Analyzing associated factors with vasoplegic shock in the postoperative period of Cardiac Surgery. Analyzing the influence of vasopressin as rescue therapy to first-line treatment with norepinephrine.
DesignCohort, prospective and observational study.
SettingMain hospital Postoperative Cardiac ICU.
PatientsPatients undergoing cardiac surgery with subsequent ICU admission from January 2021 to December 2022.
InterventionsRecord of presurgical, perioperative and ICU discharge clinical variables.
Main variables of interestchronic treatment, presence of vasoplegic shock, need for vasopressin, cardiopulmonary bypass time, mortality.
Results773 patients met the inclusion criteria. The average age was 67.3, with predominance of males (65.7%). Post-CPB vasoplegia was documented in 94 patients (12.2%). In multivariate analysis, vasoplegia was associated with age, female sex, presurgical creatinine levels, cardiopulmonary bypass time, lactate level upon admission to the ICU, and need for prothrombin complex transfusion. Of the patients who developed vasoplegia, 18 (19%) required rescue vasopressin, associated with pre-surgical intake of ACEIs/ARBs, worse Euroscore score and longer cardiopulmonary bypass time. Refractory vasoplegia with vasopressin requirement was associated with increased morbidity and mortality.
ConclusionsPostcardiopulmonary bypass vasoplegia is associated with increased mortality and morbidity. Shortening cardiopulmonary bypass times and minimizing products blood transfusion could reduce its development. Removing ACEIs and ARBs prior to surgery could reduce the incidence of refractory vasoplegia requiring rescue with vasopressin. The first-line treatment is norepinephrine and rescue treatment with VSP is a good choice in refractory situations. The first-line treatment of this syndrome is norepinephrine, although rescue with vasopressin is a good complement in refractory situations.
Analizar los factores asociados al shock vasopléjico en el postoperatorio de Cirugía Cardiaca. Analizar la influencia de la vasopresina como terapia de rescate al tratamiento de primera línea con noradrenalina.
DiseñoEstudio de cohortes, prospectivo y observacional.
ÁmbitoUCI de Postoperatorio Cardiaco de hospital de tercer nivel.
PacientesPacientes sometidos a cirugía cardiaca con ingreso posterior en UCI desde enero de 2021 hasta diciembre de 2022.
IntervencionesRegistro de variables clínicas prequirúrgicas, perioperatorias y al alta de UCI.
Variables de interés principalsTratamiento crónico, presencia de shock vasopléjico, necesidad de vasopresina, tiempo de circulación extracorpórea, mortalidad.
Resultados773 pacientes cumplieron los criterios de inclusión. La edad media fue 67,3 años, predominio del sexo masculino (65,7%). Se documentó vasoplejia postCEC en 94 pacientes (12,2%). La vasoplejia se asoció independientemente con edad, sexo femenino, creatinina prequirúrgica, tiempo de circulación extracorpórea, lactato al ingreso en UCI y necesidad de complejo protrombínico. De los pacientes que desarrollaron vasoplejia, 18 (19%) precisaron vasopresina de rescate, asociándose con la toma prequirúrgica de IECAs/ARAII, peor Euroscore y mayor tiempo de circulación extracorpórea. La vasoplejia refractaria con necesidad de vasopresina se asoció a aumento de morbimortalidad.
ConclusionesLa vasoplejia post-circulación extracorpórea se asocia a aumento de morimortalidad. Acortar tiempos de circulación extracorpórea y minimizar necesidades trasfusionales podrían disminuir su desarrollo. Retirar IECAS y ARAII previa a la cirugía podría reducir la incidencia de vasoplejia refractaria con necesidad de rescate con vasopresina. El tratamiento de primera línea de este síndrome es la noradrenalina, si bien, el rescate con vasopresina es un buen complemento en situaciones de refractariedad.
Although extracorporeal circulation (ECC) has revolutioned cardiac surgery, its use is no stranger to vascular (large vessel ruptures and/or dissections), embolic, hemorrhagic (related to anticoagulation), and hemodynamic complications.
Regarding the latter, vasoplegic shock during the immediate postoperative care stands out, defined as systemic arterial hypotension (mean arterial pressure—MAP—<65mmHg) due to intense vasodilation with loss of systemic vascular resistance (SVR<800dyness/cm2), and a normal or elevated cardiac index (CI>2.2L/min/m2). It is characterized by an inappropriate response to usual doses of vasopressor drugs, occurring between 5% and 25%, and associated with a high mortality rate.1,2
The mechanisms involved are multifactorial and not entirely known, mainly mediated by a disproportionate immune response: release of proinflammatory mediators, complement activation due to surgical aggression, ischemia-reperfusion injury to the heart and lungs, polytransfusion, or blood exposure to exogenous material in the ECC circuit.1 These factors promote an increase in oxygen-free radicals, endothelins, nitric oxide (NO), platelet activation factors, thromboxane A2, prostaglandins, and cytokines.3 All of these lead to intense systemic arterial vasodilation, participating in the development of the systemic inflammatory response syndrome (SIRS), which intensifies such vasodilation.1,2 Additionally, this situation triggers a relative decrease in plasma levels of arginine-vasopressin, due to the depletion of the neurohypophyseal vasopressin reserve and an initial release due to the stress caused by the duration of ECC, along with a relative deficit of cortisol and dysfunction of the renin-angiotensin axis.3 This dysfunction is due to decreased production of angiotensin-2 by exclusion of the pulmonary circulation during ECC, thus precipitating vasoplegia.5
Parallel to the activation of the aforementioned vasodilatory mechanisms, there is resistance to vasoactive drugs and molecules, especially amines, due to inactivation of cytoplasmic calcium channels.3
The combination of these biochemical and cellular processes generates intense systemic vasodilation, clinically manifested as distributive shock with severe arterial hypotension.
