To describe the implementation of a Medical Information System (MIS) in the Critical Care Department (CCD).
DesignA prospective observational cohort study was carried out.
SettingClinical and Surgical wards in Son Llàtzer Hospital.
PatientsPatients with criteria of rapid care alert (RCA) without treatment, cardiac arrest (CA), and unexpected ward deaths (UWD), during 2010.
Main variablesAge, sex, nursing shift, nursing alert, vital signs, unplanned admission to intensive care, CA, UWD and death.
ResultsThe MIS detected 9647 episodes with RCA signs in 4020 patients (26.4episodes/day). A total of 8547 episodes were reviewed. Sixty-five patients required rapid response by the intensive care staff; 61.5% were detected in the afternoon shift (15:00–22:00), and 61.5% were admitted to the CCD. Diminished consciousness (DC) and respiratory failure were the most frequent problems. The sepsis rate was 23%. We reviewed 45 CA and 35 UWD. Of the total cases of CA, 33 patients died (73.3%) and 66.7% had criteria of untreated RCA. Monitoring (p<0.05) and rhythms amenable to defibrillation (p<0.002) were associated to survival. As regards the UWD, 75% had criteria of untreated RCA, and 40.6% presented diminished consciousness. In the last 6 months there was a significant reduction in UWD (p=0.01).
ConclusionsThe MIS could be a complimentary tool in the activity of the CCD to improve the prognosis of hospitalized patients.
Describir la implementación de Técnicas de Información y Comunicación (TIC) sobre el Servicio de Medicina Intensiva (SMI).
DiseñoEstudio de cohortes prospectivo observacional.
ÁmbitoHospitalización de Áreas Médicas y Quirúrgicas del Hospital Son Llàtzer.
PacientesPacientes con criterios de alarma de rápida asistencia (ARA) no tratados, paradas cardiacas (PC) y muertes inesperadas en planta (MI) durante el año 2010.
Variables de interés principalEdad, sexo, turno de enfermería, alerta de enfermería, criterios ARA, ingreso en SMI, PC, fallecimiento y MI.
ResultadosEl sistema informático (SI) detectó 9.647 episodios con criterios ARA en 4.020 pacientes (26,4 episodios/día). Se realizaron 8.547 revisiones por el intensivista. Sesenta y cinco pacientes precisaron actuación temprana del SMI. De ellos, el 61,5% fueron detectados en el segundo turno (de 15:00 a 22:00) y el 61,5% ingresó en el SMI. La disminución del nivel de conciencia (DNC) y la insuficiencia respiratoria fueron los más frecuentes. La etiología más frecuente fue la sepsis (23%). Se incluyeron 45 PC y 35 MI. Del total de PC, 33 pacientes fallecieron (73,3%) y el 66,7% presentaron criterios ARA no tratados. La monitorización (p<0,05) y los ritmos desfibrilables (p<0,002) se asociaron a supervivencia. En las MI, el 75% presentaron criterios ARA no tratados y el 40,6% presentaron DNC. En el segundo semestre se observó una reducción significativa de las MI (p=0,01).
ConclusionesLas TIC pueden ser una herramienta complementaria a la actividad asistencial del SMI para mejorar el pronóstico de los pacientes hospitalizados en planta.
Unexpected deaths and cardiac arrest (CA) episodes occurring in hospitals1,2 are often preceded by alarm signs.3,4 Likewise, unprogrammed admissions of hospitalized patients to the Critical Care Department (CCD) are usually preceded by alterations in vital signs that have not been detected and/or registered, and which have not received medical intervention.5,6
It is clear that not all the technology of a CCD can be found in conventional hospital wards, but Medical Information Systems (MIS) currently allow the early detection of certain parameters that identify patients at risk of suffering serious adverse events.
The continuous work burden of Emergency Departments and the increased complexity of patients admitted to hospital are causing a rise in the proportion of admissions of patients at a high risk of developing serious disease susceptible to ulterior admission to the CCD.
Correctly understanding this problem allows us to consider possibilities for interprofessional and multidisciplinary collaboration not only with the medical specialties but also with other professional areas such as communications engineering. In fact, collaboration and coordinated clinical management constitute the basis for guaranteeing care continuity in a patient-centered structure or system. The development of computer programs offers a fast and easy way to detect variables indicative of physiological and laboratory test instability, with a view to detecting possible patients at risk.
The use of Medical Information Systems (MIS) in hospitals aims to improve the outcomes of the healthcare process, placing emphasis on safety and quality. The adoption of tools that allow us to manage the care of such patients can lead to a more efficient distribution of the existing healthcare resources, since they provide us in time with the information needed for optimizing decision making.7
In Son Llàtzer Hospital (Palma de Mallorca, Spain) we attempt to secure the integration of communication technologies for use in healthcare activities, with a view to increasing the quality of patient care and thereby improving survival and lowering the costs.
