Handover is a frequent and complex task that also implies the transfer of the responsibility of the care. The deficiencies in this process are associated with important gaps in clinical safety and also in patient and professional dissatisfaction, as well as increasing health cost. Efforts to standardize this process have increased in recent years, appearing numerous mnemonic tools. Despite this, local are heterogeneous and the level of training in this area is low.
The purpose of this review is to highlight the importance of IT while providing a methodological structure that favors effective IT in ICU, reducing the risk associated with this process. Specifically, this document refers to the handover that is established during shift changes or nursing shifts, during the transfer of patients to other diagnostic and therapeutic areas, and to discharge from the ICU. Emergency situations and the potential participation of patients and relatives are also considered. Formulas for measuring quality are finally proposed and potential improvements are mentioned especially in the field of training.
El traspaso de información (TI) es una tarea frecuente y compleja que lleva implícito el traspaso de la responsabilidad del cuidado del paciente. Las deficiencias en este proceso se asocian a importantes brechas en la seguridad clínica e insatisfacción de pacientes y profesionales. Los esfuerzos por estandarizar el TI se han incrementado en los últimos años, dando pie a la aparición de herramientas mnemotécnicas. Globalmente las prácticas locales del TI son heterogéneas y el nivel de formación, bajo.
El objetivo de esta revisión es enfatizar la importancia del TI y proporcionar una estructura metodológica que favorezca el TI efectivo en las UCI, reduciendo el riesgo asociado a este proceso. Específicamente, se hace referencia al TI durante los cambios de guardia y los turnos de enfermería, durante el traslado de los pacientes a otras áreas diagnósticas y terapéuticas y en el momento del alta de UCI. También se contemplan las situaciones de urgencia y se señala la potencial participación de pacientes y familiares. Por último, se proponen fórmulas para la medición de la calidad y se mencionan posibles mejoras en este proceso, especialmente en el ámbito de la formación.
In current medical practice, which is fundamented upon teamwork and where no single professional is able to supervise the care of a patient for 24h, 365 days a year, information handover (IH) is a frequent and unavoidable process.
In our setting, IH is essentially a matter of habits and routines, and only in exceptional cases is it mediated by some type of specific training.1,2 Perhaps for this reason communication errors are an important source of incidents and adverse events. In the SYREC study, contributing factors related to communication were found to be present in 5.76% of the incidents and in more than one-half of the sentinel events.3 In this respect, deficient IH has been associated to treatment errors, prolonged patient stay and increased healthcare costs.4
The Joint Commission has recommended the development of structured communication procedures among professionals.5 In parallel, other countries have launched similar initiatives.6–8 In our setting, the Patient Safety Strategy of the Spanish National Health System 2015–20209 has underscored the need to promote communication among professionals in order to ensure that the information handed over is precise, adequate and addressed to the correct person, and advocates the implementation of structured communication techniques.
The aim of the present review is to illustrate the importance of IH and at the same time afford a methodological structure favoring effective IH in the Intensive Care Unit (ICU), and reducing the risks associated to this process. Specifically, this document refers to IH established during changes in medical shifts or nursing shifts; during the transfer of patients to other diagnostic and therapeutic areas; and at discharge from the ICU. Emergency situations and the potential participation of patients and relatives are also considered. Lastly, formulas for measuring quality are proposed, and potential improvements are mentioned particularly in relation to training.
Information handover: terms and definitionsInformation handover: this refers to communication among healthcare professionals, in which the clinical information of a patient is transmitted, and the responsibility of care is transferred either temporarily (change in shift) or permanently (change in Unit or healthcare level; see the subsection “Care transition”).10
Intra-disciplinary information handover: this occurs between healthcare professionals that have the same academic training (physician–physician in the change in shift, nurse-nurse and assistant-assistant in the change in shift, for example).
Inter-disciplinary information handover: this occurs between healthcare professionals that have different academic trainings (physician–nurse in the daily patient visit, for example).
Care transition: this occurs when the patient is moved to a different place and healthcare level, and is transferred to another Department for the continuation of treatment.
Checklist: this is a tool making it possible to determine whether certain standardized procedures have been carried out, or whether the necessary equipment/resources for safely carrying out an activity are available.11
Daily targets: these are a series of concrete objectives/goals that are intended to be reached in the course of the day. A checklist allows them to be visible to all the team members.
