To evaluate a new organizational model in an intensive care unit, with the implementation of early warning systems and a support unit.
DesignA retrospective, comparative cohort study was carried out.
SettingThe study was carried out in the Department of Intensive Care Medicine (DICM) of a tertiary hospital (2009–2011), with the comparison of three time periods (P1, P2 and P3) that differed in terms of organization and logistics.
PatientsWe analyzed all patients admitted to the ICU during the study period. Patients from maternal and infant intensive care were excluded.
Variables of interestPercentage of patients with stays of under two days, with invasiveness used; readmission to the DICM, type of admission and percentage of stays of longer than one month; APACHE II score, mean stay in the ICU and shift distribution of the admissions.
ResultsWe analyzed a sample of 3209 patients (65% males), with a mean age of 58.23 (18.23) years, a mean APACHE II score of 16.67 (8.23), and presenting an occupancy rate of 7.3 (10.3) days in the analyzed period.
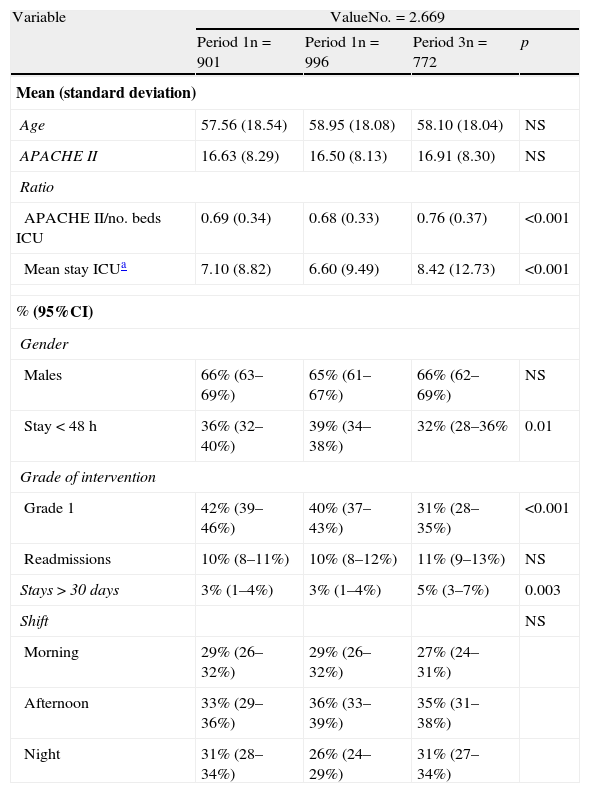
The ratio APACHE II score/number of beds was 0.69 (0.34) in P1, compared to 0.68 (0.33) in P2 and 0.76 (0.37) in P3 (p<0.001). The intervention surveillance grade (grade 1) was 42% (39–46%) in P1, 40% (37–43%) in P2 and 31% (28–35%) in P3 (p<0.001). The average stay in the ICU ranged from 7.10 days (8.82) in P1 to 6.60 days (9.49) in P2 and 8.42 days (12.73) in P3 (p<0.001).
ConclusionsThere has been an increase in the number of patients seen in our DICM, with a decrease in the patients admitted to the conventional ICU. Patients now admitted to the ICU are more seriously ill, require a greater level of intervention, and give rise to an increase in the mean duration of stay in the ICU.
Evaluar un nuevo modelo organizativo en un servicio de Medicina Intensiva, con la puesta en marcha de servicio extendido y unidad de apoyo.
DiseñoEstudio de cohortes retrospectivo, comparativo.
ÁmbitoEl estudio se realiza en un SMI de un hospital de tercer nivel (2009-2011). Comparando 3 periodos de tiempo (P1, P2 y P3) deferentes en cuanto a organización y logística dentro nuestro SMI.
PacientesSe analizan todos los enfermos que ingresan en el SMI, durante el periodo de estudio. Se excluyen los pacientes del área de cuidados intensivos materno infantil.
Variables de interésPorcentaje de enfermos con estancias menores de 2 días, invasividad empleada en los enfermos; reingreso en el SMI, el tipo de ingreso y el porcentaje de estancias superiores a un mes; APACHE II, las estancias medias en la UCI y la turnicidad de los ingresos.
ResultadosAnalizamos una muestra de 3.209 enfermos; La edad media fue de 58,23 (18,23), con un APACHE II medio de 16,67 (8,23), siendo el 65% varones y presentando una estancia media de 7,3 (10,3) días en el periodo analizado.
