To describe the prevalence of patients with mental disorders (MD) admitted to the ICU. To compare the clinical characteristics according to the presence of psychiatric history. To review the relevance of the consultations made to Psychiatry.
DesignRetrospective descriptive study.
SettingICU of the General Hospital of the Parc Sanitari Sant Joan de Deu, Sant Boi de Llobregat, Barcelona, Spain.
PatientsPatients admitted between January 2016 and June 2018.
InterventionsNone.
Main variables of interestSeverity level (APACHE II), reason for admission, days of admission, days of mechanical ventilation, psychiatric history and reason for psychiatric consultation.
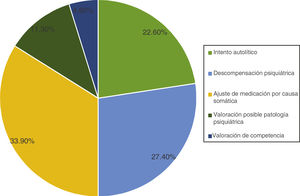
ResultsA total of 1,247 patients were included; 194 (15.5%) met MD criteria, their mean age being younger (59 vs 68, P < .001) and with a lower mean score on the APACHE II scale (12 vs 14, P ≤ .003). There were 64 consultations to Psychiatry (5.1% of admissions), 59 of which were in patients with TM (92.1%). Regarding the reasons for the consultation, 22.6% were for attempted suicide, 61.3% for pharmacological adjustment, 11.3% to rule out mental disorder, and 4.8% for competence assessment. The probability of a consultation being carried out while it was indicated was 89.1%, while the probability of not carrying it out when it was not indicated was 99.4%.
ConclusionsThis study supports the need to expand the specific recommendations for consultation to Psychiatry, beyond the assessment after a suicide attempt, since a large percentage (77.5%) of the pertinent consultations were for other reasons.
Determinar la prevalencia de pacientes con trastorno mental (TM) ingresados en UCI. Comparar las características clínicas según la presencia de antecedentes psiquiátricos. Revisar la pertinencia de las interconsultas realizadas a psiquiatría.
DiseñoEstudio descriptivo retrospectivo.
ÁmbitoUCI del Hospital General del Parc Sanitari Sant Joan de Déu, Sant Boi de Llobregat, Barcelona, España.
PacientesPacientes ingresados entre enero de 2016 y junio de 2018.
IntervencionesNinguna.
Variables de interés principalesNivel de gravedad (APACHE II), motivo de ingreso, días de ingreso, días de ventilación mecánica, antecedentes psiquiátricos y motivo de interconsulta a psiquiatría.
ResultadosSe incluyeron 1.247 pacientes. 194 (15,5%) cumplían criterios de TM, siendo su media de edad más joven (59 vs 68, p < 0,001) y con menor puntuación media en la escala APACHE II (12 vs 14, p ≤ 0,003). Se realizaron 64 interconsultas a Psiquiatría (5,1% de los ingresos), 59 de las cuales fueron en pacientes con TM (92,1%). En cuanto a los motivos de la interconsulta, 22,6% fue por intento autolítico, 61,3% para ajuste farmacológico, 11,3% para descartar trastorno mental y un 4,8% para valoración de competencia. La posibilidad de que se realizara una interconsulta estando indicada fue del 89,1%, mientras que la posibilidad de no realizarla no estando indicada fue del 99,4%.
ConclusionesEste estudio respalda la necesidad de ampliar las recomendaciones específicas para realizar interconsulta a Psiquiatría, más allá de la valoración tras intento autolítico, puesto que un gran porcentaje (77,5%) de las interconsultas pertinentes fueron por otros motivos.
