To report sleep quality and identify related factors.
DesignA descriptive cross-sectional study was made with a convenience sample of 129 patients. The differences between 3 periods were evaluated using the Wilcoxon test and Spearman correlation r. Multiple regression analyses were performed to relate independent variables to sleep quality.
SettingThe Department of Intensive Care Medicine of a tertiary hospital.
ParticipantsPatients admitted between February 2016 and December 2017.
InterventionsQuestionnaire administration.
VariablesItems of the modified Freedman questionnaire, and demographic and clinical variables.
ResultsExternal factors interfering with sleep quality were noise and constant light exposure in the 3 periods, with significant differences between these periods in nursing care (P = 0.005) and nursing activities (P = 0.019). The other factors affecting sleep quality and identified by the multivariate regression model were age (P = 0.012), daily alcohol intake (P = 0.023), benzodiazepine use during admission to the ICU (P = 0.01) and comorbidities (P = 0.005). There were significant differences in sleepiness between discharge and the first day (P ≤ 0.029) and between discharge and half stay (P = 0.001).
ConclusionsNoise and light were the most annoying factors, but statistical significance was only reached for nursing activities and care. Age, alcohol intake, benzodiazepine use in the ICU and a higher comorbidity index had a negative impact upon sleep. Sleepiness was reduced at the end of stay.
Describir la calidad del sueño e identificar los factores que la afectan.
DiseñoEstudio observacional descriptivo y transversal realizado con una muestra de conveniencia de 129 pacientes. La diferencia entre los 3 tiempos se calculó mediante la prueba de Wilcoxon y la correlación entre variables mediante la r de Spearman. Con análisis de regresión múltiple se relacionaron las variables independientes con «calidad del sueño».
ÁmbitoServicio de Medicina Intensiva de un hospital terciario.
ParticipantesPacientes ingresados en la unidad entre febrero de 2016 y diciembre de 2017.
IntervencionesAdministración de un cuestionario.
VariablesÍtems del cuestionario Freedman modificado, variables demográficas y de episodio.
ResultadosLos factores que más afectaron a la calidad del sueño en los 3 tiempos de forma constante fueron el ruido y la luz. Hubo diferencias entre los 3 tiempos para los cuidados (p = 0,005) y actividades de enfermería (p = 0,019). Mediante el modelo de regresión múltiple se encontró que otros factores que influían en la calidad del sueño eran la edad (p = 0,012), la ingesta habitual de alcohol (p = 0,023), la administración de benzodiacepinas en UCI (p = 0,01) y la comorbilidad (p = 0,005). Resultaron diferencias significativas en somnolencia entre el alta y el primer día (p ≤ 0,029), y entre el alta y la mitad de la estancia (p = 0,001).
ConclusionesLa somnolencia disminuyó al final de la estancia. Aunque el ruido y la luz fueron los factores más molestos, solo los cuidados y actividades de enfermería resultaron significativos. La edad, la ingesta habitual de alcohol, la administración de benzodiacepinas en UCI y un mayor índice de comorbilidad interfieren negativamente en la calidad del sueño.
Sleep is a basic need that modulates the immune system, regulates homeostasis and improves certain cognitive functions. In addition, it contributes to ensure adequate physiological activity through hormone secretion and anabolic stimulation1,2.
In the Intensive Care Unit (ICU), due to its characteristics and the seriousness of the patient conditions, there is an increased prevalence of alterations of circadian rhythm and sleep disturbances, with both qualitative and quantitative privations3,4. Studies in the critically ill have reported a prevalence of sleep disturbances of 22–61%. Such patients present alterations in sleep patterns, characterized by a predominance of the N1 phase (light sleep) and the N2 phase (lowered muscle tone), with a decrease or absence of the N3 phase (deep and repairing sleep) and rapid eye movement (REM) sleep. The patients suffer frequent awakenings, a high arousal index and periods of daytime sleep (40–50% of sleep may take place during the day)5–7. These individuals are rarely able to complete a full sleep cycle8,9.
The Critical Care Medicine Society has presented 18 recommendations aimed at minimizing the negative effects of pain, agitation, delirium, immobility and sleep disruption in the critical patient (the PADIS guidelines), and has proposed a multicomponent protocol to promote sleep in the critically ill. On the other hand, it underscores the need to evaluate these episodes in a coordinated manner10.
