The term “sustainable development”, as used in the Brundtlandt Report (1987), refers to development that satisfies the needs of the current generation without placing at risk the capacity of future generations to satisfy their own needs.
The concept of “One Health”, introduced in 2000, in turn, refers to the notion that human, animal and environmental health are interdependent (https://www.who.int/news-room/questions-and-answers/item/one-health). According to the World Health Organization (WHO), the concept of One Health focuses on the worldwide objective of increasing interdisciplinary collaboration (public health, medicine, medical care, veterinary medicine, research, environmental sciences, etc.) in the care of human, animal and environmental health, to develop and implement programs, policies and legislation in favor of improved health.
In 2015, all the member states of the United Nations approved 17 objectives as part of the Agenda 2030 for Sustainable Development; of these, 7 were related to health, sustainability and the environment (https://www.who.int/news-room/questions-and-answers/item/one-health). In 2020, the countries presented their climate action plans, the so-called “Nationally Determined Contributions” (NDC), to meet the pledges of the Paris Agreement. Following the agreements of the climate summit in 2021 on the occasion of the COP26 in Glasgow, the change needs to be implemented in our Intensive Care Units (ICUs), progressing in compliance with the Paris Agreement and the Agenda 2030 for sustainable development. Of the 50 countries that attended the summit, 14 set the year 2050 as the deadline for Greenhouse Gases (GHG) = Zero. In 2022, Sanidad #PorElClima (https://sanidadporelclima.es/) acknowledged 10 Spanish hospitals as pioneers in reducing their carbon footprint to secure emission neutrality in 2050.
The term GREEN ICU (GREater ENvironmental sustainability in Intensive Care Units) is a multidisciplinary initiative to design an evidence-based guide to reduce the environmental footprint of intensive care (https://blogs.brighton.ac.uk/sustainablecriticalcare/, https://cris.brighton.ac.uk/ws/portalfiles/portal/25490301/GREEN_ICU_SHARE_2021.pdf). Concepts have been expanded from “evidence-based medicine” to “patient-centered medicine”, and now “planet-centered medicine”.
The impact and consequences1 for both people and the planet of the extraction of natural resources, manufacturing, packaging, transport, use/reuse and recycling/elimination of waste, the emission of greenhouse gases (GHG: CO2, methane, nitrous oxide), the use and contamination of water, the generation and waste of energy, ecotoxicity and social and economic impacts… are simply not assimilable.
Mention should be made of some data to place the importance of the problem in focus. If healthcare were a nation, it would rank fifth in terms of GHG.2 These gases form part of air pollution and are responsible for 4.2 million deaths a year.3 In this regard, ICUs make an important contribution to the emission of CO2.4 Eighty percent of the carbon footprint is attributable to clinical care as such.5 In addition, hospitals generate 20% of the flow of solid waste,6 and it has been found that 47% of this waste is incinerated, 16% is recycled and 7% is discarded.
The use of disposable materials and PPE (personal protection equipment) during the COVID-19 pandemic worsened the problem. The environmental impact of the critical patient is attributable not only to GHG but also to ecotoxicity in relation to material flow analysis, waste generation and the use of about 300 liters of water a day.4 Special mention also should be made of the fact that 90% of all orally administered medications are excreted in wastewater as active substances through patient urine and stools.7 Such waste in turn can lead to the development of antibiotic-resistant strains. This causes over 33,000 deaths a year in Europe.8
The drugs we use are characterized by persistence, bioaccumulation and toxicity. This and the generation of resistance to antibiotics causes damage over the entire chain of life, and ultimately impacts upon humans. On the other hand, 30% of our clinical care is of low value, causing contamination without health benefits of any kind.7 Furthermore, hospitals increasingly receive patients with disorders linked to climate change,9 and this further increases the generation of GHG. Considering all the above, it is clear that our efforts toward sustainability must move faster.
Debate about the possible solutions focuses on the following aspects:
- •
A lack of protocolized updates on what we need to know in order to form part of the solution.
- •
“Bottom to top” initiatives, creating local Green Teams, versus legal regulations and “top to bottom” policies, with a triple strategy at ecological, social and financial level.