Mental disorder (MD) is a common entity in the overall population. Its prevalence is around 20%,1 and it is associated with a tremendous loss of quality of life, a higher mortality rate, and a long length of stay.2 The WHO estimates that by 2030 depression will become one of the three leading causes of disability among the population, together with HIV and cardiovascular disease.3
In hospitalized patients, this prevalence is much higher up to rates between 12% and 60%.4–8 However, it is hard to define what is considered a metal condition in this specific population since some physical and psychiatric symptoms often overlap. These high numbers of prevalence contrast with the low rate of psychiatric referrals recommended in these patients, nearly 2.2% in Spanish hospitals.9 The most common types of demands from physicians who perform these consultations are: diagnostic or therapeutic collaboration, organization of hospital discharge for ongoing treatment, and transfer to a psychiatric ward.10
There are very few studies available on MD in patients admitted to the intensive care unit (ICU) despite the fact that this comorbidity can worsen the prognosis of critically ill patients.7,11,12 Scientific literature that includes critically ill patients and psychiatric patients basically focuses on psychiatric disorders included in post-ICU syndrome. This syndrome is defined as the appearance of physical, cognitive or mental health worsening in patients admitted to the ICU that persists after hospital discharge.13,14 Back in 2008, Pechlaner et al.15 already emphasized the significant scarcity of evidence available regarding psychiatric disorders at the ICU setting. They mention that both the epidemiology and impact of psychiatric disorders on critical conditions is still very uncertain and indefinite, and that close collaboration between intensivists and psychiatrists benefits not only scientific advancement but also patient care. Knowing the negative impact that ICU stays can have, it would be important to detect and manage psychiatric symptoms in patients who also have a past medical history of MD.
Intensivists do not have specific training in the assessment and management of people with MD. There is no clear criteria on the specific care these patients should receive at the ICU or in the referrals to the Psychiatry Unit. Only a few studies on these referrals due to confusional syndrome have been published for the assessment of acute poisoning related to substance abuse or autolytic attempts.16 The only specific recommendation given by the Spanish Society of Intensive, Critical and Coronary Unit Medical Care (SEMICYUC) is that psychiatric referrals should happen before the ICU discharge in all patients with autolytic attempts.17
The convenience or appropriateness of psychiatric referrals allows us to assess the quality and functioning of the system. Vaz Leal et al.18 ranked as inappropriate all those psychiatric referrals due to poor interpretation of the patient and his behavior by the treating physician. Categorizing the process of adaptation of the patient to his disease as a psychiatric disorder, his reactions to adverse life experiences or justified complaints against real facts represented 6% of the overall number of non-indicated consultations in this study.
The primary endpoints of this study are to determine the prevalence of MD at the ICU setting, compare the characteristics of patients with psychiatric health records to those without them, and review the appropriateness of the psychiatric referrals recommended by the ICU team. To this end, a list of psychiatric referral criteria at the ICU setting has been achieved by consensus from our team. This consensus should be a proposal of the possible appropriate criteria that can serve as a guide for intensivists and improve the management of these patients.
Material and methodThis was a retrospective study of patients admitted from January 1 2016 through June 30 2018 to the ICU of Hospital General del Parc Sanitari Sant Joan de Déu, in Sant Boi de Llobregat, Barcelona, Catalonia, Spain. The general hospital has 200 beds, and each unit has a total of 6 beds: 2 for critically ill patients, and 4 for semi-critically ill patients. It occurs that it is part of a larger health complex that includes 448 beds for psychiatric patients. Also, it is the reference center for Benito Menni Complex Assitencial, a psychiatric center with 600 beds located in the same population. In the Discussion below this will be considered as one of the study limitations since the special characteristics of this center complicate the full extrapolation of data to other centers. However, we consider that these characteristics add value to the data obtained. All patients over 18 admitted to the ICU during the aforementioned period were included in the study. They were classified based on their past medical history of MD or lack of it as we’ll be seeing next.
The study was approved by the CREC with code no. PIC-161-18 on October 25, 2018.
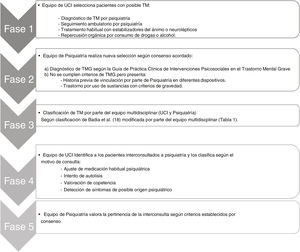
All the health records from patients admitted to the ICU were manually reviewed through a series of 5 different stages (Fig. 1).
Stage 1. ICU review of all patients admitted during the said periodAt this stage, the early screening of the overall sample of patients was conducted by selecting only those with a possible MD. This group included patients whose hospital discharge reports included any of the following items:
- •
Diagnosis of a MD by a psychiatrist.
- •
Psychiatric follow-up.
- •
Presence of mood stabilizers or neuroleptic drugs as part of the patient’s routine treatment plan.
- •
Organ repercussions due to drug or alcohol abuse.
At this stage, the psychiatric team purified once again the sample previously selected using a more restrictive and specific criterion of psychiatric history achieved by consensus based on experience, the routine clinical practice, and a review of the medical literature available to this date.
