Patient follow-up after intensive care unit (ICU) discharge allows the early recognition of complications associated to post-intensive care syndrome (PICS). The aim of this project is to standardize outcome variables in a follow-up program for patients at risk of suffering PICS.
MethodsThe Rehabilitation and Patient Follow-up Committee of the Argentine Society of Intensive Care Medicine (Sociedad Argentina de Terapia Intensiva, SATI) requested the collaboration of different committees to design the present document. A thorough search of the literature on the issue, together with pre-scheduled meetings and web-based discussion encounters were carried out. After comprehensive evaluation, the recommendations according to the GRADE system included in the follow-up program were: frequency of controlled visits, appointed healthcare professionals, basic domains of assessment and recommended tools of evaluation, validated in Spanish, and entire duration of the program.
ConclusionThe measures herein suggested for patient follow-up after ICU discharge will facilitate a basic approach to diagnosis and management of the long-term complications associated to PICS.
El seguimiento de pacientes al alta de la unidad de cuidados intensivos (UCI) permite el reconocimiento precoz de las complicaciones asociadas al síndrome post terapia intensiva (SPTI). El objetivo de este estudio es la estandarización de medidas básicas de resultado incluidas en un programa de seguimiento de pacientes en riesgo de presentar SPTI.
MétodosEl comité de Seguimiento y Rehabilitación luego de la Enfermedad Crítica de la Sociedad Argentina de Terapia Intensiva (SATI) convocó a diferentes comités para la redacción del presente documento. Se realizó una búsqueda bibliográfica, junto con reuniones y foros de discusión. Las recomendaciones incluidas en el programa de seguimiento según el sistema GRADE son: frecuencia de seguimiento, profesionales encargados del programa, dominios básicos a evaluar, herramientas recomendadas para su evaluación validadas al español y duración del programa.
ConclusiónLas medidas recomendadas para el seguimiento de pacientes permiten establecer los lineamientos básicos para la identificación y tratamiento precoz de las complicaciones asociadas al SPTI.
Over the last few years, the long-term consequences of critical disease have become more and more importance, due to the growing increase of life expectancy and the evolution of healthcare technologies that contribute to more patients being admitted to intensive care units (ICU) who survive the experience. These survivors suffer from important functional, psychological, and neurocognitive effects that have an impact on their health-related quality of life.1 These effects were called PICS, which stands for post-intensive care syndrome, at the Conference of the Medical Society of Critical Care held back in the year 2010.2 PICS develops quickly following the critical disease and it can last for up to 5 years3 or even more after the acute period of hospitalization. This syndrome affects both the patients who had the disease and their families, which has been referred to as family PICS,4 and is defined as the psychological consequences of the family member or care giver of a critically ill patient.
Below we can find a description of the areas most impacted by the PICS that can be classified as physical (functional), mental, and neurocognitive.
The physical complications after the ICU discharge are frequent and they can be classified as pulmonary and extrapulmonary, and they are maybe the main determinants, among other results, of the place of referral after the ICU discharge. In patients evaluated using pulmonary tests, a mild restrictive pattern was observed (that became normal 6 months after discharge) as well as the presence of an alteration in carbon monoxide diffusion, which improved over time, but it was not responsible for the fatigue patients exhibited.1
The most common extrapulmonary consequence is muscle weakness, associated with reduced muscle mass, strength and endurance. The study conducted by Hermans et al.5 it confirmed that ICU acquired weakness (ICUAW) was associated with less probability of weaning from mechanical ventilation (hazard ratio [HR], 0.709 [0.549–0.888]; P=.009), surviving the ICU (HR, 0.698 [0.553–0.861]; P=.008) and the hospital (HR, 0.680 [0.514–0.871]; P=.007) and higher mortality rate per year (30.6% vs. 17.2%; P=.015) compared to those who did not show muscle weakness. The risk of mortality per year was even greater if weakness was there even at ICU discharge (P=.001). Contracture-induced joint rigidity during the ICU stay is present in around 60% of the patients and it is a determinant factor in their capacity to walk independently after being discharged from hospital. Neuropathy entrapment, peripheral nerve damage, heterotopic ossifications, sexual dysfunction, dysphonia, voice changes, and cosmetic issues such as bed sores, transient alopecia, striations and scars are common complications that have an impact on the patient's functionality. They can be defined as the performance of Activities of Daily Living (ADL) of self-care and other Instrumental Activities of Daily Living (IADL) associated with autonomy, independence and competence. Chelluri et al.6 observed that, a year after discharge, most of these patients showed some degree of autonomy in their basic ADL and still greater autonomy in the IADL. Similar results are described in a follow-up study conducted in Argentina7 in which 51% of the patients still had some degree of dependence 3 months after leaving the ICU, while 33% were still dependent one year later.