- •
Types of analyses needed to focus the solution: measurement of our carbon footprint representing the total GHG (ScopeCO2), life cycle analysis (LCA),6 for example via ReCiPe 2016, material flow analysis (MFA), and the identification of environmental critical points (hot spots).
- •
Zero carbon footprint is not equivalent to zero environmental impact. Each day use is made of drugs and disposable materials that cause ecological damage.
- •
Fifty percent of all ICU waste could be recyclable with adequate separation and processing. Wastewater treatment plants are not designed to eliminate pharmaceutical products.
- •
A sustainable ICU is cyclical, allowing auto-regulation and resolving problems as close as possible to their origin.
- •
Healthcare expenditure and the inferred GHG do not imply improved outcomes or better life expectations.10
- •
Following the “do not do” recommendations reduces burdens referred to patients, costs and the environment.10
For over a decade, solutions have been proposed focused on the care of the critical patient. Improvement is possible, and the NHS in the United Kingdom has been able to reduce its carbon footprint by 580 kt CO2e in 2021. We can not only care for but also heal our planet.
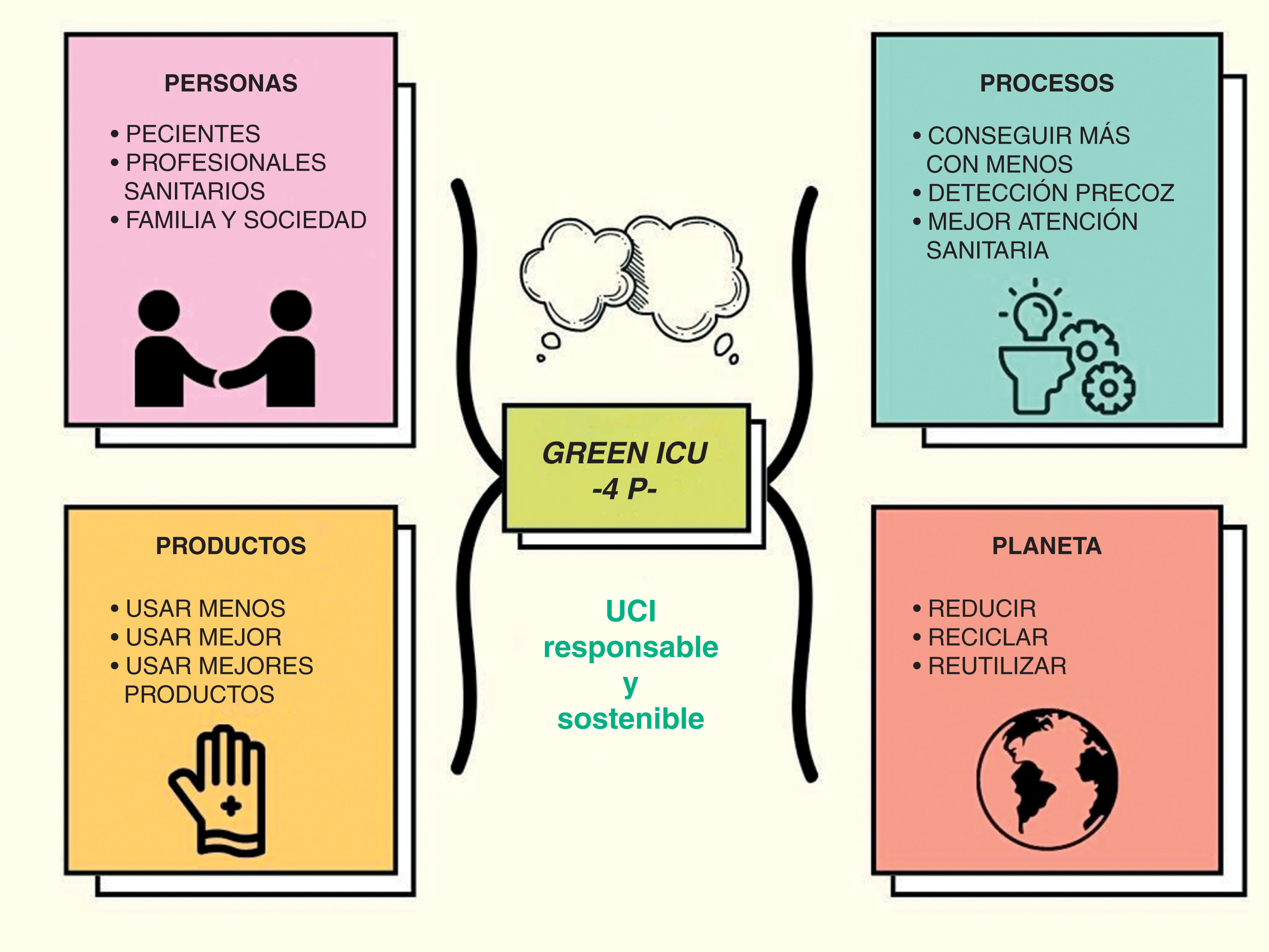
A strategy could focus on the 4 Ps (Fig. 1): products, people, processes and planet (Table 1). Prevention is crucial in this regard, with priority being placed on less and better first use/intervention. In addition, our defined objectives should be consensus-based, assumed, long-term, with a genuine impact, of a local and global scope, and integrated within our occupational and personal identity.