Psychiatric history was defined by consensus the following way:
- a
Diagnosis of severe mental disorder (SMD).19 Different definitions exist. However, the one provided by the Clinical Practice Guidelines on Psychosocial Interventions in Severe Mental Illness was used here. Diagnosis is achieved based on 3 different dimensions: clinical signs, duration, and degree of functional disability occurred. Regarding the clinical dimension certain psychiatric diagnoses were included with presence of positive and negative psychotic symptoms, a severely altered pattern of relations, and an improper behavior to context or serious inappropriate affection involving a distorted perception of reality. Regarding the time dimension, patients with disorders of 2-year evolution or significant progressive functional impairment over the last 6 months were included. Finally, patients with moderate or serious disease-related complications regarding personal, familial, working, and social functioning were included as well.
- b
Lack of diagnosis of SMD but presence of some of the following criteria:
- ○
History of being associated to the program of Primary Care and Mental Health Support Program (PSP), a Mental Health Center (MHC), psychogeriatrics or psychiatry specialized in intellectual disabilities.
- ○
Disorder due to use of substances in the following cases:
- •
Associated with a Substance Abuse and Mental Health Center (SAMHC)
- •
Cases in which attempts would have been made to refer the patient to the SAMHC.
- •
Consumption with organ damage (liver cirrhosis, gastroesophageal varices, pancreatitis, ascites).
- •
Behavioral or legal issues.
- •
Elevated alcohol use with respect to the SDU (standard drink unit) considered harmful (>8 SDUs in men/6 SDUs in women).
- •
Detection of abstinence symptoms during the ICU stay.
- •
- ○
The multidisciplinary team categorized the group of patients with a past medical history of MD into 3 diagnostic categories: acute poisoning, autolytic attempt, and MD disorder associated with the main diagnosis. The latter was subdivided into 6 different groups:
- •
Substance-related MD.
- •
Psychotic drugs-related MD (including bipolar disorder with psychotic symptoms).
- •
Mood disorder-related MD.
- •
Anxiety disorder-related MD.
- •
Personality disorder-related MD.
- •
Impulse control disorder-related MD.
In the presence of more than 1 single diagnosis in a patient, the most serious one was selected (Table 1).
Categorization of mental disorders based on Badia et al.20
| 1. Acute poisoning | |
| 2. Autolytic attempt | |
| 3. Associated mental disordera | 1. Substance-related MD |
| 2. Diagnosis of schizophrenia and other psychotic disorders (including bipolar disorder with psychotic symptoms) | |
| 3. Mood disorders | |
| 4. MD with anxiety disorders | |
| 5. Personality disorders | |
| 6. Impulse control disorders |
This categorization was based on the only previous model of MD classification at the ICU setting that is specified in an article published by Badia et al.20 regarding data comparisons. However, in this study the third diagnostic category has inclusion characteristics that are different from ours considering MD in all those patients with psychiatric follow-up and diagnosed based on DSM-IV-TR. Also, only the first 4 subgroups are distinguished here.
Stage 4. Identification of patients referred for psychiatric consultation during their ICU stay based on 4 reasons regarding referral recommendations- a
Adjustment of routine psychiatric medication due to:
- ○
Change of psychiatric signs during the ICU stay
- ○
Somatic clinical signs that complicate the administration of the patient’s standard medication.
- ○
- b
Autolytic attempt.
- c
Competence assessment.
- d
Detection of symptoms compatible with psychiatric disease.
The psychiatric team reviewed the past medical history of patients selected with a history of MD to assess the proper indication for psychiatric referral. The course of the somatic illness, psychiatric disorders, and disease progression were taken into consideration. The Psychiatry Unit reached the following consensus based on the indications for referrals.
- a
Indicated referrals:
- ○
SMD with a of complex course of medication and/or clozapine for its adjustment or reintroduction.
- ○
SMD with symptoms of decompensation or chronic symptoms of severity.
- ○
SMD with comorbid confusional syndrome to perform differential diagnosis
- ○
Acute confusional syndrome of difficult pharmacological management
- ○
Autolytic attempt before admission to hospital floor
- ○
Anxiety-depression symptoms interfering with the ICU treatment (eg, intake refusal, emotional liability, severe anxiety, resistant insomnia, etc.)