The treatment of this condition has traditionally been based on vasoactive amines (norepinephrine (NAD) or adrenaline), which have a narrow therapeutic margin and are associated with cardiovascular adverse events (arrhythmias and myocardial ischemia) with incidence rates close to 50%.6 Furthermore, during the course of vasoplegic shock, smooth muscle cells present in the blood vessels acquire resistance to amines (mainly NAD) through complex mechanisms (activation of potassium channels, increased synthesis of NO, desensitization of adrenoreceptors, and relative deficiency of vasopressin and corticosteroids.5,7 In this regard, arginine vasopressin (AVP), a physiological vasopressor hormone, has been proposed as a bailout therapy for in this type of shock.
The objective of our study is to describe the factors associated with the occurrence of post-ECC vasoplegic shock and the impact that the development of refractory vasoplegia and the need for bailout vasopressin has on morbidity and mortality.
Patients and methodsWe conducted a retrospective and observational cohort study with successive patients undergoing cardiac surgery at Hospital Miguel Servet, Zaragoza, Spain treated in the intensive care unit from January 1, 2021 through December 31, 2022. The study was approved by the Research Ethics Committee of the Autonomous Community of Aragon. The follow-up period covered the duration of the immediate postoperative care period at the ICU until the discharge date to the hospitalization ward or death date.
Patients older than 18 years old undergoing elective or emergency cardiac surgery (valvular, coronary, aortic) were included (those in whom the indication for surgery occurred during admission). Patients who died within the first 24h after surgery, emergency surgery, or due to endocarditis (including cardiac transplantation and aortic dissection) and surgery without ECC were excluded.
Demographic data, comorbidities, chronic therapies used, Euroscore (European System for Cardiac Operative Risk Evaluation), ECC time, ischemia time, use of blood products, the length of ICU stay, need for treatment with vasoactive drugs (VAD), or support with ventricular assist devices, and pre- and postoperative analytical data were recorded for each patient. Furthermore, complications during admission were recorded: development of cardiac arrhythmias, acute kidney failure, need for mechanical ventilation (MV) for > 48h, presence of nosocomial infections, polytransfusion, need for reintervention, surgical wound infection, and death. Acute and acute-on-chronic kidney failure were defined in full compliance with criteria of the Acute Kidney Injury Network (AKIN).10 Furthermore, patients were categorized into those with kidney failure without need for renal replacement therapy (RRT) and those who actually did. Neurological complication was defined as the occurrence of postoperative neurological focal deficits or persistent coma or stupor and/or presence of seizures. Infectious complications were defined using the criteria established by ENVIN-HELICS.11 Postoperative respiratory failure was defined as respiratory failure due to postoperative complications that required ICU admission or prolonged ICU stays with ventilatory support (whether invasive and/or non-invasive). Postoperative acute hepatic dysfunction was defined as doubling of the upper normal limit of transaminases associated with evidence of liver failure (jaundice and/or coagulopathy) in a patient without chronic liver disease. Paralytic ileus was defined as decreased GI motility 48h after surgery, preventing the introduction of enteral nutrition, and mesenteric ischemia as a reduced blood flow to the intestines, whether abruptly or progressively. ICU mortality beyond the first 24h after admission was recorded as well.
The state of shock immediately after surgery shock was categorized as follows:
- 1
Vasoplegic shock: systemic arterial hypotension (MAP<65mmHg) due to intense vasodilation, with SVR (<800dyness/cm5) and normal or elevated CI (>2.2L/min/m2) in the absence of acute cardiac dysfunction and active infection, characterized by an inadequate (reduced) response to standard doses of vasopressor drugs. Refractory dose of vasopressor drug was defined as an infusion of NAD>0.5μg/kg/min of NAD base; equivalent to 1μg/kg/min of NAD bitartrate, initiating the gradual infusion of VSP doses with up-titration of 0.01−0.02IU/h up to a maximum dose of 2IU/h, according to hemodynamic response.