Finally, coming back to work or prior activities fully is perhaps the most relevant functional determinant factor for a patient's life after ICU discharge. This result involves not only the patient's physical recovery, but also their full psychological and neurocognitive recovery. In the study conducted by Herridge et al.,1 only 49% of the patients came back to work within a year after ICU discharge; similar results were found in Argentina.6
On the other hand, acknowledging psychological disorders as symptoms of anxiety, depression, post-traumatic stress syndrome (PTSD)8 is crucial since all these disorders have a negative impact on health-related quality of life and they delay the come back to work. The presence of depression also increases the risk of suicide. Jones et al.9 described a large number of symptoms and psychological disorders in ICU survivors, such as anxiety, depression, guilt, fear of death, swinging moods, irritability, nightmares, agoraphobia, panic attacks, social isolation, etc. The symptoms of depression that occurred the year after ICU discharge are common,10 and they affect 28% (8%–57%) of the patients, a much higher incidence rate compared to the general population (7%–8%) and to those who suffered acute myocardial infarctions (14%) and maybe it is even greater since most studies excluded patients with a psychiatric history. The symptoms of anxiety occur in 24% (from 23 to 48%) of ICU survivors and PTSD in 22% (from 8 to 51%) of the critically ill patient populations. One in every 4 survivors will suffer from it, so its incidence rate is greater than that of the general population and similar to the one of those exposed to major traumas (3.5%). Evolution of the psychological symptoms over time varies: depressive symptoms improve within the first year, the symptoms of anxiety can persist beyond the first year and PTSD seems to remain stable. Over time, the problem tends to become chronic. The early diagnosis and treatment of PTSD can reduce its progression to chronicity.
Brain dysfunction at the ICU is one of the most common forms of organ failure that affects critically ill patients and occurs in its acute form as delirium. Not only acute brain dysfunction is common here, but also the brain dysfunction that occurs after the critical disease in the form of neurocognitive impairment that may last for months and years and prevents coming back to the previous functioning level.
The cognitive functions more commonly affected after ICU discharge are attention, memory and executive functions.11 Like psychological alterations, the neurocognitive ones can only be identified at the ICU discharge if they are properly tested, since in most cases they are not evident at first sight as it would be the case with physical alterations. Above all cognitive disorders are relevant in young patients who survive their ICU stay. Different studies have shown that neurocognitive impairment affects between 20% and 80% of ICU survivors, depending on the diagnostic tests used and the population assessed. Memory, attention and concentration disorders are present in 78% of patients one year after discharge. At the same time, speed processing and executive functions are also altered. During the BRAIN ICU study,12 we saw that 40% of the patients showed results that were consistent with moderate brain trauma and 26% a similar pattern to that of Alzheimer's disease. This pattern persisted in 24% and 34% of the patients at one year, respectively. In sum, cognitive impairment among ICU survivors affects over one third of the patients who were on mechanical ventilation.
The presence of persistent chronic pain after the critical disease has been described in several studies. It can be present for over 11 years after ICU discharge, and one third of the patients require professional treatment to alleviate it13 since it affects quality of life and ADL.14
Nutritional (caloric and protein) deficiency sustained by patients at ICUs involves weight loss which, upon discharge, is around 20%. Recovery is slow and only 70% recover within a year of discharge.1 During stay in the critical area around 2% of the lean muscle mass is lost per day, which is associated with protein and energy deficiencies. Recovering from weight loss is difficult, since patients suffer from reduction of appetite due to multiple causes such as depression, dyspnea, weakness, taste disorders, and/or swallowing disorders. The ICU stay-induced lack of teeth is another limiting factor to be able to recover from weight loss. In turn, nutritional deficiency conditions the survivors’ physical and functional rehabilitation.