Informative sessions (briefings/debriefings): briefings are short team meetings in which roles are assigned, expectations are established and problems are anticipated. They can be oriented toward the identification of risk situations. Debriefings in turn are meetings designed to exchange information after team intervention, reviewing the actions taken and analyzing their effectiveness.
Team huddles: these are short ad hoc meetings (maximum 15min) in which each member of the team indicates the priority objective of his or her activity. These meetings are useful for readjusting objectives.
Characteristics of the information handover process adapted to the change in shiftInformation handover should be viewed as a process. It is not advised to create a process for all types of IH, though processes for some of them—such as the change in shift—are indicated. This helps to identify the phases that conform the task. By understanding it this way, we not only demonstrate the cognitive demands involved but also make it easier to evaluate the functioning of the process and introduce improvements.12 It also must be considered that a process designed for an ICU might not be adequate in other settings.
Information handover referred to changes in shift is defined as an interactive process in which specific patient data are communicated and the responsibility is transferred from the team that is ending its shift to the team that replaces it.13 It is advisable for the construction of this process to include a series of sections:14
- (a)
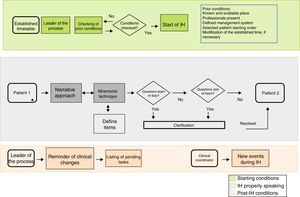
Creation of a map of the process. This map can be used to define the key points for conducting IH. It can be designed with different levels of detail. Each section defines potential areas for analysis and, where applicable, improvement (Fig. 1).
- (b)
Adaptation of the process to the local culture. The following questions need to be answered:What is the purpose of IH? Answering this question attributes character to the process; each ICU can opt for an operative, formational or mixed approach.
- -
What is the content of IH? The information which each ICU considers essential for ensuring quality care. The content can be modulated by factors inherent to the patient (e.g., severity or evaluative period) or to the environment (e.g., who participates in IH).
- -
Who should be the leader of the process? A professional with experience and with a broad vision of what happens in the Unit.
- -
Who should carry out IH? It should be carried out by professionals (emitters and receptors) with a required minimum of training in intensive care medicine, and always under the supervision of a senior professional.
How should IH be carried out? By combining the verbal and, if necessary, written information (reports) or images (complementary tests) or drawings (schematic representation of surgical procedures). A narrative approach is recommended, with the support of mnemonic tools, leaving a space for questions or comments13 (see the section: “Narrative approach and mnemonic rules”). The leader of the IH should guarantee the proportionality of time used in each patient and redirect the discussions (or assign them to some other moment or format), in order to secure the objective of the IH. It is advisable for the leader to have the authority to select the order of patients in the IH, if so advised based on severity criteria. A crucial aspect is the control of interruptions: it is recommendable to identify a person, other than the leader (perhaps the assistant coordinator or some other previously designated individual), to be placed in charge of attending the visit of other professionals and calls to the pager.
Where should IH take place? The location should be known and established by consensus, without discarding the possibility of some types of IH at the patient bedside—which could contribute relevant information from the surroundings.13
- (c)
Diffusion of the process. Diffusion is required of the map, contents and location, with identification of the leader of the IH so that all the professionals of the Department can be duly informed and participate actively.
- (d)
Obtainment of feedback from the surroundings. It is important to obtain feedback on all the aspects of the process in order to allow modifications and adaptations to the type of patients attended and to the local care structure, including the availability or not of specialists in training.
- (e)
Monitoring of the process. This is the task of the leader. Satisfaction questionnaires are useful in this regard (see the section: “Quality of IH: indicators and barriers”).