- 2
Post-cardiotomy cardiogenic shock, defined as acute heart failure, with decreased cardiac output (CO) resulting in tissue hypoperfusion, with CI<2L/min/m2, systolic blood pressure (SBP) < 90mmHg, and SVR within normal values. It includes uni- or biventricular cardiac dysfunction, perioperative acute myocardial infarction (AMI), and acute valvular dysfunction.12
In the descriptive analysis, continuous variables were expressed as mean±standard deviation, median and interquartile range, and the categorical ones as absolute value of cases and percentage. Kolmogorov–Smirnov normality contrast test was used too.
In the inferential analysis, for comparison of means, the Student's t-test or one-way ANOVA was used to compared more than 2 groups, while the comparative analysis of proportions was conducted using the chi-square test. Yates correction or Fisher's exact test were used, when necessary.
We performed a multivariate analysis through binary logistic regression. In the binary logistic regression analysis, variables that were associated with the occurrence of vasoplegia in the univariate analysis and those considered of clinical interest were included. P values <.05 were considered statistically significant. Statistical analysis was performed using the SPSS version 20 statistical software package.
ResultsFrom January 1, 2021, to December 31, 2022, 3631 patients were treated in the Intensive Care Unit (ICU) of Hospital Universitario Miguel Servet, of which 895 cases (24.6%) required cardiac surgery. Of these, 122 patients were excluded from the analysis for not meeting inclusion criteria (Fig. 1).
A total of 773 patients were included in the study, with a median age of 70 years [62–75] and a predominance of male patients (65.7%). It was a population with multiple cardiovascular risk factors (Table 1), highlighting the presence of preoperative pulmonary hypertension (PHT) in 35.6% of the analyzed population.
Demographic. Epidemiological, comorbidities, and chronic treatment data.
| Total | Vasoplegia | P | |||||
|---|---|---|---|---|---|---|---|
| N=773 | Yes (n=94) | No (n=679) | |||||
| n | % | n | % | n | % | ||
| Age (Mean±SD) | 67.3±10.9 | 69.8±8.9 | 66.0±11.0 | .001 | |||
| Sex: | |||||||
| Woman | 265 | 34.30% | 31.80% | .000 | |||
| Past medical history | |||||||
| AHT | 531 | 68.70% | 69 | 73.40% | 462 | 68.00% | ns |
| Dyslipidemia | 493 | 63.80% | 54 | 57.40% | 439 | 64.70% | ns |
| Diabetes mellitus | 234 | 30.30% | 28 | 29.80% | 206 | 30.30% | ns |
| Smoking | 326 | 42.20% | 34 | 36.20% | 292 | 43.00% | ns |
| CKD | 133 | 17.20% | 15 | 16.0% | 118 | 17.40% | ns |
| Ejection fraction: | ns | ||||||
| +EF < 50% | 133 | 17.20% | 16 | 17.0% | 117 | 17.20% | |
| Postoperative PHT | 278 | 36.00% | 49 | 52.10% | 229 | 33.70% | .000 |
| Previous therapy | |||||||
| ACEIs/ARBs II | 473 | 61.20% | 51 | 54.20% | 422 | 62.20% | ns |
| Beta-blockers | 412 | 53.30% | 49 | 52.10% | 363 | 53.50% | ns |
| Statins | 435 | 56.30% | 52 | 55.30% | 383 | 56.40% | ns |
| Calcium antagonists | 148 | 19.10% | 23 | 24.50% | 125 | 18.40% | ns |
| Aldosterone antagonists | 133 | 17.20% | 18 | 19.10% | 115 | 16.90% | ns |
| Sacubitril valsartan | 19 | 2.60% | 1 | 1.10% | 19 | 2.80% | ns |
| SGLT2 inhibitors | 97 | 12.50% | 13 | 13.80% | 84 | 12.40% | ns |
| Sildenafil | 13 | 1.70% | 1 | 1.10% | 12 | 1.80% | ns |
| Microbiological history | |||||||
| MRSA detection | 17 | 2.20% | 5 | 5.30% | 12 | 1.80% | .028 |
| Type of surgery | |||||||
| Isolated or combined aortic valve repair (valve and/or coronary artery) | 72 | 9.70% | 6 | 6.40% | 66 | 9.70% | .022 |
| Isolated or combined aortic valve repaira | 518 | 67.00% | 75 | 79.80% | 443 | 65.20% | |
| Isolated coronary artery repaira | 168 | 21.70% | 11 | 11.70% | 157 | 23.10% | |
| Other | 15 | 1.90% | 2 | 2.10% | 13 | 1.90% | |
AHT, arterial hypertension; CKD, chronic kidney disease; EF, ejection fraction; MRSA, methicillin-resistant Staphylococcus aureus; PHT, pulmonary hypertension.
Post-ECC vasoplegia was documented in 12.2% of the cases (94 patients), with a predominance of female patients (P<.0001), an older population (P=.001), type of surgery (P=.022), and with the presence of preoperative PHT (P<.0001), as well as in the subgroup of patients where methicillin-resistant Staphylococcus aureus (MRSA) was detected in the preoperative epidemiological control swab (P=.028) (Table 1).