The evaluation of sleep in critical patients is a complex process11–13, and objective tools are needed for this purpose. However, these tools – such as polysomnography (PSG) and actigraphy – are not available in all ICUs, and professionals specifically trained to interpret the data obtained are moreover needed. In this setting the alternative is to evaluate sleep using subjective methods based on questionnaires, which despite their associated subjectivity bias are less expensive and are easier to apply14,15.
ObjectivesTo describe sleep quality in the critical patient and identify its conditioning factors, and to evaluate differences in sleep quality and drowsiness during patient admission to the ICU.
Patients and methodsStudy designA descriptive cross-sectional study was carried out in the Department of Intensive Care Medicine of Hospital General Universitario de Castellón (Castellón, Spain). This hospital has a polyvalent ICU comprising a critical care unit with 15 beds and an intermediate care unit with 6 beds.
Study participantsThe study included patients admitted to the Department of Intensive Care Medicine in the period between 23 February 2016 and 20 December 2017. A convenience sample was recruited, comprising patients meeting the inclusion criteria and who signed the informed consent document.
The analyzed critical patients were required to be over 18 years of age and to be able to speak Spanish. Patients with neuromuscular block were excluded, as were those with hearing or speech problems, a prior diagnosis of dementia or a history of substance abuse. We also excluded patients with neurological disorders (Glasgow coma score < 12) and individuals with a sedation score on the Richmond Agitation- Sedation scale out of range (+1 and −1).
Study procedureBefore the study was started, the protocol was presented to the Department of Intensive Care Medicine and was approved by the Research Ethics Committee of Hospital General Universitario de Castellón.
The instrument used to evaluate sleep quality and the factors influencing it was the questionnaire developed by Freedman et al. in 199916, in its modified version translated into Spanish and published by Gómez-Sanz17and subsequently validated by our group18. The items are measured using Likert-type scales from 0 to 10 points. We also took into account other factors that could affect sleep quality, such as patient age and gender, the type of admission, the temperature in the patient room, pain as scored by a visual analog scale (VAS), routine alcohol intake and use of opiates or benzodiazepines, severity assessed by the APACHE II score, sleep medication used in the home, and comorbidity assessed with the Charlson index.
The data were compiled in the early morning between 8–10 a.m. The questionnaire was distributed on a heteroadministered basis. Data were recorded on the first day of admission, half-way through the ICU stay, and on the day of discharge from the Unit.
Statistical analysisThe description of the characteristics of the sample was based on calculation of the median and interquartile range (IQR). Continuous variables were reported as the mean and standard deviation (SD). The reliability of the questionnaire was assessed using the Cronbach α coefficient, and normal data distribution was assessed with the Kolmogorov-Smirnov test. The differences among the three different study timepoints were explored using the Wilcoxon signed-rank test for related samples, and associations between variables were analyzed with the Spearman correlation test (r). Multiple linear regression analysis in turn was used to relate the independent variables to the dependent variable “sleep quality”. The statistical analysis was conducted using the SPSS version 23.0 statistical package. Statistical significance was considered for p ≤ 0.05.
ResultsThe study sample consisted of 129 patients. Their characteristics are described in Table 1.
Characteristics of the patients and of admission to intensive care.
| Baseline characteristics of the patients | |
| Age | 60 (52−72) |
| Female gender | 49 (38) |
| BMI | 27.42 (24.35−30.48) |
| Charlson index | 1 (1−4) |
| Alcohol consumption | 17 (13.18) |
| Smoking | 47 (36.43) |
| Use of hypnotic drugs (home) | 37 (26.36) |
| Reason for admission | |
| Medical | 60 (46.5) |
| Postsurgery | 30 (23.3) |
| Coronary | 24 (18.6) |
| Trauma | 15 (11.6) |
| Unit of admission | |
| ICU | 92 (71.32) |
| UCIm | 37 (28.8) |
| APACHE II | 11 (5−6) |
| Days of stay in ICU | 6 (4−9) |
The data are reported as the median (IQR) or numbers (%).
BMI: body mass index; ICU: Intensive Care Unit; UCIm: Intermediate Care Unit; MV: mechanical ventilation; IMV: invasive mechanical ventilation; NIMV: noninvasive mechanical ventilation.