El ratio APACHEII/número de camas fue de 0,69 (0,34) en P1, frente a 0,68 (0,33) de P2 y 0,76 (0,37) en P3 (< 0,001). El grado de intervención de vigilancia (Grado 1) fue del 42% (39-46%) en P1, 40% (37-43%) en P2 y 31% (28-35%) en P3 (< 0,001). La estancia media en UCI varió de 7,10 días (8,82) en P1, 6,60 días (9,49) en P2 y 8,42 días (12,73) en P3 (< 0,001).
ConclusionesSe ha producido un aumento del número de pacientes atendidos por nuestro SMI, con un descenso de pacientes que ingresan en las UCI convencionales. Los enfermos que ingresan ahora en la UCI son enfermos más graves, requieren un nivel de intervención mayor y ocasionan un aumento de la estancia media en la UCI.
Different studies have shown that an important proportion of the patients admitted to conventional hospital wards do not receive the best possible care before requiring admission to the Intensive Care Unit (ICU). On the other hand, in an important number of cases admission to the ICU potentially could have been avoided.1–3 Risk identification and quantification in the seriously ill patient, and particularly its grading and the consequent appropriate patient assignment within the hospital setting, should be carried out by the professionals that are most familiarized with patients of this kind, i.e. intensivists.4,5
Within the specific context of our hospital, the intensivists for a number of years have been aware of the important difference between the care received by patients in the ICU and the care received by these same patients when admitted to hospital wards.6
With the purpose of improving patient grading and care, and in sum of offering patients the best care adjusted to their needs, our Department of Intensive Care Medicine (DICM) began to plan its reorganization in the year 2009, culminating in 2011 with the creation and inauguration of a small Intermediate Care Support Unit (ICSU).
In June 2009 our hospital inaugurated what is currently known as an Extended Intensive Care Service (EICS). Its implantation was carried out in several phases: a first EICS project development phase; a second activation criteria definition phase; a third personnel training and reorganization phase, with diffusion among the implicated services; a fourth initial operative and periodic evaluation phase; and finally a fifth phase that closed the intensive care extension project with the coming into service (in October 2010) of the aforementioned Intermediate Care Support Unit (ICSU).6
At present, with stable functioning of the EICS and ICSU, we have carried out a study to analyze the impact of this new model in our DICM. To this effect, we have evaluated the observed variations in tendency referred to “inappropriate” admissions, patient care grading, and the impact of the model in daily clinical practice.
Patients and methodsDesign: A retrospective study has been made of data collected at the time of discharge from the DICM or patient death.
Setting: A third level reference university hospital with approximately 900 beds. The DICM currently is physically differentiated into four areas:
- (a)
Ward “A” of the General Intensive Care Unit (GICU-A): 10 boxes for polyvalent clinical cases, general surgery postoperative patients and specialty surgical cases, as well as liver and pancreas transplant patients.
- (b)
Ward “B” of the General Intensive Care Unit (GICU-B): 12 beds for neurological critical cases, polytraumatized patients and lung transplant and specialty surgery postoperative patents.
- (c)
Maternal-children's ICU: 6 beds for polyvalent clinical pediatric and gynecological patients. Due to its organizational, physical and patient clinical characteristics, this unit is not considered in the present study.
- (d)
Intermediate Care Support Unit (ICSU): 4 recently established boxes for non-critical seriously ill patients (excluding mechanical ventilation, patients requiring isolation measures, and renal replacement techniques).
The data study period corresponding to the patients admitted to our DICM extended from July 2008 to 25 October 2011. This period in turn was divided into three time categories to the effects of posterior analysis:
- (1)
Period 1 (P1): An analysis was made of the records of the patients admitted to the DICM between 15 July 2008 and 15 July 2009. In this period of time the DICM was characterized by stable functioning of the GICU-A (equipped with 12 boxes in this period) and GICU-B.
- (2)
Period 2 (P2): Between 24 October 2009 and 24 October 2010. In this period, and in addition to the GICU-A and GICU-B, the EICS was operational, though without the ICSU.
- (3)
Period 3 (P3): Between 25 October 2010 and 25 October 2011. During this period our DICM was operational with the GICU-A (10 boxes), GICU-B, EICS and ICSU.
Patients: All admissions to the DICM during the indicated time periods were recorded on a consecutive basis. We excluded maternal-pediatric admissions to the ICU, as well as patients admitted to the DICM for the conduction of invasive procedures (central venous catheter placement, chest drainage, etc.), and which implied a stay of under 24h.
