E that is involved in cognitive function disorders and further development of Alzheimer’s disease have worse functional results in the long-term.10
Similarly, in the future, the quaternary injury could be therapeutically modified. Its most significant and visible targets are the inflammatory phenomenon, the immune response, and the process of reparative neurogenesis.8
ConclusionsIn the pathophysiology of TBI, the concepts of tertiary and quaternary injuries arise as new mechanisms of brain injury that should be taken into consideration for a holistic management of care and treatment of TBIs. In the future, the research lines currently ongoing could be shedding light on many of these unsolved challenges.
Conflicts of interestNone reported.
Please cite this article as: Godoy DA, Murillo-Cabezas F. Conceptualización evolutiva de los mecanismos lesionales en el traumatismo craneoencefálico. Med Intensiva. 2022;46:90–93.