- (f)
Management of barriers. The approach to IH always implies in-depth work (related to the organizational culture) for the Department supervisors to minimize the barriers facing the process. Examples of such barriers are a lack of interest in this type of activity (which may be viewed as being of scant relevance), tiredness (physical and mental), stress,15 a lack of an adequate place, delays caused by the care burden, a lack of teamwork culture, and an absence of communication training.16
Fig. 2 offers some recommendations for improving IH during the duty visit. The construction of a solid process around IH can result in benefits such as the correction of management errors,17 the construction of a shared image of the patient (this being an essential element, since it overcomes differences in criterion and experience between intervening professionals),18,19 and the ensuring of individual and organizational learning.20,21
Narrative approach and mnemonic toolsInformation handover is strongly dependent upon the circumstances of each patient, and in many cases it must be oriented more toward projection or anticipation of the clinical course than toward the listing of data—a circumstance that greatly complicates standardization of the process. In this regard, it is advisable to start IH using the narrative approach, underscoring the singularities of each clinical case. By sharing this information, it is possible to jointly devise a management plan and anticipate changes.22
On the other hand, mnemonic tools facilitate structuring of the information and avoid the omission of relevant data—this being one of the most frequent problems.23 Over twenty have been described.24 However, it must be considered that rigid standardization has not always been associated to improvements in safety, though it does increase the perception of control of the process on the part of the professional, and facilitates teamwork.25 Furthermore, although the structure and conformation of these tools has recently been analyzed in depth,23 the quality of the studies and the lack of validation preclude definitive recommendations on the use of each tool with respect to the rest.26 One of the most widely accepted and used tools in our setting is the SBAR (Situation, Background, Assessment and Recommendation); it therefore could be used as a starting option. Examples of its use can be found in Tables 1 and 2. Other tools have also been found to be very useful27; each ICU therefore should adopt the methods used for IH in accordance with their concrete needs.
Example of the use of the SBAR tool in nursing information handover.
| Situation | Antecedents |
|---|---|
| Identification of the professional | Date of admission or days of stay |
| Identification of the patient | Allergies |
| Principal diagnosis | Diet |
| Medication | |
| Catheters, tubes and drains | |
| Pain | |
| Recent interventions |
| Evolution | Recommendations |
|---|---|
| Vital signs | Tasks requiring monitoring |
| Neurological condition | Pending treatments |
| Respiratory condition | Pending tests |
| Treatment administered during the shift | |
| Tests made during the shift |
Example of SBAR for information handover during the patient transfer preparation phase in surgical procedures (communication with the Departments of Anesthesia and Surgery).
| Situation | Antecedents |
|---|---|
| Identification of the professional | Date of admission or days of stay |
| Patient name and box number | Allergies |
| Principal diagnosis | Catheters, tubes and drains |
| Reason for the procedure | Recent interventions |
| Evolution | Recommendations |
|---|---|
| Neurological condition. Sedoanalgesia. RASS. Type of monitoring | Most important recent problems |
| Respiratory condition. Modality. FiO2. PEEP | Pending treatment |
| Hemodynamic condition. Vasoactive drugs | |
| Renal condition. Hemodialysis. Renal replacement therapy | |
| Infectious condition. Antibiotherapy | |
| Hematological condition | |
| Family information |
Nurses face many changes in shift, participate in within-hospital transfers, and can leave the ICU setting to carry out certain activities. As a result, IH is also a crucial element in their daily work.
On considering a concrete aspect, namely IH on occasion of the nursing change in shift, this corresponds to an intra-disciplinary IH (defined in the section: “Information handover: terms and definitions”).28 Specifically, in this type of IH the existing barriers have been studied in depth.29,30 In this respect, we can mention barriers related with the emitter (difficulty transmitting the relevant information in an orderly manner, excessive information, or difficulty remembering part of the information); with the receptor (fear of asking); or with both (cultural barrier, lessened attention due to the fact that this is a routine process, and the inclusion of personal judgments and subjective data). Further barriers are the lack of standardization of the process; the surroundings (noisy environment, interruptions and lack of confidentiality and intimacy); limited availability of time; the patient (IH being more complex in the case of more seriously ill patients); and with training (scarce). In view of these barriers, and particularly considering the time used and the environment in which the procedure is carried out, the use of mnemonic tools may be more advisable.31Table 1 shows the utilization of the SBAR tool. It has recently been suggested that a variant of the SBAR, the so-called ISOBAR (I: identification of the professionals and of the patient; O: observation and description of vital signs and pending tests), adapts better to the different specialties, though it has not been contrasted in the UCI.32
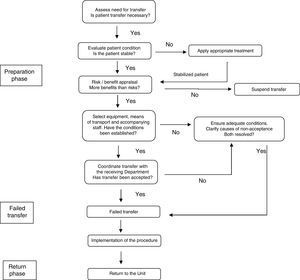
Information handover during the patient transfer processMany procedures require moving the patient outside the ICU.33 Patient transfers are essentially multidisciplinary processes involving not only the duly trained physician and nurse,34 but also assistant staff and professionals from other Departments. It is advisable for each ICU to have its own transfer protocol specifying not only the tasks and monitoring procedures involved but also the type of communication among the professionals35 (Fig. 3).