- ○
Assessment of mental competence in complex cases or with a psychiatric history.
- ○
Disorder due to newly detected severe substance abuse (appearance of abstinence symptoms at the ICU without any past medical history reported, abuse-related medical complications) without any previous association with PSP or drug addiction centers.
- ○
- b
Non-indicated referrals:
- ○
SMD admitted to the ICU with stable non-complex medication and psychopathological stability.
- ○
Medical complications during the ICU stay that prevent assessing the patient’s mental state (orotracheal intubation, elevated sedation…)
- ○
Acute confusional syndrome of typical characteristics and routine management.
- ○
Known disorder due to known substance abuse with abstinence-related symptoms.
- ○
Disorder due to substance abuse associated with PSP or Psychiatry Unit with proper follow-up.
- ○
Anxiety-depression symptoms that do not interfere with the treatment administered at the ICU.
- ○
The following variables were collected from hospitalized patients:
- •
Level of severity (APACHE II).
- •
Length of stay at the ICU.
- •
Past medical history of psychiatric disorders.
- •
Days on invasive mechanical ventilation.
- •
Reason for admission.
- •
Destination at discharge.
- •
Application of mechanical contention due to agitation.
- •
Psychiatric record.
- •
Reason for psychiatric referral (if this ever took place).
Data was treated according to current legislation.
Statistical analysis was conducted using the IBM SPSS Statistics v21 software package. The normal distribution of the variables was assessed using Kolmogorov-Smirnov test. Data is expressed as means and standard deviations for continuous variables with normal distribution, and medians and interquartile ranges (25%–75%) for continuous variables without normal distribution. Continuous variables were compared using the Student t test or the Mann-Whitney test depending on whether distribution was normal or not. Categorical variables were compared using the chi-square test. The ANOVA test was used for repeated measurements. P values <.05 were considered statistically significant.
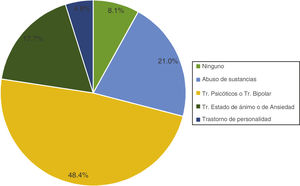
ResultsThere was a total of 1247 ICU admission with a mean age of 67 years-old during the study period (SD = 6). In a first assessment conducted by intensivists, a total of 363 patients (29.1%) with possible MD were included. In the second assessment data was cleaned until a total de 194 patients (15.5%) with a history of MD were found. A total of 64 psychiatric referrals were advised (5.1% of all admissions). The most common psychiatric disorder in patients with referrals was psychosis or bipolar disorders (48.4%) followed by substance abuse (21%), and mood changes (17.7%). A total of 8.1% of the patients recommended for referrals had no psychiatric history of MD whatsoever (Fig. 2).
Table 2 shows the social, demographic, and clinical characteristics of patients studied based on the reason for admission, severity based on the APACHE II score, days on invasive mechanical ventilation or type of discharge based on the presence, or not, of a psychiatric medical history. The mean age of patients with a past medical history of MD was 59 years of age (SD = 14) vs 68 (SD = 16) from the patients of control group (P < .001). The main reason for admission in patients with MD was respiratory failure (25.3%) while the most common cause for admission in patients without MD was a heart condition (40.4%). The level of severity reported according to the APACHE II score was lower in patients without MD with a mean of 12 (SD = 7) vs 14 (SD = 8) without any significant differences being reported (P < .003). Invasive mechanical ventilation was more commonly used in patients with MD (P < .001) although no significant differences were found regarding days on IMV.
Social, demographic, and clinical characteristics of the patients.