The main objective of the present study was to describe the implementation of an automatic MIS for detecting rapid care alerts (RCA) in hospitalized patients. Likewise, an analysis was made of the characteristics of the patients with CA and unexpected death.
Materials and methodsStudy designA prospective, observational cohort study was carried out covering the period between 1 January 2010 and 31 December 2010.
Study settingClinical and surgical hospitalization areas.
Study populationAll patients admitted by the Emergency Department were evaluated. The inclusion criteria comprised individuals with criteria of RCA not subjected to treatment (or treated inadequately) and who required early intervention (within 12h following detection) by the Critical Care Department (CCD) (Table 1). In-hospital cardiac arrests and unexpected deaths were also evaluated.
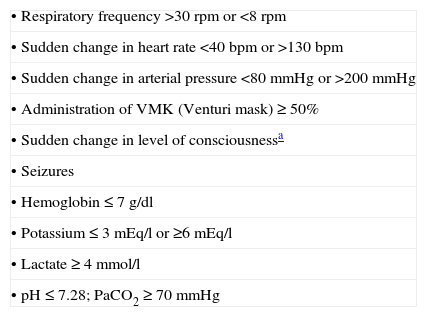
Criteria of RCA activation – Son Llàtzer Hospital.
| • Respiratory frequency >30rpm or <8rpm |
| • Sudden change in heart rate <40bpm or >130bpm |
| • Sudden change in arterial pressure <80mmHg or >200mmHg |
| • Administration of VMK (Venturi mask)≥50% |
| • Sudden change in level of consciousnessa |
| • Seizures |
| • Hemoglobin≤7g/dl |
| • Potassium≤3mEq/l or ≥6mEq/l |
| • Lactate≥4mmol/l |
| • pH≤7.28; PaCO2≥70mmHg |
Patients admitted on a programmed basis for ambulatory major surgery, and patients with criteria of RCA treated adequately by the ward physician, were excluded from the study.
Principal study variablesPatients with criteria of rapid care alert not subjected to treatmentPatient age and gender were recorded, together with the nursing shift during which the event occurred, the nursing alert, the cause and the criteria of RCA. The three nursing shifts comprised the following periods: a first shift from 08:00 a.m. to 15:00 p.m., a second shift from 15:00 p.m. to 22:00 p.m., and a third shift from 22:00 p.m. to 08:00 a.m. on the following day.
Cardiac arrestThe demographic characteristics of the in-hospital cardiac arrests were analyzed. Data collection was carried out following the Utstein guidelines.8
Unexpected deathsEach month an analysis was made of all the deaths occurring in the hospital center, differentiating expected or foreseeable deaths (on the basis of disease evolution) from unexpected ward deaths (sudden death or death occurring as a result of an event that proved unexpected or was influenced by a delay in diagnosis and/or treatment). Among the unexpected ward deaths, avoidable death was defined as an unforeseeable fatality with criteria of RCA not subjected to treatment within the 12h prior to the event, and in which the fatal outcome might have been avoidable if treatment had been provided. These deaths were reviewed by 5 physicians unrelated to the physician in charge of the patient. Classification as avoidable death required agreement among all 5 physicians.
In the case of CA and in unexpected deaths we recorded the criteria of RCA not subjected to treatment that were not adequately detected or evaluated by the CCD or by the ward physician.
Patient consent was not requested, since the study was considered to comprise an emergency clinical situation. The study was approved by the Research Ethics Committee of both the Hospital and the Autonomous Community (Balearic Islands, Spain).