Preparation phase:
This is the most complex phase. Adequate planning can reduce adverse events during transfer.36 The preparation phase is characterized by the coexistence of intra- and inter-disciplinary IH.
With regard to intra-disciplinary IH (physician–physician), handover in transfer to the surgical area and the performance of diagnostic tests serves to establish consensus regarding the indication of the procedure and justification of patient transfer. It also helps to specify the destination, confirm the meeting time, and estimate the duration of the procedure. In the specific case of IH related to surgical procedures, the use of mnemonic tools is recommended (Table 2).
In turn, once transfer has been confirmed, inter-disciplinary IH (which includes nurse-physician-assistant) can be implemented through a specific checklist that has been shown to improve safety37 (Table 3), and which should be directed by the nurse in charge of the patient, with the presence of all the members taking part in the transfer of the patient.
Proposed checklist for the preparation phase.
| Pre-transfer phase | Yes/no |
|---|---|
| 1. Is the patient stable enough? | |
| 2. Is there any absolute contraindication? | |
| 3. Is informed consent necessary? Informed patient/family | |
| 4. Are isolation measures needed? | |
| 5. Has availability been confirmed by the receiving area? | |
| 6. Has the exact reception time been confirmed? | |
| 7. Is the professional team required according to the clinical situation available? | |
| 8. Is the required monitoring available? | |
| 9. Have the oxygen, transfer respirator and battery been checked? Respirator parameters | |
| 10. Has the transfer monitor and battery been checked? | |
| 11. Has the necessary medication and transfer kit been checked? | |
| 12. Have the infusion pump batteries been checked? | |
| 13. In the case of a chest drain, decide the need for clamping | |
| 14. Is the necessary documentation available? | |
| 15. Has the airway been secured and is it adequate? Is secretion aspiration needed? Tracheal tube cuff check? Tube correctly affixed? | |
| 16. Are the venous accesses suited to the clinical situation available? | |
| 17. Can perfusion, nutrition or other devices be momentarily suspended? | |
| 18. Is the transfer material correctly distributed? | |
| 19. Has the receiving area been informed that the patient is leaving the Unit? Has access to the elevators been checked? |
Transfer phase:
The quality of care during this phase also has an impact upon the appearance of incidents.38 It is necessary to maintain correct coordination during transfer in order to facilitate access to the point of destination—including the availability of elevators. Information handover in this phase is of an inter-disciplinary nature (fundamentally verbal) and is focused on data referred to deviations from the pre-established plan. In the case of incidents, the recommendations applicable to IH in emergency scenarios should be followed. In this phase, if the patient is being moved to the operating area, a mnemonic tool should be used with the anesthetist and surgeon to check patient arrival status (Table 2). Caruso et al.39 have reported that the use of standardized and face-to-face IH between the physicians in charge of the patient in the ICU and the Department of Anesthesia does not prolong transfer time and significantly improves professional satisfaction.
Return phase:
Inter-disciplinary IH also takes place among the professionals that have carried out patient transfer. It is advisable for the exchange of information to based on the same checklist used in the preparation phase (Table 3). Logically, not all the checklist items are of use in this phase, though the list will serve as reference to safely revert the changes in monitoring and check devices, as well as patient airway and stability. A variant of this phase is when return transfer is carried out by another Department, for example Anesthesia following surgery. In this case it is also advisable to use the same mnemonic tool as that employed in the preparation phase (Table 2).
Information handover at discharge from the ICUDirect communication between the supervising physicians of the ICU and the physicians of the destination Department only occurs in 25% of the cases40—this being associated with an increase in adverse events,41 readmissions42 and professional dissatisfaction.43 Communication should be a structured process involving verbal and documental IH.44 In this regard, van Sluisveld et al.,45 in a systematic review analyzing the interventions made to improve the safety and efficacy of IH between the ICU and the conventional hospital wards, found that the use of a support for IH (a physical or electronic document) and the mediation of a liaison nurse have a significant impact upon the reduction of delays in discharge and adverse events. No decrease in mortality was observed, however, and inconsistent results were obtained in relation to ICU stay and readmissions. In our setting, and from a practical viewpoint, we recommend IH to take place at the patient bedside (between the supervising physician of the ICU and his or her counterpart in the destination ward), using verbal and documental information (supplied by the discharge report itself).46,47 Communication (at least be telephone) is also advised when the patient effectively leaves the ICU.