The occurrence of vasoplegia was associated with a greater need for platelet transfusion (P=.001), fresh frozen plasma (P=.001), fibrinogen (P=.003), and prothrombin complex (P<.0001) (Table 2).
Perioperative data.
| Total | Vasoplegia | P | |||||
|---|---|---|---|---|---|---|---|
| N=773 | YES (n=94) | No (n=679) | |||||
| Mean | SD | Mean | SD | Mean | SD | ||
| Total EuroScore | 2.56 | 2.58 | 2.96 | 2.12 | 2.5 | 2.64 | ns |
| Preoperative BP (mmHg) | 124 | 16 | 119 | 14 | 125 | 16 | .001 |
| Preoperative creatinine levels (mg/dL) | 1.09 | 0.67 | 1.18 | 0.6 | 1.07 | 0.68 | ns |
| Preoperative hematocrit (%) | 41 | 5.1 | 40.3 | 5.3 | 41.1 | 5.1 | ns |
| ECC time (min) | 101 | 36 | 117 | 39 | 99 | 35 | .000 |
| Ischemia time (min) | 73 | 30 | 82 | 33 | 72 | 29 | .006 |
| Platelet at the ICU admission (x nL) | 149 | 71 | 173 | 76 | 146 | 70 | .000 |
| Hemoglobin at the ICU admission (g/dL) | 10.3 | 1.4 | 9.5 | 1 | 10.4 | 1.4 | .000 |
| Fibrinogen at the ICU admission (g/L) | 2.2 | 2.9 | 2.2 | 2.9 | 2.2 | 2.9 | ns |
| Lactic acid at the ICU admission (mmol/L) | 1.8 | 0.9 | 2.2 | 1.5 | 1.7 | 0.8 | .001 |
| Transfusion needs | |||||||
| Red blood cells (no. of concentrates) | 152 | 19.70% | 23 | 24.50% | 129 | 19.00% | ns |
| Platelets (pool no.) | 398 | 51.50% | 63 | 67.00% | 335 | 49.30% | .001 |
| Fibrinogen (g) | 229 | 29.60% | 40 | 42.60% | 189 | 27.80% | .003 |
| Prothrombin complex | 188 | 24.3% | 40 | 42.6% | 148 | 21.8% | .000 |
| Frozen fresh plasma (n | 8 | 1.00% | 4 | 4.30% | 4 | 0.60% | .001 |
| Factor VIIa | 11 | 1.40% | 2 | 2.10% | 9 | 1.30% | ns |
Binary logistic regression analysis showed a statistically independent positive association with age (OR, 1.036; 95%CI, 1.008–1.064; P=.010), female gender (OR, 2.56; 95%CI, 1.569–4.179; P<.0001), preoperative creatinine levels (OR, 1.388; 95%CI, 1.019–1.893; P=.038), ECC times (OR, 1.009; 95%CI, 1.003–1.016; P=.007), lactic acid level upon ICU admission (OR, 1.33; 95%CI, 1.069–1.654; P=.010), and the need for prothrombin complex transfusion during surgery (OR, 1.733; 95%CI, 1.013–2.963; P=.045). On the other hand, higher preoperative systolic blood pressure values acted as an independent protective factor (OR, 0.975; 95%CI, 0.961–0.990; P=.001) (Table 3).
Variables with an independent association with post-ECC vasoplegia.
| OR | 95%CI | P | ||
|---|---|---|---|---|
| Age | 1036 | 1008 | 1064 | .01 |
| Sex (woman) | 256 | 1569 | 4179 | .000 |
| Preoperative BP | 0975 | 0961 | 099 | .001 |
| Preoperative creatinine | 1388 | 1019 | 1893 | .038 |
| EC time | 1009 | 1003 | 1016 | .007 |
| Lactic acid at the ICU admission | 133 | 1069 | 1654 | .01 |
| Prothrombin complex transfusion | 1733 | 1013 | 2963 | .045 |
Variables introduced: age, gender, total EuroScore, preoperative blood pressure, preoperative creatinine, preoperative hematocrit, ECC time, ischemia time, lactic acid at the ICU admission, preoperative pulmonary arterial hypertension (PAH), ejection fraction < 50%, platelet transfusion requirement, fibrinogen transfusion requirement, prothrombin complex requirement, MRSA detection, type of surgery.
Similarly, the occurrence of vasoplegia was associated with higher rates of medical and surgical complications after admission to the ICU (Table 4).