4P: Products, processes, people and planet.
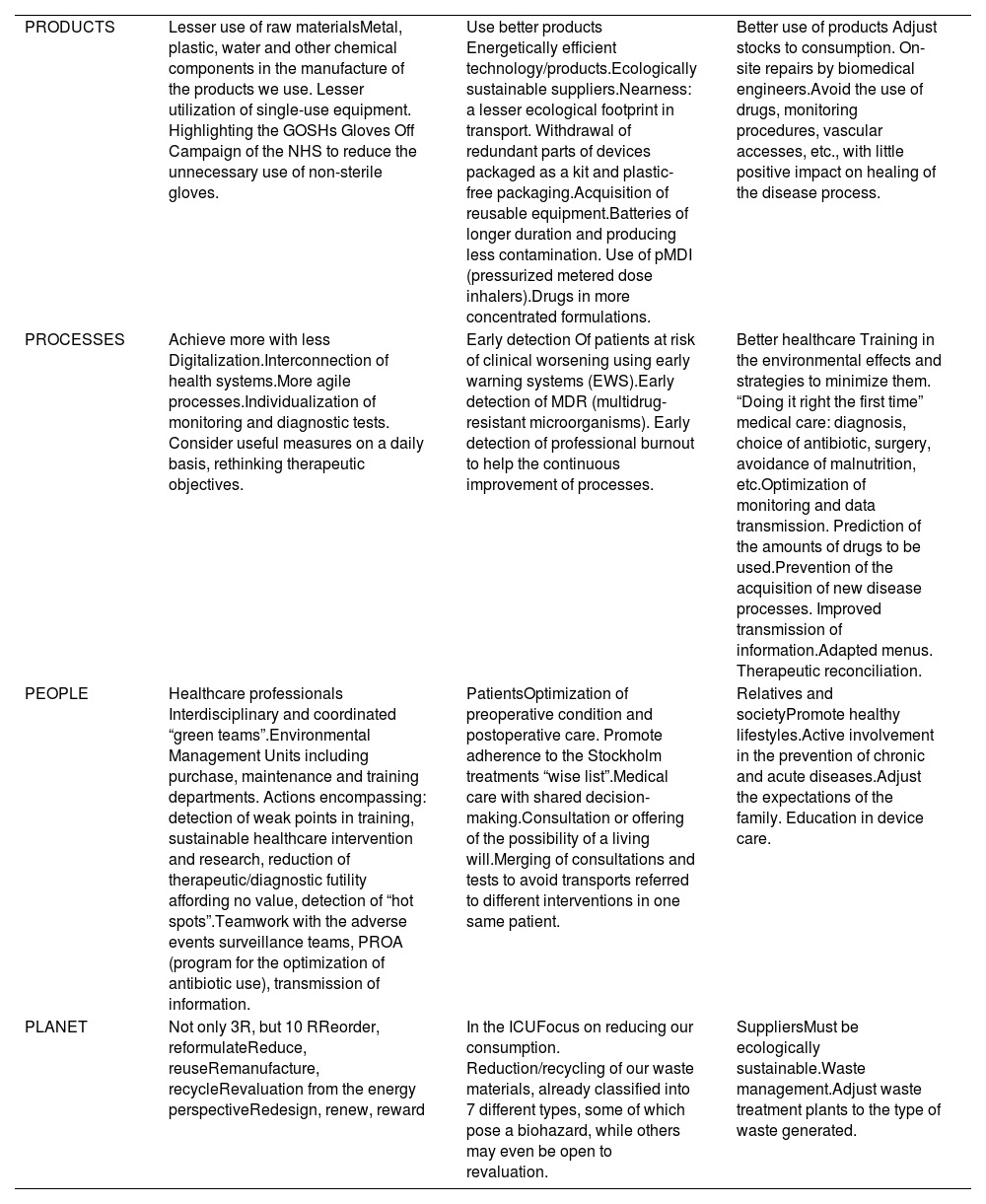
| PRODUCTS | Lesser use of raw materialsMetal, plastic, water and other chemical components in the manufacture of the products we use. Lesser utilization of single-use equipment. Highlighting the GOSHs Gloves Off Campaign of the NHS to reduce the unnecessary use of non-sterile gloves. | Use better products Energetically efficient technology/products.Ecologically sustainable suppliers.Nearness: a lesser ecological footprint in transport. Withdrawal of redundant parts of devices packaged as a kit and plastic-free packaging.Acquisition of reusable equipment.Batteries of longer duration and producing less contamination. Use of pMDI (pressurized metered dose inhalers).Drugs in more concentrated formulations. | Better use of products Adjust stocks to consumption. On-site repairs by biomedical engineers.Avoid the use of drugs, monitoring procedures, vascular accesses, etc., with little positive impact on healing of the disease process. |
| PROCESSES | Achieve more with less Digitalization.Interconnection of health systems.More agile processes.Individualization of monitoring and diagnostic tests. Consider useful measures on a daily basis, rethinking therapeutic objectives. | Early detection Of patients at risk of clinical worsening using early warning systems (EWS).Early detection of MDR (multidrug-resistant microorganisms). Early detection of professional burnout to help the continuous improvement of processes. | Better healthcare Training in the environmental effects and strategies to minimize them. “Doing it right the first time” medical care: diagnosis, choice of antibiotic, surgery, avoidance of malnutrition, etc.Optimization of monitoring and data transmission. Prediction of the amounts of drugs to be used.Prevention of the acquisition of new disease processes. Improved transmission of information.Adapted menus. Therapeutic reconciliation. |