Patients of the cardiological critical care unit (the old coronary ICU previously ascribed to our DICM) were likewise not analyzed.
Method: The following variables were recorded:
- I.
Demographic data: Age and gender.
- II.
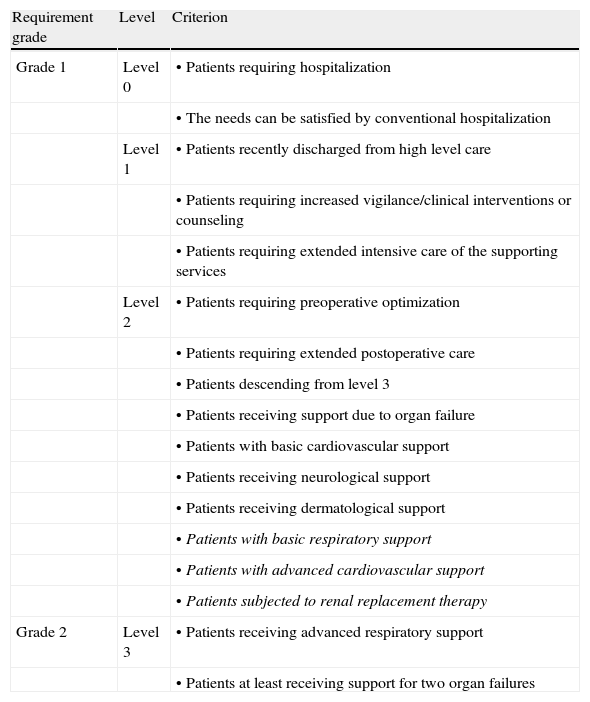
“Inappropriate” ICU admission trend variables: Modification of the percentage of patients with stays of under 48h, and variations in patient requirements (Table 1):
- a.
Grade 1 was taken to represent patients pertaining to level 1 and level 2 according to the standards and guides of the International Critical Care Society.7 We excluded from level 2 those patients with basic ventilatory assist requirements, basic or advanced cardiovascular support needs, and the use of renal replacement therapy.
- b.
Grade 2 was taken to represent patients of level 2 with basic ventilatory assist requirements, basic or advanced cardiovascular support needs, and the use of renal replacement therapy, together with patients pertaining to level 3 according to the standards and guides of the International Critical Care Society.
Table 1.Grading of the patients in our DICM according to the standards and guides of the International Critical Care Society.
Requirement grade Level Criterion Grade 1 Level 0 • Patients requiring hospitalization • The needs can be satisfied by conventional hospitalization Level 1 • Patients recently discharged from high level care • Patients requiring increased vigilance/clinical interventions or counseling • Patients requiring extended intensive care of the supporting services Level 2 • Patients requiring preoperative optimization • Patients requiring extended postoperative care • Patients descending from level 3 • Patients receiving support due to organ failure • Patients with basic cardiovascular support • Patients receiving neurological support • Patients receiving dermatological support • Patients with basic respiratory support • Patients with advanced cardiovascular support • Patients subjected to renal replacement therapy Grade 2 Level 3 • Patients receiving advanced respiratory support • Patients at least receiving support for two organ failures - a.
- III.
Critical patient care grading variables: Readmission to the DICM and the percentage of stays lasting over one month.
- IV.
Daily clinical practice management effect variables: Variations in patient severity (Acute Physiology and Chronic Health Evaluation: APACHE II; and APACHE II/number of beds ratio), mean stay and timing (shifts) of the admissions.
Statistical analysis: A descriptive statistical analysis was made of the global cohort and of each of the sub-cohorts, according to the time period evaluated. Continuous variables are reported as the mean±standard deviation (SD), while categorical variables are reported as percentages with the corresponding 95% confidence interval (95%CI). The comparative statistical analysis was based on analysis of variance (ANOVA) for the comparison of mean values between the patient sub-cohorts. Categorical variables in turn were compared using the chi-squared test.
The statistical analysis was carried out using the MedCalc® 11.4.2.0 statistical package.
ResultsDescriptive statistics: We analyzed the records of 2669 patients admitted to the ICU during the indicated period of time, and 540 patients admitted to the ICSU.
The mean age (SD) of the patients admitted to the ICU during the overall study period was 58 years (18.23), with a mean APACHE score of 16.66 (8.23) and a mean stay of 7.29 (10.36) days. Sixty-five percent of the patients were males, and 55% presented chronic disease. The global mortality rate during the study period was 18%.
Comparative statistics: The variables analyzed in each period of the study are shown in Table 2.