Quality of life among ICU survivors is significantly reduced in the months and years to come compared to the general population.15 The impact on quality of life is associated with the above-mentioned physical, psychological and cognitive complications, along with chronic pain and the individuals’ social and family support. In turn, mortality in ICU survivors is different from that shown by the general population adjusted by sex and age. In their study, Williams et al.16 conducted a 17- year follow-up of ICU survivor patients after their discharge and they proved that one year mortality was greater compared to the group of survivors (standardized mortality ratio [SMR]=2.90; 95%CI: 2.73–3.08) and it remained greater than that of the general population in each year for the following 15 years of the follow-up (SMR=2.01; 95%CI: 1.64–2.46).
The effects of critical disease do not seem to derive directly from the characteristics of the disease that caused the patient to be admitted at the ICU or from its severity. This has been a cause for concern over the last 10 years among the international scientific community and several research lines have been developed to try to identify the consequences of critical disease and its possible risk factors. In addition, several randomized controlled trials (RCT) have been conducted to evaluate the effect that physical, psychological and neurocognitive rehabilitation has on improving the quality of life and physical and the psychological functionality among this group of patients. These trials have revealed variable results, they have been negative in some trials1,2,8–34 and positive in others.1–4,21–25 The last review published by the Cochrane Collaboration,35 whose objective was to evaluate the long-term results of an ICU discharge rehabilitation program, revealed inconclusive results, partly due to the variability in the tools used to measure each domain and the results assessed in each trial. The conclusions from the review conducted by Jensen et al.36 are similar; all the authors emphasize the need for standardizing the interventions and measuring the results in future trials.
Requiring a post-intensive therapy multidisciplinary treatment in this group of patients is significantly greater than in the rest of the population37–39; therefore, the use of healthcare resources and expenses is significant here.40 The UK National Institute for Health and Care suggests an evaluation and follow-up program for patients that survive the ICU in their NICE guidelines (National Institute for Health and Care Excellence),41 since between 10% and 40% of the patients who survive hospitalization suffer from re-hospitalizations within 30 and 180 days of hospital discharge which is associated with an increase of mortality and healthcare costs, in addition to being an objective of quality in some healthcare systems. In vulnerable populations such as the elderly,42 psychiatric patients, heart failure,43 who receive multiple drug treatments,44 and chronic conditions45 such as chronic obstructive pulmonary disease (COPD),46 the post-hospitalization follow-up has proven to have a significant impact on the reduction of the number of re-hospitalization, and as a consequence, in the reduction of costs. However, this has not been generalized to all hospitalized patients, that is, post-hospitalization follow-up would not be justified for the entire population at hospital discharge, but only for those patients with increased risk of suffering from re-hospitalization. The patients who survive critical disease with requirements of mechanical ventilation make up a sub-group that is vulnerable to suffer from re-hospitalization,47 since their quality of life is especially deteriorated as well as their functionality.6 There are some trials that justify the implementation of follow-up programs in this sub-group with aimed at reducing re-hospitalizations,48,49 and the costs of the program are justified by their results.50
The absence of a follow-up program makes the routine, close monitoring of patients at ICU discharge difficult, thus preventing the early detection of complications and their feasibility of treatment in an attempt to avoid new periods of hospitalization.
The goal of the present document is to collect basic measures of results and the tools validated in Spanish included in a Follow-up Program that would allow the evaluation of patients at risk of presenting PICS at hospital discharge. This document considers the possibility of assessing additional results; however, its main goal is to outline a minimum evaluation standard of the most important results that can be accessed by healthcare professionals in Iberian America.
MethodsThe Comité de Seguimiento y Rehabilitación de la Sociedad Argentina de Terapia Intensiva (Follow-up and Rehabilitation Committee of the Argentine Society of Intensive Care, SATI) summoned different inter-society committees involved with the issue of follow-up of survivors after ICU discharge in an attempt to design the guidelines of the Follow-up Program in patients at risk of developing PICS. The call was accepted by the Chapter of Kinesiology, the Nutrition Committee, the Critical Pneumology Committee, and the Mental Health Committee.