Medical and surgical complications at the ICU admission.
| Total | Vasoplegia | P | |||||
|---|---|---|---|---|---|---|---|
| N=773 | Yes (n=94) | No (n=679) | |||||
| n | % | n | % | n | % | ||
| Acute kidney injury | 146 | 18.90% | 35 | 37.20% | 111 | 16.30% | .000 |
| Exacerbated CKD | 65 | 8.40% | 15 | 16.00% | 50 | 7.40% | .005 |
| Reintervention | 22 | 2.80% | 9 | 9.60% | 13 | 1.90% | .000 |
| Bacteremia | 7 | 0.90% | 5 | 5.30% | 2 | 0.30% | .000 |
| MV-associated pneumonia | 8 | 1.00% | 7 | 7.40% | 1 | 0.10% | .000 |
| Surgical site infection | 2 | 0.30% | 0 | 0.00% | 2 | 0.30% | ns |
| Mesenteric ischemia | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | ns |
| Postoperative ileum | 14 | 1.80% | 5 | 5.30% | 9 | 1.30% | .007 |
| Multi-drug resistant colonization | 15 | 1.90% | 6 | 6.40% | 9 | 1.30% | .001 |
| Multi-drug resistant infection | 1 | 0.10% | 1 | 1.10% | 0 | 0.00% | .007 |
| Neurological complications | 26 | 3.40% | 9 | 9.60% | 17 | 2.50% | .000 |
| Respiratory infection | 57 | 7.40% | 13 | 13.80% | 44 | 6.50% | .011 |
| Liver failure | 3 | 0.40% | 2 | 2.10% | 1 | 0.10% | .004 |
| Death | 19 | 2.50% | 10 | 10.60% | 9 | 1.30% | .000 |
| Need for vasoactive support and blue methylene | |||||||
| Noradrenaline | 461 | 59.60% | 94 | 100% | 368 | 54.20% | .000 |
| Dobutamine | 626 | 81.00% | 81 | 86.20% | 545 | 80.30% | Ns |
| Vasopressin | 23 | 3.00% | 18 | 19.10% | 5 | 0.70% | .000 |
| Blue methylene | 3 | 0.40% | 3 | 3.20% | 0 | 0.00% | .002 |
| Need for renal replacement therapy (RRT) and VA-ECMO | |||||||
| RRT | 15 | 1.90% | 8 | 8.50% | 7 | 1.00% | .000 |
| VA-ECMO | 3 | 0.40% | 2 | 2.10% | 1 | 0.10% | .004 |
| Time on MV (hours) | Median | Median | Median | .004 | |||
| 5.9 [4.3−8.2] | 7.2 [5.0−13.0] | 5.8 [4.3−7.9] | |||||
| Length of ICU stay (days) | Mean | SD | Mean | SD | Mean | SD | .000 |
| 5.15 | 10.3 | 10.97 | 15.6 | 4.35 | 9.06 | ||
| Mortality | n | % | n | % | n | % | |
| 19 | 2.50% | 10 | 10.60% | 9 | 1.30% | .000 | |
AHT, arterial hypertension; CKD, chronic kidney disease; MV, mechanical ventilation; RRT, renal replacement therapy; VA-ECMO, veno-arterial extracorporeal membrane oxygenation.
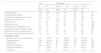
Regarding the group of patients who developed vasoplegia (n=94), 18 of them required the administration of VSP as bailout therapy in the immediate postoperative period, with a statistically significant association with the use of ACEIs, aldosterone antagonists, and SGLT2i prior to surgical intervention. Additionally, these patients had worse EuroScore scores (P=.017), longer ECC times (P=.011), and higher lactic acid levels upon the ICU admission (P<.0001). Finally, patients who experienced refractory vasoplegia and required bailout VSP exhibited more complications, the intraoperative transfusion of blood products, consumption of technical resources, longer ICU stays and higher mortality rates (44.4% vs 2.6%; P<.0001) (Table 5).
Patients with post-ECC vasoplegic shock. Factors associated with and increased severity and need for VSP therapy. Prognosis of post-ECC vasoplegia.