Principal variables of the analyzed patient cohort, according to the different time periods.
| Variable | ValueNo.=2.669 | |||
| Period 1n=901 | Period 1n=996 | Period 3n=772 | p | |
| Mean (standard deviation) | ||||
| Age | 57.56 (18.54) | 58.95 (18.08) | 58.10 (18.04) | NS |
| APACHE II | 16.63 (8.29) | 16.50 (8.13) | 16.91 (8.30) | NS |
| Ratio | ||||
| APACHE II/no. beds ICU | 0.69 (0.34) | 0.68 (0.33) | 0.76 (0.37) | <0.001 |
| Mean stay ICUa | 7.10 (8.82) | 6.60 (9.49) | 8.42 (12.73) | <0.001 |
| % (95%CI) | ||||
| Gender | ||||
| Males | 66% (63–69%) | 65% (61–67%) | 66% (62–69%) | NS |
| Stay<48h | 36% (32–40%) | 39% (34–38%) | 32% (28–36% | 0.01 |
| Grade of intervention | ||||
| Grade 1 | 42% (39–46%) | 40% (37–43%) | 31% (28–35%) | <0.001 |
| Readmissions | 10% (8–11%) | 10% (8–12%) | 11% (9–13%) | NS |
| Stays>30 days | 3% (1–4%) | 3% (1–4%) | 5% (3–7%) | 0.003 |
| Shift | NS | |||
| Morning | 29% (26–32%) | 29% (26–32%) | 27% (24–31%) | |
| Afternoon | 33% (29–36%) | 36% (33–39%) | 35% (31–38%) | |
| Night | 31% (28–34%) | 26% (24–29%) | 31% (27–34%) | |
The variables shift and readmission were studied more in depth:
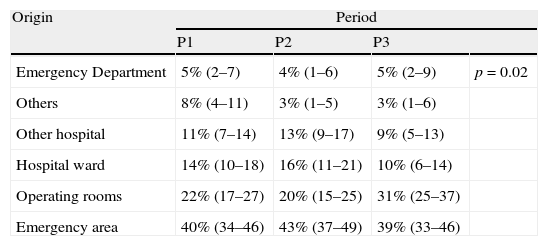
The admissions occurring during the night shift (from 22:00p.m. to 8:00a.m. of the following day) did not vary in percentage terms during the three periods, though the origin of admission was seen to vary significantly: the number of admissions from the hospital wards decreased in P3, accompanied by an increase in the number of admissions from the surgical areas (Table 3).
Variability of the origin of the patients admitted to the ICU during the night shift.
| Origin | Period | |||
| P1 | P2 | P3 | ||
| Emergency Department | 5% (2–7) | 4% (1–6) | 5% (2–9) | p=0.02 |
| Others | 8% (4–11) | 3% (1–5) | 3% (1–6) | |
| Other hospital | 11% (7–14) | 13% (9–17) | 9% (5–13) | |
| Hospital ward | 14% (10–18) | 16% (11–21) | 10% (6–14) | |
| Operating rooms | 22% (17–27) | 20% (15–25) | 31% (25–37) | |
| Emergency area | 40% (34–46) | 43% (37–49) | 39% (33–46) | |
Analysis of readmission in turn showed that up to 11.6% of all readmissions to the ICU during P3 corresponded to patients that were admitted to the ICSU. Likewise, the severity of the patients readmitted to the ICU, as determined from the APACHE II score, showed an increase from 18.1 (7.5) to 19.8 (7.6) on comparing the patients readmitted in P1 versus those readmitted during P3 (p=0.15).
The mean stay in the DICM varied significantly in the three study periods from 7.10 (8.82) days in P1 to 6.60 (9.49) days in P2, and 5.89 (10.29) days in P3 (p=0.009).
The ICU occupation index increased significantly from 73% in P1 to 81% in P3 (p<0.001).
DiscussionThe present study has examined the way in which the introduction of a new model of Intensive Care Medicine in our DICM has modified patient severity variables, grading and care afforded by the intensivists in our hospital. A particularity of the analysis is that it does not contemplate coronary patients, in contrast to the situation found in most intermediate care units.8–13
A number of conclusions can be drawn from the data obtained. Firstly, the functioning of an EICS and the stable inauguration of an ICSU, interacting and operating jointly, have been associated to an increase in the number of patients attended by the DICM. In effect, at present, our DICM attends 45% more patients than four years ago.