A detailed bibliographic search was conducted in each area; then, five meetings and 3 discussion forums were held (according to the three PICS spheres: the physical, the psychological and the neurocognitive) among the different committee members in order to achieve consensus on the characteristics of the Follow-up Program. Randomized and controlled trials were included and selected during the bibliographic search for rehabilitation protocols upon discharge from ICU to assess the existing evidence and make the corresponding recommendation for each domain. The recommendations were made in accordance with the GRADE system.
It was decided to include the following topics in the document (Fig. 1 and Table 1):
- •
Population meeting the inclusion criteria in the Follow-up Program
- •
Follow-up Frequency
- •
Personnel in charge of the Follow-up Program
- •
Basic domains to be assessed in the Follow-up Program and recommended tools for their evaluation
- ∘
Survival
- ∘
Physical Function
- ∘
Mental Health
- ∘
Pain
- ∘
Cognitive Function
- ∘
Quality of life
- ∘
Nutrition
- •
Additional domains to be assessed in the Follow-up Program
- ∘
Pharmacological therapy at ICU discharge
- ∘
Swallowing
- ∘
Assessment of pulmonary function
- •
Duration of the Follow-up Program
Domains included in the Follow-Up Program.
| Domains | Test | Cut-off point for referral |
|---|---|---|
| Survival | Interview | – |
| Physical function | Índice de Katz | Inability to perform ADL |
| Test de caminata de 6 minutos | Inability to walk | |
| Mental function | HADS | Score >7 |
| BDI-II | Score >14–20 | |
| BAI | Score >11 | |
| IES-R | Score >24 | |
| Pain | EQ5D question #3 | Moderate pain |
| Cognitive function | MOCA | Score <17 |
| Quality of life | EQ5D SF-36 | – – |
| Nutrition | MST | Score ≥2 |
The table shows the domains to be assessed during follow-up together with the tests validated into Spanish and the cut-off scores for every test that are indicative of referral to the specialist.
ADL: activities of daily life; BAI: Beck Anxiety Inventory; BDI-II: Beck Depression Inventory-II; IES-R: Impact of Event Scale-revised; EQ5D: Euroqol EQ-5D; HADS: Hospital Anxiety and Depression Scale; MOCA: Montreal Cognitive Assessment; MST: Malnutrition Screening Tool; SF-36: Short Form 36.
This program was designed to follow up ICU patients that show at least 2 of the following criteria:
- –
APACHE II score >14.
- –
Frailty upon admittance at the ICU51: according to the Clinical Frailty Scale CSHA (Clinical Frailty Scale, from the Canadian Study of Health and Aging).52 The patients that show mild frailty when they are admitted may be included in the program (for their description, see supplementary data).
- –
Duration of invasive mechanical ventilation (IMV) or non-invasive mechanical ventilation (NIMV) greater than 7 days.
- –
Patients who cannot walk with assistance or show significant weakness at ICU discharge.
- –
ICU stays over 10 days.
- –
Patients who according to the opinion of their attending physician show indication of follow-up.
- –
Patients with a diagnosis of prior severe cognitive impairment or any condition that prevents rehabilitation will be excluded.
In patients referred to rehabilitation or geriatric centers it will be possible to conduct the evaluation via phone call/email.
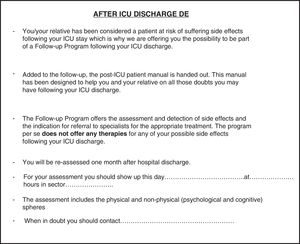
Patients who meet the inclusion criteria for the Follow-up Program at ICU discharge should receive the follow-up sheet (see Fig. 2) and the rehabilitation Manual. This manual was developed by Jones's53 group at St Helens and Knowsley Hospital and it was translated by the SATI Follow-up and Rehabilitation Committee with the authorization of Christina Jones (see the follow-up manual in Spanish available at https://www.sati.org.ar/index.php/areas-o/comites-o/comite-de-seguimiento-y-rehabilitacion-o/comite-de-seguimiento-y-rehabilitacion-produccion-academica).
RecommendationBased on the trials included, it is not possible to establish a recommendation about the population to be included in the follow-up (see Table 2).