| Preoperative clinical variables | Total (Vasoplegia) | Vasopressin | P | ||||
|---|---|---|---|---|---|---|---|
| N=94 | Yes (n=18) | No (n=76) | |||||
| Age (Mean±SD) | 69.8±8.9 | 71.7±5.4 | 69.4±9.5 | ns | |||
| n | % | n | % | n | % | ||
| Woman | 49 | 52.10% | 8 | 44.40% | 41 | 53.90% | ns |
| Past medical history | |||||||
| AHT | 69 | 73.40% | 13 | 72.20% | 56 | 73.70% | ns |
| Dyslipidemia | 54 | 57.40% | 9 | 50.00% | 45 | 59.20% | ns |
| Diabetes mellitus | 28 | 29.80% | 5 | 27.80% | 23 | 30.30% | ns |
| Smoking | 34 | 36.20% | 9 | 50.00% | 25 | 32.90% | ns |
| CKD | 15 | 16.00% | 1 | 5.60% | 14 | 18.40% | ns |
| EF: | ns | ||||||
| +EF < 50% | 16 | 17.10% | 3 | 16.70% | 12 | 15.80% | |
| Preoperative PHt | 49 | 52.10% | 8 | 44.40% | 41 | 53.90% | ns |
| Previous therapy | |||||||
| ACEIs / ARBs II | 51 | 54.20% | 5 | 27.80% | 46 | 60.50% | .012 |
| Beta-blockers | 49 | 52.10% | 6 | 33.30% | 43 | 56.50% | ns |
| Statins | 52 | 55.30% | 8 | 44.40% | 44 | 57.90% | ns |
| Calcium antagonists | 23 | 24.50% | 4 | 22.20% | 19 | 25% | ns |
| aldosterone antagonists | 18 | 19.10% | 0 | 0.00% | 18 | 23.70% | .023 |
| Sacubitril Valsartan | 1 | 1.10% | 0 | 0.00% | 1 | 1.40% | ns |
| SGLT2 inhibitors | 13 | 13.80% | 5 | 27.80% | 8 | 10.50% | .048 |
| Sildenafil | 1 | 1.10% | 0 | 0.00% | 1 | 1.40% | ns |
| Microbiological history | |||||||
| MRSA detection | 5 | 5.30% | 1 | 5.60% | 4 | 5.30% | ns |
| Perioperative variables | Mean | SD | Mean | SD | Mean | SD | P |
| EuroScore | 2.96 | 2.12 | 4.02 | 2.41 | 2.71 | 1.98 | .017 |
| Preoperative BP (mmHg) | 119 | 14 | 115 | 12 | 120 | 14 | ns |
| Preoperative creatinine (mg/dL) | 1.18 | 0.6 | 1.42 | 0.87 | 1.13 | 0.51 | |
| Preoperative hematocrit (%) | 40.3 | 5.3 | 40.8 | 5.2 | 40.2 | 5.3 | ns |
| EC time (min) | 117 | 39 | 142 | 46 | 110 | 34 | .011 |
| Ischemia time (min) | 82 | 33 | 96 | 46 | 79 | 29 | ns |
| Platelet at the ICU admission (x nL) | 173 | 76 | 175 | 93 | 173 | 72 | ns |
| Hemoglobin at the ICU admission (g/dL) | 9.5 | 1 | 9.2 | 1.2 | 9.6 | 0.9 | ns |
| Fibrinogen at the ICU admission (g/L) | 2.2 | 2.9 | 3 | 2.7 | 2 | 2.9 | ns |
| Lactic acid at the ICU admission (mmol/L) | 2.2 | 1.5 | 3.6 | 2.7 | 1.9 | 0.8 | <.001 |
| Need for the intraoperative transfusion of hemoderivatives | n | % | n | % | n | % | P |
| Red blood cells | 23 | 25.5 | 8 | 44.4 | 15 | 19.7 | .028 |
| Platelets | 63 | 67.0 | 16 | 88.9 | 47 | 61.8 | .028 |
| Fibrinogen | 40 | 42.6 | 9 | 50 | 31 | 40.8 | Ns |
| Prothrombin complex | 40 | 42.60% | 13 | 72.20% | 27 | 35.5 | .005 |
| Frozen fresh plasma | 4 | 4.3 | 2 | 11.1 | 2 | 2.6 | ns |
| Factor VIIa | 2 | 2.1 | 1 | 5.6 | 1 | 1.3 | ns |
| Complications during the ICU stay | n | % | n | % | n | % | P |
| Acute kidney injury | 35 | 37.2% | 10 | 55.6% | 25 | 32.9% | ns |
| Exacerbated CKD | 15 | 16.0% | 6 | 33.3% | 9 | 11.8% | .025 |
| Reintervention | 9 | 9.6% | 6 | 33.3% | 3 | 3.9% | <.001 |
| Bacteremia | 5 | 5.3% | 2 | 11.1% | 3 | 3.9% | Ns |
| MV-associated pneumonia | 7 | 7.4% | 5 | 27.8% | 2 | 2.6% | <.001 |
| Surgical site infection | 94 | 100% | 18 | 100% | 76 | 100% | Ns |
| Postoperative ileum | 5 | 5.3% | 1 | 5.6% | 4 | 5.3% | Ns |
| Mesenteric ischemia | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | Ns |
| Multi-drug resistant colonization | 6 | 6.4% | 1 | 5.6% | 5 | 6.6% | Ns |
| Multi-drug resistant infection | 1 | 1.1% | 0 | 0.0% | 1 | 1.3% | Ns |
| Neurologic complications | 9 | 9.6% | 5 | 27.8% | 4 | 5.3% | .004 |
| Respiratory distress | 13 | 13.8% | 5 | 27.8% | 8 | 10.5% | Ns |
| Liver failure | 2 | 2.1% | 2 | 11.1% | 0 | 0.0% | .003 |
| Need for RRT, VA-ECMO | n | % | n | % | n | % | P |
| RRT | 8 | 8.5% | 5 | 27.5% | 3 | 3.9% | .001 |
| VA-ECMO | 2 | 2.1% | 1 | 5.6% | 1 | 1.3% | ns |
| Time on MV (hours) | Median | Median | Median | ||||
| 7.2 [5.0−13.0] | 54.9 [23.8−251.0] | 6.1 [4.6−9.0] | <.001 | ||||
| Length of ICU stay (days) | Mean | SD | Mean | SD | Mean | SD | P |
| 10.97 | 15.6 | 19.49 | 19.43 | 8.95 | 13.95 | .009 | |
| Mortality | n | % | n | % | n | % | P |
| 10 | 10.6% | 8 | 44.4% | 2 | 2.6% | <.001 | |
AHT, arterial hypertension; CKD, chronic kidney disease; EF, ejection fraction; MV, mechanical ventilation; RRT, renal replacement therapy; VA-ECMO, veno-arterial extracorporeal membrane oxygenation.