| Overall | No MD | MD | ||
|---|---|---|---|---|
| N = 1247 | N = 1053 | N = 194 | P | |
| Age (years) | 67 ± 16 | 68 ± 16 | 59 ± 14 | <.001 |
| APACHE II score | 12,1 ± 7,2 | 12 ± 7 | 14 ± 8 | .003 |
| IMV (%) | 15% (188) | 11% (139) | 4% (49) | <.001 |
| Days on IMV | 4 ± 4 | 5 ± 0.4 | 3.9 ± 0.6 | .527 |
| ICU stay (days) | 3 ± 8 | 8 ± 0.2 | 6.4 ± 0.5 | .408 |
| Reason for admission | Percentage (N) | |||
|---|---|---|---|---|
| Cardiovascular | 37% (458) | 40.4% (425) | 17.5% (34) | <.001 |
| Respiratory failure | 17% (206) | 15% (159) | 25.3% (49) | .001 |
| Emergency postoperative period | 12% (148) | 12.5% (132) | 8.2% (16) | .092 |
| Scheduled postoperative period | 8% (94) | 8.1% (85) | 4.1% (8) | .054 |
| Sepsis | 7% (89) | 7.6% (80) | 4.6% (9) | .141 |
| Digestive | 5% (56) | 3.9% (41) | 7.7% (15) | .018 |
| Neurologic | 3% (42) | 2.7% (28) | 7.2% (14) | .001 |
| Trauma-related | 3% (38) | 3% (32) | 3.1% (6) | .968 |
| Drug poisoning | 2% (20) | 0.2% (2) | 9.3% (18) | <.001 |
| CPR | 1% (17) | 0.9% (10) | 3.6% (7) | .003 |
| Non-drug poisoning | 0.2% (3) | 0% (0) | 1.5% (3) | <.001 |
| Other | 6% (74) | 5.6% (59) | 7.7% (15) | .249 |
| Death | 6% (78) | 6.3% (66) | 6.2% (12) | .97 |
| Contention | 6% (76) | 5.3% (56) | 10.3% (20) | .013 |
| Psychiatric referrals | 5% (64) | 0.6% (6) | 30% (58) | <.001 |
A total of 59 (92.1%) out of the 64 psychiatric referrals recommended in patients admitted to the ICU had a psychiatric history of MD. Fig. 3 shows how the reasons for psychiatric referrals were distributed in the study sample. In our sample, 89.1% of all psychiatric referrals (N = 57) were properly requested by the psychiatric team unlike the 10.9% of them (N = 5). On the other hand, no psychiatric consultation occurred if not indicated in 99.4% (N = 1185) while no psychiatric assessment was requested when actually needed in 0.6% of the cases (N = 69).
The reasons that justified non-indicated referrals were to response to anxiety syndromes or because the patient had been put on previous medication by other mental health professionals. The reasons that justified the indicated referrals were to adjust the medication due to worsening psychiatric disorder during the ICU admission, and to treat confusional syndrome in patients with MD.
DiscussionIn this study there is a 15.5% prevalence of mental disorders at the ICU setting. Two similar studies were found on the prevalence of MD at the ICU setting. Patients with MD had higher APACHE II scores without any differences being found in the mortality rate reported. Psychiatric referrals occurred in 5.1% of the overall number of patients.
A stage-based methodology was used for a consistent analysis of the history of MD. After an initial review that only included the ICU discharge report many patients without a history of MD were excluded compared to those with more comprehensive assessments to confirm whether such diagnosis would have been achieved by a specialist or that the patient would have been treated with some type of therapy at a mental health cent at that time or in the past.
In their series of cases, Suchyta et al.7 found a 19% prevalence of previous MD and a 19% prevalence of substance abuse without specifying the percentage that both medical histories presented in a series of 742 critically ill patients. Badia et al.20 found a 7.8% prevalence in their series of 1860 patients. Such variable results can be associated with the review method of the patients since the three of them were retrospective studies or the units where they were conducted had different characteristics.
Regarding the characteristics of the population with MD compared to the group without such a medical history, no significant differences were found regarding the days on mechanical ventilation or mortality as in the study conducted by Badia et al.20. The level of severity at admission (measured using the APACHE II score) was significantly higher in patients with MD as reported by other series.7 What is surprising is that no mortality differences were reported. A clinical history of MD reportedly increases mortality rate as it was confirmed in the study conducted by Suchyta et al.7 However, some of the patients included in their series were trauma patients due to the special characteristics of such unit. The fact that a higher APACHE II score was not associated with a higher mortality rate in our patients or in those from the study conducted by Badia et al.20 can be due to the size of the sample or to an excessive penalization of the level of conscience in such score for this group of patients, especially those with acute poisoning. Patients with MD were significantly younger compared to those without MD, which is consistent with former studies.12,21 Regarding the ICU stay (days), no significant differences were reported in our series unlike the study conducted by Badia et al.20 where the ICU stay was shorter in patients with MD. We believe that this difference can be due to the fact that over 60% of the patients from their series were admitted due to autolytic attempts or acute poisonings with mean shorter stays compared to patients admitted with somatic conditions and associated MD. The most common reason for ICU admission in the group of patients with MD was respiratory failure while cardiac causes were the most common cause for admission in the group of patients without a medical history of MD. This piece of information has not been compared with other series.