GRADE-based recommendation for the Follow-up Program.
| Items | Evidence | Recommendation |
|---|---|---|
| Follow-up population | – | No recommendation |
| Frequency of follow-up | – | No recommendation |
| Professionals in charge | – | No recommendation |
| Survival | Low evidence | No recommendation |
| Physical function | Very low evidence | No recommendation |
| Mental function | Very low evidence | No recommendation |
| Pain | – | No recommendation |
| Cognitive function | – | No recommendation |
| Quality of life | Very low evidence | No recommendation |
| Nutrition | – | No recommendation |
| Duration of the program | No recommendation |
Recommendations according to the GRADE system and based on randomized controled follow-up studies at ICU discharge. Evidence is categorized as very low, low, moderate, or high.
GRADE: Grading of Recommendations Assessment, Development and Evaluation.
Here the recommendation from our expert panel's: the patient should meet at least 2 of the aforementioned criteria to be included in the program. However, the follow-up is orientated to patients with a logical possibility of rehabilitation, that is, patients with effects so severe that cannot improve over time will be excluded, as well as those that, at hospital discharge, are almost in the exact same condition as before the ICU admission. This differentiation, though complex, is crucial to make an adequate selection of patients.
Follow-up frequencyThe first meeting between the patient and the follow-up team should be held within the first month after hospital discharge to assess the different domains and eventually establish an early treatment. Patients showing alterations in the domains evaluated should be referred to the corresponding specialist, and they can have an appointment 6 months after hospital discharge. Patients that show no alterations can have an appointment 12 months after the discharge. Follow-up frequency can increase in case the attending team deems it necessary.
RecommendationBased on the trials included, it is not possible to establish a recommendation about the frequency of the follow-up (see Table 2).
Our expert panel's recommendation is this: the patient can be given an appointment within a month after hospital discharge and, depending on the alterations observed it will be the subsequent frequency including a appointment one year after discharge.
Personnel in charge of the Follow-up ProgramThe team in charge of the patient's follow-up at ICU discharge should know the complications associated with PICS and be capable of evaluating the different domains. This team should be made up of at least one physician and one kinesiologist. There is little evidence54 that it would be beneficial for the attending physician to be trained in the critical area. Ideally, a psychologist and a nutritionist should join the team, but that will depend on the possibilities of each institution.
RecommendationBased on the trials included, it is not possible to establish a recommendation about the personnel in charge of the follow-up (see Table 2).
Our expert panel's recommendation is this: the management of the PICS should be conducted via a multidisciplinary team led by a physician, preferably one trained in the critical area, and one kinesiologist. Ideally, a psychologist and a nutritionist could join the team.
Basic domains to be assessed in the Follow-up Program and recommended tools for their evaluationAll the evaluations mentioned below are tests validated in Argentina or into Spanish language that can be applied by healthcare personnel not specialized in a specific area.
SurvivalSurvival evaluation can be conducted via phone call or in person.
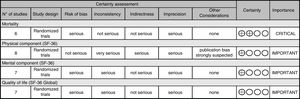
RecommendationBased on the trials included, it is not possible to establish a recommendation about the impact of the follow-up programs on the patients’ survival at UCI discharge (see Table 2 and Fig. 3).
Experts’ recommendation: we consider that follow-up programs are useful for the assessment of survival, but data are insufficient to evaluate their impact.
Physical functionPhysical function is one of the most compromised spheres at ICU discharge and it should be assessed during follow-up. There are several tests available and the following ones are the most highly recommended:
- –
Six-minute Walk Test (6MWTM). The 6MWTM55 evaluates comprehensively the response of the respiratory, cardiovascular, metabolic, musculoskeletal and neurosensory systems that an individual develops during exercise. This test can only be conducted in patients that can walk (for further details, see supplementary data). In those patients who cannot walk, the Katz index will be used here.
- –
Katz Index (KI): KI56 evaluates the people's dependence/independence in 6 ADL: bathing (sponge, shower or bathtub), dressing, toileting, transferring, continence, and feeding. If the patient shows some degree of dependence in any of the ADL, motor rehabilitation will be indicated (for further details, see supplementary data).