Post-ECC vasoplegia is a serious and frequent condition, with incidence rates ranging from 5% up to 25%,2,3,13,14 reaching up to 44% in some series,3,15,16 and associated with high mortality (25%–50%).1,17 In our series, the detected prevalence is 12.2%, associated with a lower overall mortality than the one documented in other series (10.6%).
The medical literature identifies multiple risk factors related to this condition, such as male sex,4,13,15,18 advanced age,2,3,13,18 higher EuroScore scores,18 preoperative use of ACEIs,5,19 or extended ECC times. Our data are consistent with those published regarding age, having shown an independent association.
Regarding sex, however, we saw a predominance in females, behaving as an independent predictor for the development of vasoplegia. This is consistent with that published by Mesa et al.20
In our study, no statistically significant association was seen between the development of vasoplegia and the EuroScore score. However, the subgroup of patients with vasoplegia who received treatment with VSP had higher scores with a statistically significant association. This scale provides a simple assessment of perioperative mortality risk in cardiac surgery.21 In the medical literature, EuroScore has been related to vasoplegia in univariate analyses, with the statistical significance disappearing in the multivariate analyses.13,14 In this work, it was included in the multivariate analysis without observing statistical significance; therefore, we cannot consider it an adequate predictor of postoperative vasoplegia.
Regarding perioperative drug treatment, the meta-analysis conducted by Noubiac et al.22 of 10 observational case-control studies showed that the use of ACEIs and ARBs poses an independent risk factor for the development of post-ECC vasoplegia. However, our results do not reveal such a relationship. They have even been considered a protective factor vs the development of NAD refractory vasoplegia in the group of patients who developed it. This finding might seem paradoxical at first glance; however, it should be noted that patients categorized as chronic users of ACEIs and/or ARBs II discontinued the drug within the 48h prior to the intervention to prevent this condition, as recommended by some authors.15 The abrupt withdrawal of ACEIs and/or ARBs II leads to a rapid elevation of blood pressure within the first few days.23,24 This phenomenon could justify our results, where higher preoperative systolic blood pressure values constituted an independent protective factor for the development of post-ECC vasoplegia, as reflected in the cumulative evidence.2,15,25 Therefore, chronic users of ACEIs/ARBs II may experience a reflex elevation of their blood pressure values upon discontinuation of treatment, resulting in a lower incidence of vasoplegia. We have not found in the literature ANY studies whose design takes this measure into account in the incidence of post-ECC vasoplegia.
PHT is an independent risk factor for mortality in cardiac surgery.26 It is included in various surgical risk prediction models (including the Euroscore21) as one of the most significant factors for the occurrence of postoperative vasoplegia.20 A study published in 2018 found that numerous variables related to pulmonary hemodynamics (pressure in the pulmonary artery trunk, pressure in the right atrium, pulmonary vascular resistance), when increased preoperatively, were related to the postoperative occurrence of vasoplegia. In our study, the presence of preoperative PHT has been associated with the development of vasoplegia.
The duration of ECC is one of the factors most widely associated with this condition.13,15 ECC induces the release of inflammatory mediators (cytokines, interleukins) that predispose to the development of vasoplegia, and additionally, it excludes pulmonary circulation. This results in a decreased catabolism of vasodilatory molecules, such as bradykinin, which is synthesized in the pulmonary alveoli. Consequently, there is a plasma increase of vasodilatory components followed by a decrease in vasoconstrictive components, disrupting the natural balance of vasomotor tone.16
In our population, longer surgical times (both ECC time and ischemia time) have been associated with the onset of vasoplegia and the need for bailout VSP in the group of patients with vasoplegia. There was a statistically significant association with the type of surgery, but it disappeared in the logistic regression analysis, justified by the greater importance of ECC time in more complex surgeries.
Regarding intraoperative and immediate postoperative factors at the ICU setting, we have found that lower hemoglobin levels are associated with a higher risk of vasoplegia, which has been previously described in some studies. Additionally, the meta-analysis conducted by Dayan et al.15 concludes that both intraoperative hemorrhage and/or hemorrhagic shock, as well as the transfusion of plasma components have been associated with post-ECC vasoplegic shock. Such data are reinforced by our findings, as we have demonstrated that the need for prothrombin complex transfusion during surgical intervention has proven to be an independent risk factor for the development of post-ECC vasoplegia. Both the nature of the components of the prothrombin complex and the situations of massive bleeding in which its administration is indicated can trigger an inflammatory response and consequently, vasoplegic shock.