Referrals were recommended in 5.1% of all ICU patients. In their series, Sánchez-González et al.9 found an in-hospital psychiatric referral rate of 2.2%. In other series, this rate is between 0.7% and 5%.21–26 We believe that the large number of referrals from the ICU is due not only to the ongoing collaboration with the Psychiatry Unit, but also to the large number of psychiatric patients hospitalized. The rate of referrals in patients with a past medical history of MD only was 30%, much lower compared to that reported by Badia et al.20 (32.9%).
Five different reasons for psychiatric referral were found: medication adjustment due to somatic disease, medication adjustment due to causes attributed to the underlying psychiatric disease, assessment of autolytic attempts, assessment of underdiagnosed possible MD, and assessment of competence. This certainly widens the only recommendation made by SEMICYUC on referrals in cases of autolytic attempts before patient release to the hospital ward. Vaz Leal et al.18 describe that, in general, the main factors that trigger psychiatric referrals from the hospital ward are the existence or absence of psychopathological disorders detectable when the referral was proposed; the existence or absence of psychopathological traits in the patient’s health record, and the presence or absence of psychopathological disorders at the time of admission. In a study conducted by the European Consultation-Liaison Working Group25 among 56 general hospitals from 11 different countries for a total of 3608 patients the most common reasons for requesting in-hospital psychiatric referrals were psychiatric symptoms (50%), unexplained physical symptoms (15%), substance abuse (9%), past medical history of MD (8.5%), assessment of suicidal ideas (6%), and coping behaviors regarding medical-surgical disease (5.8%). These factors are not exactly consistent with our help request to control psychiatric symptoms, assess substance abuse or the patient’s medical history of MD for the sole purpose of regulating medication.
Regarding the rate of indicated referrals, we found no former studies for comparison purposes. Overall, data shows that the chances of referral actually taking place when indicated were high (89.1%) while the chances of having requested them when not indicated were 10.9% Although the number of patients not referred for psychiatric consultations who would have needed to be referred was 1%, this result is biased due to the low number of referrals recommended in the overall population (5.1%). In these cases, it was considered that referrals should have been recommended for being patients with a medical history of MD and symptoms of agitation during their ICU stay. Given the actual context and knowing about confusional syndrome, referrals should be recommended in the presence of these symptoms in this group of patients.
The main study limitation is that it was conducted in one single ICU and with specific characteristics that affected patients with psychiatric past medical histories: a small ICU part of a complex hospital that provides healthcare to a much larger population compared to psychiatric patients and, therefore, with special sensitivity from ICU professionals regarding MD on top of a close collaboration with the Psychiatry Unit. Therefore, data cannot be extrapolated to other centers. However, we believe that data also adds value to the results given the special healthcare provided to this type of patients.
Another study limitation was that the indication, or not, for patient referral was only reviewed in patients with a history of MD, which means that maybe there were indicated referrals that were never performed on patients without such a history. Also, it is a retrospective study meaning that it was based on clinical history reviews with the corresponding loss of information.
Data from this study support the need for expanding the set of specific recommendations to carry out psychiatric referrals in ICU patients beyond the sole assessment of autolytic attempts prior to ICU discharge since, in a large percentage (77.5%) of appropriate referrals are due to several reasons. Further studies would be needed to handle the indication for psychiatric referrals from the ICU setting much better.
AuthorsAll authors made substantial contributions to this study. All authors agree on the content of this manuscript.
Conflicts of interestNone reported.
Please cite this article as: Fernández Trujillo A, López Ortiz C, Cuñat Rodriguez O, del Hoyo Buxo B, Parrilla FJ, Serrano-Blanco A, et al. Antecedente de trastorno mental en la UCI e interconsulta a psiquiatría. Med Intensiva. 2022;46:559–567.