As commented above, the intervention of the nursing staff in this process is crucial, since it involves coordination among Departments.48 The nursing discharge report, together with displacement of the nurse to the destination Department, facilitate the continuity of patient care.49 The nursing discharge report can also serve as a guide for channeling verbal information once the patient reaches the destination ward. The report should contain data referred to identification of the patient, information for contacting the family or representative, and data on the disease establishing the indication of ICU admission, the patient vital signs at discharge from the ICU, intravenous medication (including parenteral nutrition), gastric tolerance, state of care of sores and wounds, types of drains, catheter line insertion dates, psychosocial particulars, and identification of the professional drafting the report.50 In a new recently published systematic review, Wibrandt et al.51 underscored the liaison nurse as the most important element for improving the safety of the patient during this process.
Information handover in emergency situationsCommunication plays a key role both within and between care teams in emergency situations. Such circumstances require assertive and unequivocal communication. No team acting in an emergency situation can work in total silence.52
Different formulas can improve communication in situations of this kind.53 The decision to incorporate them to the daily work routines constitutes a profound change; introduction therefore should be made gradually and only in selected processes. Table 4 offers some examples of communication patterns applicable in this context. It can also be useful to suppress hierarchical gradients, make use of the SBAR tool, adopt briefing-debriefing techniques (see the section: “Information handover: terms and definitions”), introduce so-called communication under 10,000 feet (based on the aeronautical analogy whereby only critical maneuvers are made under that altitude – such as landing and takeoff, for example – and where communication is limited to what is strictly necessary; in our case, this kind of communication should be reserved for situations such as orotracheal intubation, catheterization, etc.), or use the so-called two challenge rule (employed to assume the responsibility of a task when the individual in charge fails to do so for some reason).
Useful communication standards in emergency situations.
| Communication strategy | Medical example |
|---|---|
| Avoid confusing language when a clear situation is identified | I need a surgeon! Intubate the patient now! |
| Flying by voice: I expose my opinions in public to be heard; we invite the rest of the team to confirm or correct | We still have no pulse after 10! What can be happening? What have we overlooked?? |
| Grading of assertiveness, according to the communication objective we seek | Orders: Intubate now! Statement: We need the X-ray! Suggestion: We should get the X-ray! Question: What if we first get the X-ray? Preference: I think we should first get the X-ray |
| Five-step approach We draw attention We present the problem in clear language We present the problem as we see it We propose a solution: We reach agreement: | Excuse me doctor! The patient is entering bradycardia! The patient is suffering arrest! Prepare the defibrillator! What do you think? |
| Repeat-back: repeat or confirm method | A: Administer 3mg of adrenalin! B: So I administer 3mg of adrenalin? A: Yes |
| SBAR | Situation: I would like to comment on a patient Background: It's the 35-year-old polytrauma patient Assessment: Surgical fixation was done 7 days ago, he has fever Recommendation: I suggest wound culture |
| Step-back: done to re-evaluate and take a moment to think after every certain interval of activity | Stop massaging while I check for a pulse! |
| Communications under 10,000 feet: management of interruptions, distractions. It can be given a term in our setting, e.g.: “Only critical information: OCI” | Only operation language A: I need your opinion; do you have a moment? B: No, OCI! |
On the other hand, team management in emergency situations encompasses other fundamental aspects, e.g., formal team creation, operating dynamics, the adoption of shared decision making mental models, the facilitation of feedback after interventions, and the management of fatigue.54 As this is an aspect of great importance, the impact of team organization upon patient prognosis remains the subject of controversy.55
Information handover and participation of the patients and caregiversHistorically, IH has been regarded as a task exclusive of the professionals, without implication on the part of the patients or their caregivers (including relatives). The presence of these people requires the comprehensive handling of information,56 though there are also several advantages: identification of the supervising professionals is facilitated, certain decisions can be shared, and opportunities arise for identifying room for improvements in the system.57 The idea that patients and their caregivers form part of the working team in the healthcare setting is a disruptive concept. Can a patient or the relatives of a patient be regarded as members of the working system? The answer is probably yes, particularly when considered from a humanization of care perspective and if the concept of multidisciplinary work is expanded.58,59
Nevertheless, IH involving patients, caregivers and families must take a series of aspects into account, such as the adequate maintenance of patient confidentiality and privacy; the possible need to request patient consent (if able to do so) to the sharing of clinical information with the caregivers (taking into account the complex family interactions there may be in each case); evaluation of the true capacity of the patient and family to participate in IH; and assessment of whether this method obliges the omission of relevant information or increases interruptions—which would result in inefficacy of the process.