There are no solid recommendations to guide the management of post-ECC vasoplegia. Catecholamines are considered the first-line therapy. NAD has alpha-1 effects with direct action on vascular tone. Among its side effects are arrhythmic and ischemic events at myocardial and other organ levels; however, these are dose-dependent. Its safety profile is well-known, being safe at low doses (<0.3μg/kg/min). Recent studies support the use of VSP5 or agents such as methylene blue, hydroxocobalamin, corticosteroids, or angiotensin II.27 Among them, VSP has demonstrated its efficacy in significant works, being used as a bailout therapy to treat distributive shock.5,6 In the context of post-ECC vasoplegic shock, its use aims to reverse the loss of vascular tone in patients undergoing cardiac surgery who remain unresponsive to the usual therapeutic measures.4,28 Observational studies describe the beneficial hemodynamic effects of VSP at low doses in patients with post-cardiotomy shock.29–31
In the VANCS controlled trial,5 patients with post-ECC vasoplegic shock were randomized into 2 groups to receive either NAD or VSP (both drugs as monotherapy). Therefore, the effect of the standard of care for this condition could not be evaluated: initial NAD and addition of bailout VSP (which is the clearest and most common indication for VSP in critically ill patients).32–34
Another interesting characteristic of VSP therapy in patients undergoing cardiac surgery is its neutral effect on myocardial oxygen consumption.5 The VANCS trial demonstrated that VSP does not induce an increased heart rate and is not associated either with an increased incidence of myocardial ischemia.5,8
VSP can cause ischemia and necrosis; however, this occurs at doses higher than its therapeutic range (>3.6IU/h).9,35 In fact, in our study, there were no serious ischemic complications in the VSP group at the doses used. However, the group of patients with refractory vasoplegia who needed bailout VSP showed higher morbidity rates and more complications vs patients whose vasoplegic shock could be controlled with low doses of NAD (<0.25μg/kg/min NAD base). In this regard, the refractory vasoplegia that prompted the use of VSP may have implied a higher degree of organ failure, which is the cause of the increased morbidity and mortality observed in this group.
One of the strengths of our study is that the hemodynamic profile of shock has been clearly defined, classifying post-ECC vasoplegia as patients in shock with normal or elevated cardiac output (determined by echocardiography and/or invasive hemodynamic monitoring) (CI>2.2L/min/m2), low systemic vascular resistances (SVR<800dyness/cm5), and no evidence of hypovolemia or active infection.
A major limitation in the published literature on the management of this condition lies in how post-ECC vasoplegia has traditionally been defined. Loose criteria have been used to determine the hemodynamic variables that define it, categorizing it as a nonspecific postoperative shock after a cardiac intervention with extracorporeal surgery.36 Consequently, the predominant type of shock (cardiogenic and/or vasoplegic) has often not been differentiated. The recent meta-analysis conducted by Noubiap et al. with more than 15000 recruited patients explicitly acknowledges the use of lax hemodynamic criteria to define post-ECC vasoplegic shock.22 This fact may have led to a variable degree of imprecision in the evaluation and comparison of vasoactive agents in the management of post-ECC vasoplegia. In other words, studies have been designed with molecules affecting vascular tone in shock scenarios with possible cardiogenic (and even hypovolemic) components, which could diminish the robustness of their results.
The therapeutic approach used in our work is consistent with the latest recommendations and expert consensus,37,38 advocating for the initiation of NAD and, in more severe cases, the addition of VSP. Furthermore, there is currently no recommendation on the threshold dose of NAD as the mark that jumpstarts VSP therapy, with this dose varying from 0.1μg/kg/min to 0.7μg/kg/min across the different studies that have analyzed this issue.38,39 Therefore, another strength of our study is that this threshold was pre-established at doses of 0.5μg/kg/min of NAD base.
The main limitation of this study is its observational design, thus demonstrating association rather than causality. The low number of patients requiring VSP, the single-center nature of the study, the lack of collection of intraoperative variables such as septal temperature, the composition and quantity of cardioplegic solution, or not classifying the “refractory” profile associated with the administration of NAD (requiring a rapid and exponential increase in its dose) vs the "controlled" profile (progressive increase in NAD until reaching a plateau without associated side effects)40 are other limitations of our study that should be considered in future studies.
ConclusionsPost-ECC vasoplegia is associated with a higher mortality rate and development of complications. Shortening ECC time and reducing transfusions could minimize the risk of vasoplegia. ACEIs/ARBs discontinuation medical prior to surgery could reduce the need for VSP.
Vasopressor support with low-dose NAD is still considered first-line therapy, being VSP a good addition in refractory situations instead of having to up-titrate NAD (NAD≥0.5μg/kg/min of basal NAD).
Authors’ contributionsAll authors declare that they have collaborated significantly in the design and development of this study, approved the submitted document, and taken responsibility for its contents.
Conflicts of interestNone declared.