| PEOPLE | Healthcare professionals Interdisciplinary and coordinated “green teams”.Environmental Management Units including purchase, maintenance and training departments. Actions encompassing: detection of weak points in training, sustainable healthcare intervention and research, reduction of therapeutic/diagnostic futility affording no value, detection of “hot spots”.Teamwork with the adverse events surveillance teams, PROA (program for the optimization of antibiotic use), transmission of information. | PatientsOptimization of preoperative condition and postoperative care. Promote adherence to the Stockholm treatments “wise list”.Medical care with shared decision-making.Consultation or offering of the possibility of a living will.Merging of consultations and tests to avoid transports referred to different interventions in one same patient. | Relatives and societyPromote healthy lifestyles.Active involvement in the prevention of chronic and acute diseases.Adjust the expectations of the family. Education in device care. |
| PLANET | Not only 3R, but 10 RReorder, reformulateReduce, reuseRemanufacture, recycleRevaluation from the energy perspectiveRedesign, renew, reward | In the ICUFocus on reducing our consumption. Reduction/recycling of our waste materials, already classified into 7 different types, some of which pose a biohazard, while others may even be open to revaluation. | SuppliersMust be ecologically sustainable.Waste management.Adjust waste treatment plants to the type of waste generated. |
These four principles (https://healthmanagement.org/c/icu/issuearticle/green-icu-4ps-it-is-not-an-option-to-not-accomplish-it) are reproducible in our setting, perhaps with different tools, and if shared could allow us to progress towards our goal quickly. The fundamental consideration, as with our patients, is not to cause harm - and this also applies to our planet. We must act today; change is mandatory. We need to have a “sustainability kit” for our responsible ICUs, because we as intensivists want practical measures, adopting an approach where medical and environmental ethics walk together.
FundingThe present study has received no funding.
Conflict of interestThe authors declare that they have no conflicts of interest.
.11.
Thanks are due to the healthcare professionals as a driving force of life and sustainable change.