Another option for those who wish to make a more detailed evaluation is the following ones:
- –
Test Timed Up and Go57 (TUG): it requires the patients to get up from a chair, walk, turn around and walk back until they sit down again, while the examiner times how long it takes them to complete the test (for further details, see supplementary data).
Based on the trials included, it is not possible to establish a recommendation about the impact of the follow-up programs on the patients’ physical function (see Table 2 and Fig. 3).
Experts’ recommendation: follow-up programs are recommended for assessing and rehabilitating physical function at ICU discharge. Patients showing a significant reduction of their physical function as evidenced by their dependence on any of the ADL, evaluated by the KI, or by their impossibility to walk by 6MWTM, should be referred to motor rehabilitation.
Mental healthAccording to the most common complications found in this area, it is recommended to evaluate anxiety, depression and PTSD during follow-up after ICU discharge.
- –
Depression: to evaluate depression the score Hospital Anxiety and Depression Scale58 (HADS) or the Beck Depression Inventory-II (BDI-II) can be used. The HADS, which is most commonly used, consists of 17 items. Scores over 7 points would be indicative of referral to psychiatry. The BDI-II59 has a score that goes from 0 to 63; scores over 14 or 20 would be indicative of referral to psychiatry (for further details, see supplementary data).
- –
Anxiety: The Beck Anxiety Inventory (BAI)60 assesses anguish or panic disorders and generalized anxiety with a score that goes from 0 to 63. Values over 11 would be indicative of referral to psychiatry (for further details, see supplementary data).
- –
PTSD: there are different tools to evaluate PTSD, among these we have the Impact of Event Scale61 (IES) and the Impact of Event Scale-revised 62 (IES-R). The IES is made up of 15 items and 2 subscales that evaluate 2 of the 3 components of PTSD: intrusive thoughts and avoidance. The IES-R incorporates 7 new items (for a total of 22 items) and assesses the third component: the state of hyperarousal. Its use is not recommended for the diagnosis of PTSD; however, cut-off points are specified and suggest specific interviews. Scores ≥24 would be indicative of a clinical problem; scores ≥33 would be indicative of a probable PTSD diagnosis; and scores ≥37 would be indicative of a serious problem (for further details, see supplementary data).
Based on the trials included, it is not possible to establish a recommendation about the impact of the follow-up programs on the patients’ mental function (see Table 2 and Fig. 3).
Experts’ recommendation: follow-up programs are recommended for assessing and rehabilitating mental function at ICU discharge. In patients showing depression confirmed through the HADS>7 or BDI-II>14–20, or anxiety confirmed by BAI with scores over 11 or PTSD confirmed by the EIE-R scale with scores over 24, referral to the area of psychiatry should be indicated.
PainThe evaluation of pain should be included in the follow-up program since it is a frequent, limiting symptom in this group of patients. To evaluate pain question number 4 from the quality of life score Euroqol EQ-5D-3L should be used (see assessment of quality of life).
RecommendationBased on the trials included, it is not possible to establish a recommendation about the impact of the follow-up programs on the patients’ pain (see Table 2).
Experts’ recommendation: follow-up programs are recommended to assess and treat pain at ICU discharge. Patients showing pain after answering question number 4 from the Euroqol EQ-5D-3L score on quality of life (see assessment of quality of life) should be referred to the corresponding specialist.
Cognitive functionAssessing the cognitive function is a complex task and it requires the participation of specialists trained in this area. However, the early detection of cognitive disorders through simple tools can be useful in order to indicate early a timely referral to those specialized teams. We recommend the Montreal Cognitive Assessment63 (MOCA) test for the assessment of the cognitive function by personnel that is not specialized in this field. This is a simple test that allows training in its application (for further details, see supplementary data).
For those who wish to conduct a more thorough assessment, they can use the Repeatable Battery for the Assessment of Neuropsychological Status Update (RBANS® Update64) test, taking into consideration that its use is not cost-free.
RecommendationBased on the trials included, it is not possible to establish a recommendation about the impact of the follow-up programs on the patients’ cognitive function (see Table 2).
Experts’ recommendation: follow-up programs are recommended to assess and rehabilitate cognitive function at ICU discharge. Patients showing cognitive deficiencies assessed by the MOCA test with values under 17 points should be referred to a specialist in cognitive therapy for their rehabilitation.