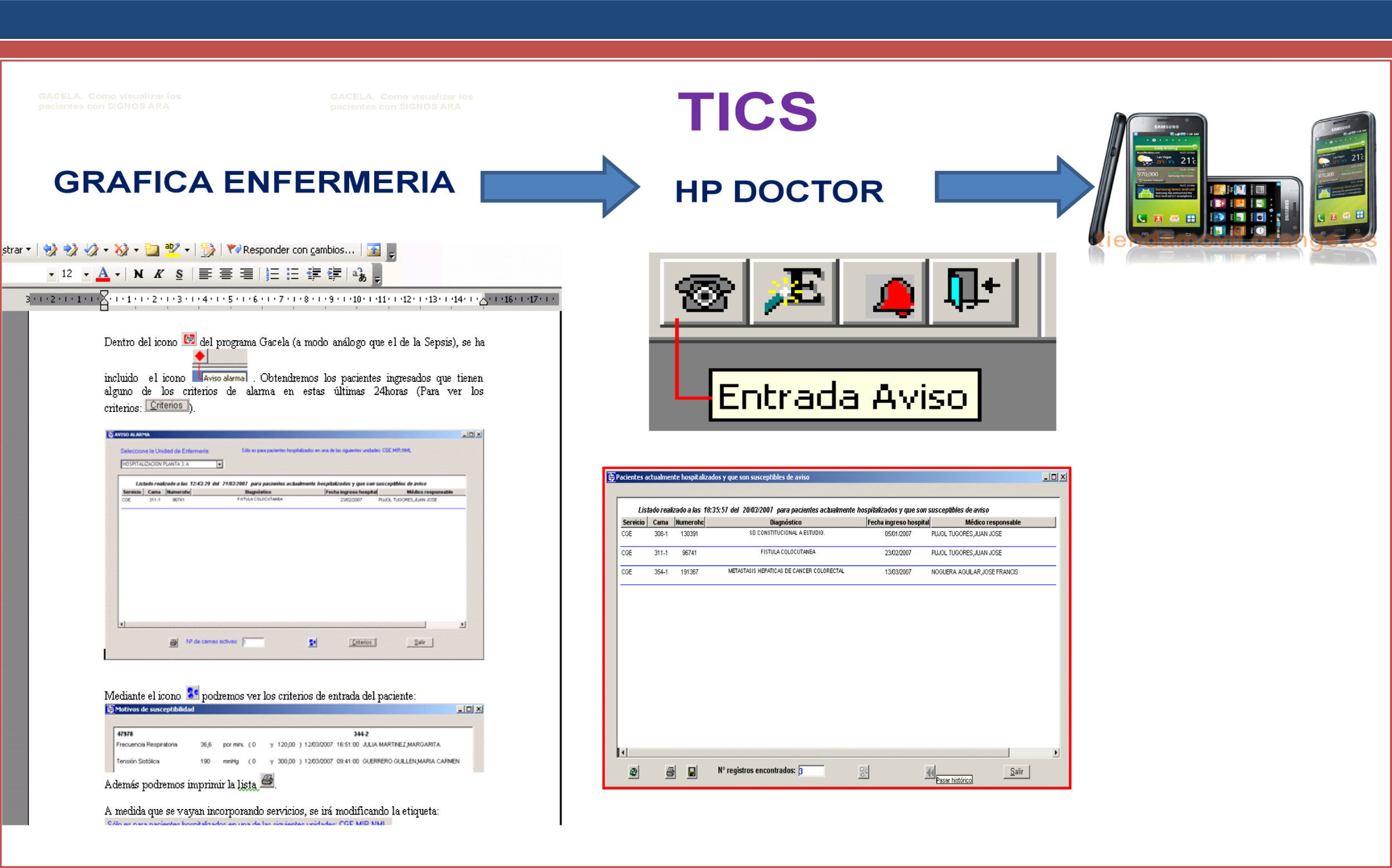
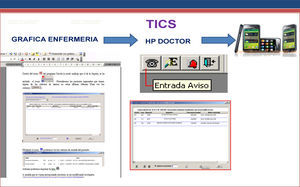
Description of the Medical Information SystemSon Llàtzer Hospital is a second level center with 450 functioning beds and a recruitment population of 250,000 inhabitants. It has been a pioneer in the use of information systems in the hospital setting. The system introduced in our center is the HP-HIS (Hewlett–Packard), which allows us to manage all written documentation, tests requests, and the reception of results and images through an MIS. The use of this system has resulted in digitalization of the case histories and nursing graphic plots, with a link to the hospital laboratory.
During the year 2009 the hospital established an early detection software network, and the medical and nursing personnel of the center were trained in its use (Fig. 1). Specifically, continued training was carried out in the form of 6 basic cardiopulmonary resuscitation ad defibrillation workshops accredited by the Spanish National Cardiopulmonary Resuscitation Plan. In these workshops the professionals were made aware of the fact that the early detection of alert criteria based on the electronic case history can prevent cardiac arrest. Posters were developed and placed in each hospital ward, explaining how to act in situations of CA and detailing the alert criteria defining patients at risk of suffering CA. Starting in January 2010 we introduced the project for detection and intervention measures targeted to patients presenting criteria of rapid care alert (RCA project).
The MIS can be used by all the nurses and physicians of the hospital (supervising physician, physician on duty, and intensivist). It allows follow-up of all the hospitalized patients, with early detection of those individuals presenting certain previously defined alterations. The nursing personnel register the vital signs on the electronic chart. When the entered variables fall outside the ranges defined as normal, or when the laboratory reports abnormal values, an alarm indicator appears in the electronic case history of the patient. The laboratory test criteria of RCA (hemoglobin, potassium, lactate, pH, PaCO2), respiratory frequency, heart rate, Canadian or Glasgow score, arterial pressure, oxygen concentration and pulsioxymetry data are automatically transmitted to a smartphone 24h a day (carried by the intensivist on duty) and to the workstation of the physician reviewing the system. When the patient presents well defined criteria of a potentially serious clinical condition (criteria of RCA), this information is transmitted by the MIS to the mentioned workstation and smartphone 24h a day. The intensivists on duty check the case histories and establish whether the alteration giving rise to the alert has been detected and corrected. The responses to such messages have been protocolized, and action on the part of the intensivist is obligate. If in the course of daily work the intensivist identifies a patient at risk, detailed clinical evaluation of the case is made with the supervising physician or the physician on duty, in order to decide the best course of action. This evaluation is carried out as soon as possible, and always within the first 12h after detection.