In general, the evidence in relation to communication between healthcare professionals and the patient relatives indicates that the use of printed documents addressing the disease and condition of the patient admitted to the ICU, in the context of structured interviews (in which other professionals focusing on ethical aspects or palliative care may also participate), improves understanding on the part of the family; has a positive impact upon their emotional state; and reduces ICU stay and the intensity of treatment.60
Quality of information handover: indicators and barriersDespite the implementation of different strategies designed to improve IH, no gold standard capable of serving as reference has been established to date. In this regard, further development of tools is required in order to allow adequate evaluation.61–63
From a practical perspective, IH quality analysis could be addressed through its effects upon structural indicators, evaluating whether there is an IH protocol in the ICU. This would be the first step.
The second step would be to address the process indicators. This can be done by using the quality indicators of the SEMICYUC64 (protocolized information handover) or prospectively evaluating compliance with the IH process (see the section: “Characteristics of the IH process adapted to the change in shift”), in accordance with the design we have used, based on the use of a checklist.
It is also possible to use outcome indicators, considering for example the number of adverse events and mortality.65
Lastly, IH efficiency indicators may be considered: the time taken by the process; the time taken to resolve incomplete communications; and reduction of the number of duplicate actions.
Improvements in the information handover process: trainingPractically all the curricular guides on patient safety specify that professional qualification must include competences referred to IH.66–68 This also applies to nursing staff.69 In the international setting, the National Quality Forum,70 the Joint Commission,71 the Accreditation Council for Graduate Medical Education and the European Handover Group72 recommend the implementation of training programs to secure the competences needed to manage IH with efficacy.73 Unfortunately, very few universities include IH in their curriculum.74
The best specific training model for this complex task has not been defined to date.75 Since many approaches are possible, clinical simulation could play a key role, since it allows critical reflection in a safe environment, without exposing patients to the risks inherent to training processes.16,76,77 In fact, it also may be considered that training in these competences should extend beyond the strict limits of IH and be complemented by other skills related to teamwork78 and even the resolution of conflicts.79
Final comment and conclusionsInformation handover is a frequent, important and complex task. If not carried out correctly, it can have a marked impact upon the quality of patient care. This affirmation is supported by the growing interest in IH reflected by the literature. Nevertheless, many attempts to systematize IH have not directly resulted in improved patient prognosis; apart from underscoring the complexity of our specialty, this fact points to the need for further organized research efforts (adopting a multidiscipline and multicenter approach) in this setting, which undoubtedly will prove to be complex. This is easy to intuit, especially when considering the growing importance of clinical information systems. For this reason, the Planning, Organization and Management Group of the SEMICYC has considered the development of these recommendations and has launched the TRINEC (Information Handover in the Critical Patient) study with the purpose of knowing how information handover is made in Spanish ICUs.
As a general conclusion, we feel that it is advisable to create a structured process for the IH modalities considered to be most relevant, with adequate identification of the leader. Structuring, through the use of mnemonic tools, is useful but must be accompanied by the narrative approach, which adds enriching nuances to IH. Different types or modalities of IH are required during patient transfer. At discharge from the ICU, the discharge information can serve as a support for communication at the patient bedside between the ICU physician and the physician of the destination Department. Nurses play a crucial role in this process. In the case of emergency situations, we need to apply specific communication standards. The participation of patients and their caregivers is an important challenge. Finally, both the measurement of quality and training in IH are two pending issues in this setting.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sirgo Rodríguez G, Chico Fernández M, Gordo Vidal F, García Arias M, Holanda Peña MS, Azcarate Ayerdi B, et al. Traspaso de información en Medicina Intensiva. Med Intensiva. 2018;42:168–179.