This increase in the number of patients attended by our DICM exhibits a series of particularities. In effect, a decrease is observed in the patients admitted to the conventional ICUs; the patients now admitted to the ICU are more seriously ill individuals as evidenced by the APACHE II score/number of available beds ratio, and require a higher level of intervention. This in turn results in a prolongation of the mean stay in the ICU.
We consider that these data are fundamented upon the stable functioning of an ICSU, designed with a profile and a series of characteristics different from those of a conventional ICU, without the feared masked increase in ICU care capacity or utilization as a covert ICU14,15–and with an added reduction in the percentage of “inappropriate” admissions to the ICU. However, in this context it is important to underscore that within the definition of inappropriate admission for stays of under two days we are masking patients who died in the first 48h of admission and patients requiring mechanical ventilation for short periods of time due to drug intoxication or overdose, and which actually correspond to appropriate admissions in a conventional ICU.
On the other hand, Wagner et al.16 reported that up to 45% of all patients admitted to the polyvalent clinical-surgical ICU of a university hospital (corresponding to a structure similar to that of our DICM) could be regarded as patients subjected to vigilance only, and that the risk of iatrogenesis in these cases outweighs the potential benefits of admission to the ICU. Based on these conclusions, we consider the incorporation of an ICSU to our DICM to offer important benefits in reference to patients of this kind. Similar observations have been made by Henning et al.17 These authors, in relation to a polyvalent unit, considered that the DICM should be organized according to patient severity at the time of admission, or the therapeutic effort required at the time. In the same way Nelson,19 using criteria such as admissions for under 24h and the absence of invasive monitorization, considered 32% of the admissions to a surgical ICU to be inappropriate–concluding that these patients could have been better managed in a less costly unit. Murata and Ellrodt20 likewise evidenced that up to 40% of the patients were admitted to an ICU for vigilance purposes only. Lastly, Franklin et al.21 studied the benefits derived from the creation of an ICSU in the context of a polyvalent clinical-surgical unit, and found such a measure to result in a 14.5% decrease in the admission of low risk patients to the polyvalent unit, with improved access on the part of high risk patients, thanks to the greater availability of beds. These observations are consistent with the increase in occupation index experienced in our ICUs, when comparing the three time periods, on the part of more seriously ill patients–as reflected by the variables analyzed.
However, in principle it may seem that the variables which we have analyzed do not illustrate such clarity when speaking of improved patient grading in our DICM. The purported beneficial effect of such grading should result in a lesser percentage of patients readmitted to the DICM.22 This affirmation is based on the possibility of transferring patients from the ICU to the ICSU in the moment when the patient care requirements decrease. In this context, progressive care could be afforded, with optimized transfer to the hospital ward, reducing the number of early discharges and readmissions. In this sense, up to one-third of the readmissions to a DICM23 could have been avoided if early discharge had not been decided. At this point we on one hand wish to underscore that in P3 up to 11% of the readmissions came from the ICSU–a situation logically not seen in P1 and P2, when the ICSU was not yet operational. On the other hand, the origin of the night shift admissions was seen to change, with a significant decrease in the number of patients transferred from hospital wards. We consider that these findings are a consequence of improved grading of the patients attended by the ICSU and EICS.24–26
Recently, our group has reported its data referred to the impact of the implantation of the EICS upon mortality,18 with an almost 5% reduction in fatalities in the ICU during the stable functioning period of the EICS.
We have not conducted a cost–benefit analysis in our Department, though assuming that the personnel costs calculated for a DICM in Spain represents approximately 69% of the total costs,27,28 and taking into account that the reorganization of our Department has been made with the same medical personnel (with no new contracts in the periods P2 and P3), we can accept the existence of cost benefits (lowering of costs due to fewer procedures and laboratory tests29) resulting from introduction of the new model. This becomes all the more patent on considering that the cost of one day of admission to the ICSU is taken to represent one-third of the cost of a day in the ICU.30
We acknowledge the need for analyses affording continuous auditing of the appropriateness of the patients treated in supporting units of this kind, in order not to mask activity as a covert ICU.14,15,31
Conflicts of interestThe authors declare that they have no conflicts of interest.
The authors express their sincere gratitude to the medical and nursing personnel, and the nursing auxiliary personnel, of the DICM of Marqués de Valdecilla University Hospital (Santander, Spain), and particularly to the ICSU personnel, for their work and patience.
Please cite this article as: González-Castro A, et al. Impacto de un nuevo modelo de Medicina Intensiva sobre la asistencia en un servicio de Medicina Intensiva. Med Intensiva. 2013;37:27–32.