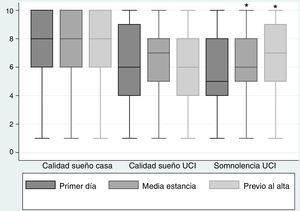
The descriptive results referred to the evaluation of sleep and drowsiness are presented as the mean and standard deviation (Fig. 1). The Kolmogorov-Smirnov test evidenced a non-normal distribution of the variables. The Wilcoxon signed-rank test was therefore used to evaluate differences among the three timepoints. There were no significant differences in sleep quality in the ICU, though significant differences in drowsiness were recorded between discharge and the first day of ICU stay (p ≤ 0.029), and between discharge and half-stay (p = 0.001). There were significant differences in sleep quality between the patient home and the ICU at the three timepoints (p = 0.001); the highest mean values corresponded to the variable “sleep quality at home”.
The descriptive results referred to the environmental factors influencing sleep quality and their differences at the three study timepoints are reported in Table S1. In all cases the mean values were higher on the first day of ICU stay than at discharge from the Unit, though statistical significance was only reached for nursing care and activities, and for sample extraction and the administration of medications.
With regard to the factors related to noise and which interfere in sleep quality, the highest values were likewise higher on the first day of ICU stay and at half-stay than at discharge from the Unit, in all cases, except for the variable “hearing people speaking”, where the values were lower at half-stay than upon admission or at discharge (Table S2).
The study of the associations between sleep quality and the factors related to both the environment and to noise evidenced no strong correlations. We recorded moderate correlations between sleep quality at discharge and noise, and sleep quality at half-stay and nursing care, diagnostic tests and nursing activities (Table S3).
Lastly, multiple linear regression analysis of the effect of other factors upon sleep quality, considering the three study timepoints, only revealed an association with assessment on the first day of admission (Table 2).
Multiple linear regression model: sleep quality on the first day of admission.
| B | Standard error | β | t | Sig. | |
|---|---|---|---|---|---|
| (Constant) | 6.883 | 1.301 | 5.289 | 0.000 | |
| Age | −0.040 | 0.018 | −0.208 | −2.208 | 0.029 |
| Gender | 0.701 | 0.483 | 0.128 | 1.450 | 0.150 |
| Alcohol | 1.459 | 0.677 | 0.185 | 2.155 | 0.033 |
| NIMV | 0.119 | 0.479 | 0.022 | 0.248 | 0.804 |
| APACHE II | 0.005 | 0.032 | 0.015 | 0.167 | 0.868 |
| VAS | −0.046 | 0.083 | −0.050 | −0.549 | 0.584 |
| Charlson index | 0.251 | 0.102 | 0.242 | 2.461 | 0.015 |
| Benzodiazepines | −1.502 | 0.487 | −0.264 | −3.082 | 0.003 |
| Temperature of the room | 0.753 | 0.310 | 0.217 | 2.427 | 0.017 |
| Use of sleep medications at home | −0.110 | 0.569 | −0.018 | −0.193 | 0.848 |
Dependent variable: sleep quality on the first day of admission to the ICU.
VAS: visual analog scale; NIMV: noninvasive mechanical ventilation.
F = 2.872.
p = 0.003.
R = 0.442; R2 = 0.196; R2 adjusted = 0.128.
The multifactorial nature of sleep disruption in the ICU and the vulnerability of critical patients make it difficult to clearly define the factors that modify sleep quality19. What is clear is that these patients suffer a worsening of sleep quality during their stay in the ICU compared with sleep at home, and in this regard our findings are consistent with those reported by Freedman16and by most of the existing literature20. We recorded no statistically significant differences referred to sleep during ICU stay as recently reported by Al Mutair et al.21, though we did document a significant decrease in patient drowsiness at the end of admission to the ICU.
If we were to use the recoding proposed by Gémez-Sanz17 and accept sleep quality scores of 1–5 as indicating “sleeping poorly”, and 6–10 as indicating “sleeping well”, it could be concluded that our patients slept adequately – though this certainly would be questionable, given the dispersion of the results and the fact that the highest mean value did not exceed χ− = 6.29 at the time of discharge from the ICU. The same can be said of drowsiness: scores of 1–5 indicate “daytime drowsiness” and scores of 6–10 indicate “remains alert and awake”, though with a mean value of χ− = 6.92) at the time of discharge, it is not possible to affirm that the patient remained alert and awake.