Quality of lifeHealth-related quality of life questionnaires are tools to measure the physical, social and mental condition of a subject. The questionnaire recommended to assess the quality of life is Euroqol EQ-5D-3L65 – a simple, generic tool with multiple-choice answers. It is widely accepted, and its use has spread to different patient populations admitted to the ICU. This questionnaire has been validated to be used via phone call and it has proven to be a reliable measuring tool with family members (in an indirect way). It allows us to make comparisons with the general population, since there is such a thing as the Argentine population's criteria.66 A brief description appears in supplementary data. Questionnaire SF-36 can also be used, it has been translated into Spanish and it has proven to be a reliable tool to use in the population after ICU discharge. It allows more thorough assessments as it is a more comprehensive test.
RecommendationBased on the trials included, it is not possible to establish a recommendation about the impact of the follow-up programs on the patients’ quality of life (see Table 2 and Fig. 3).
Experts’ recommendation: follow-up programs are recommended to assess and rehabilitate quality of life at ICU discharge. The assessment can be conducted with either questionnaire, the EQ-5D 3L or the SF-36.
NutritionAt ICU discharge patients generally show a deficient nutritional condition which justifies assessment. Validation of the Malnutrition Screening Tool (MST) has recently been published to be used within rehabilitation programs.67 This tool takes into account weight loss and its cause and classifies patients as patients at nutritional risk or as patients who are not at nutritional risk.
RecommendationBased on the trials included, it is not possible to establish a recommendation about the impact of the follow-up programs on the patients’ nutritional condition (see Table 2 and Fig. 3).
Experts’ recommendation: follow-up programs are recommended to assess the nutritional condition at ICU discharge. Patients showing values ≥2 should be referred to the specialist for follow-up purposes (for further details, see supplementary data). In addition, feeding through nasogastric tube or the ostomy bag is an indication for follow-up for the nutrition team.
Table 1 describes the domains to be evaluated during the follow-up, along with the tests validated in Spanish that can be used for its evaluation and the cut points often used to indicate referral to a specialist.
Additional domains to be assessed in the Follow-up ProgramPharmacological therapy at the ICU dischargeThe detailed assessment of the pharmacological therapy received by the patient at hospital discharge is relevant in an attempt to adjust the drugs and their doses to the actual situation of the discharged patient.
SwallowingIn patients with swallowing difficulties (coughing, wet voice, difficulty swallowing certain textures) it is possible to perform an evaluation of swallowing at the patient's bedside or request a video-deglutition examination to diagnose it properly and eventually treat it.
Assessment of pulmonary functionPatients showing stridor or dyspnea at minimal or moderate efforts should be referred to the pulmonologist, so that they can conduct diagnostic studies to rule out lesions of the airways, that are so common in this population.
Duration of the Follow-up ProgramThe time of the follow-up will vary from patient to patient. Stabilization of functions is the most relevant criterion to terminate the follow-up. Identifying the aforementioned stabilization will not always be easy to diagnose. The tests conducted during the follow-up will be, without doubt, a useful tool to assess the domains that are considered more important for the patients’ quality of life; if the results of the test do no vary substantially between one visit and the next, its termination could be considered.
RecommendationBased on the trials included, it is not possible to establish a recommendation about the duration of the follow-up in patients at ICU discharge (see Table 2).
Experts’ recommendation: a minimum duration of one year of follow-up is recommended after ICU discharge.
ConclusionsLongitudinal follow-up offices allow a multidisciplinary approach to PICS, whose goal is the early identification of alterations in physical and mental health as well as to discuss with family members goals of re-hospitalizations and palliative care, and other aspects. The adequate selection of the population to be included in the program, personalized follow-up and multidisciplinary approach are some key aspects of this program. None of the follow-up measures proposed has evidence of quality, which means that it was only possible to make experts’ recommendations in all the cases.
FundingThis study has not been funded totally or partially.
Conflicts of interestThe authors declare no conflicts of interest whatsoever.
Please cite this article as: Busico M, das Neves A, Carini F, Pedace M, Villalba D, Foster C, et al. Programa de seguimiento al alta de la unidad de cuidados intensivos. Med Intensiva. 2019;43:243–254.