On analyzing the environmental factors that prove most annoying for the patient, noise and light exposure were identified as the main problems, though only “nursing care and activities” and “sample extraction and the administration of medications” were found to be significantly higher on the first day of admission and at half-stay than at the time of discharge from the Unit. The same was observed in the case of the factors related to noise: alarms, hearing people speaking, nebulizations and the aspiration of secretions were identified as the most annoying factors on the first day of admission and at half-stay. Similar results, though evaluated on a global basis, have recently been published by Lewandowska22.
On correlating sleep quality with the environmental factors, we found a significant and negative association in all cases at half-stay and at discharge, with the exception of light exposure, which proved more annoying on the first day of ICU stay. Similar observations apply to the noise-generating factors, except the aspiration of secretions and use of the telephone, which in our study were not associated to the interruption of sleep.
The study carried out by Boyko et al.23, involving a sample of 17 patients, recorded no significant relationship between patient age, gender, severity, the administration of analgesia-sedation with remifentanil and an abnormal sleep pattern as evaluated by polysomnography. Our results are similar in terms of gender and severity. However, we did observe a significant correlation to age, with older age being associated to poorer sleep quality. Pain showed no significant association, in coincidence with the observations of Elliot et al.24 – a fact that may be interpreted as indicating adequate pain management in our Unit.
The regular consumption of alcohol and the administration of benzodiazepines was related to poorer sleep quality. In this regard, consideration would be required of how to limit the use of benzodiazepines25, with the possibility of replacing them with other drugs such as α2-adrenergic agonists, in patients that may stand to benefit from such measures. In this regard, the literature associates their administration to an electroencephalographic pattern more consistent with that of natural sleep in comparison with benzodiazepine use, and to a lesser incidence of delirium26,27.
A negative correlation was found on exploring the relationship between comorbidity and sleep quality in the ICU, with poorer sleep quality being related to an increased number of comorbidities. Similar data have been reported by Lewandowska22. Lastly, an inadequate temperature in the room also proved significant, though not so patient location in any concrete place within the Department.
Despite the many studies on sleep quality in the ICU, this remains an unresolved issue, due to its multifactorial nature. In this respect, the clinical practice guides on the management of sedoanalgesia in adult critical patients suggest – with a strong grade of recommendation – that the adoption of non-pharmacological measures, such as reducing nocturnal noise and adjusting light exposure, reduces the fragmentation of sleep and affords greater sleep quality. This in turn allows for a lesser use of sedatives such as benzodiazepines, and thus the avoidance of oversedation25,28.
It is important to adopt the recommendations of the guides, since the lack of sleep extends beyond the ICU, and patients continue to experience sleep disturbances and drowsiness at the time of discharge from hospital. The studies reveal a prevalence of altered sleep of 50–66.7% (1 month), 34–64.3% (1–3 months), 22–57% (3–6 months) and 10–61% (6 months) after hospital discharge, following critical illness29–32.
Study limitationsEvaluation based on questionnaires is admittedly subjective and can only replace the use of objective tools when the latter cannot be used. Another possible limitation of our study was the fact that no objective measurement was made of the levels of noise or light exposure.
ConclusionsPatients admitted to the ICU experience significantly worsened sleep quality during their stay in the Unit. Light exposure, noise (e.g., alarms, hearing people speaking), nebulizations and certain nursing activities such as the extraction of samples or the administration of medications, were the most annoying factors. Patient age, the regular consumption of alcohol, the administration of benzodiazepines in the ICU, and increased comorbidity also exerted a negative impact. Measures designed to reduce the modifiable factors could help to improve the sleep quality of our patients.
Authorship/collaboratorsAll the authors contributed to conception of the study, data collection, analysis of the results and the design of the manuscript, and approved its final version.
Financial supportThis study received no financial support.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Bernat Adell MD, Galarza Barrachina L, Bisbal Andrés E, Cebrián Graullera G, Pagés Aznar G, Morán Marmaneu MÁ, et al. Factores que afectan a la calidad del sueño en las unidades de cuidados intensivos. Med Intensiva. 2021;45:470–476.