Statistical analysisThe data were processed using the Statistical Package for the Social Sciences (SPSS) version 18.0. The Student's t-test was used for the comparison of means, while the chi-squared test or Fisher exact test was applied for the comparison of proportions. Multivariate analysis using stepwise variable selection logistic regression analysis was used only in the CA population, with introduction of the significant variables in the univariate analysis. Statistical significance was accepted for p<0.05.
ResultsA total of 17,991 patients were admitted by the Emergency Department during the period between 1 January 2010 and 31 December 2010. A total of 507 patients died in hospital (2.8%).
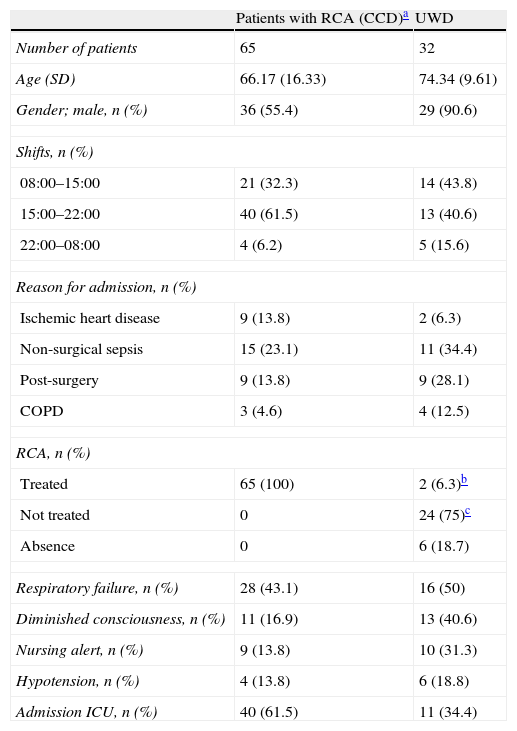
An analysis was made of the alerts transmitted online. During the study period, the MIS registered 9647 rapid care alerts (RCA) in a total of 4020 patients–this being equivalent to 26.4 alerts a day. Of these alert episodes, 1100 (11.4%) proved to be false (e.g., wrong automated arterial pressure recordings, or wrong respiratory frequency or oxygen saturation measurements). A final total of 8547 alerts were thus reviewed. Sixty-five patients (8 patients/1000 interventions) presented episodes with criteria of RCA requiring early intervention by the CCD either because adequate treatment had not been provided or because detection by the intensivist preceded action on the part of the ward physician (Table 2).
Characteristics of the patients with RCA detected by the Critical Care Department, and of the unexpected ward deaths during the year 2010.
| Patients with RCA (CCD)a | UWD | |
| Number of patients | 65 | 32 |
| Age (SD) | 66.17 (16.33) | 74.34 (9.61) |
| Gender; male, n (%) | 36 (55.4) | 29 (90.6) |
| Shifts, n (%) | ||
| 08:00–15:00 | 21 (32.3) | 14 (43.8) |
| 15:00–22:00 | 40 (61.5) | 13 (40.6) |
| 22:00–08:00 | 4 (6.2) | 5 (15.6) |
| Reason for admission, n (%) | ||
| Ischemic heart disease | 9 (13.8) | 2 (6.3) |
| Non-surgical sepsis | 15 (23.1) | 11 (34.4) |
| Post-surgery | 9 (13.8) | 9 (28.1) |
| COPD | 3 (4.6) | 4 (12.5) |
| RCA, n (%) | ||
| Treated | 65 (100) | 2 (6.3)b |
| Not treated | 0 | 24 (75)c |
| Absence | 0 | 6 (18.7) |
| Respiratory failure, n (%) | 28 (43.1) | 16 (50) |
| Diminished consciousness, n (%) | 11 (16.9) | 13 (40.6) |
| Nursing alert, n (%) | 9 (13.8) | 10 (31.3) |
| Hypotension, n (%) | 4 (13.8) | 6 (18.8) |
| Admission ICU, n (%) | 40 (61.5) | 11 (34.4) |
SD, standard deviation; COPD, chronic obstructive pulmonary disease; UWD, unexpected ward deaths; CCD, Critical Care Department; ICU, Intensive Care Unit.
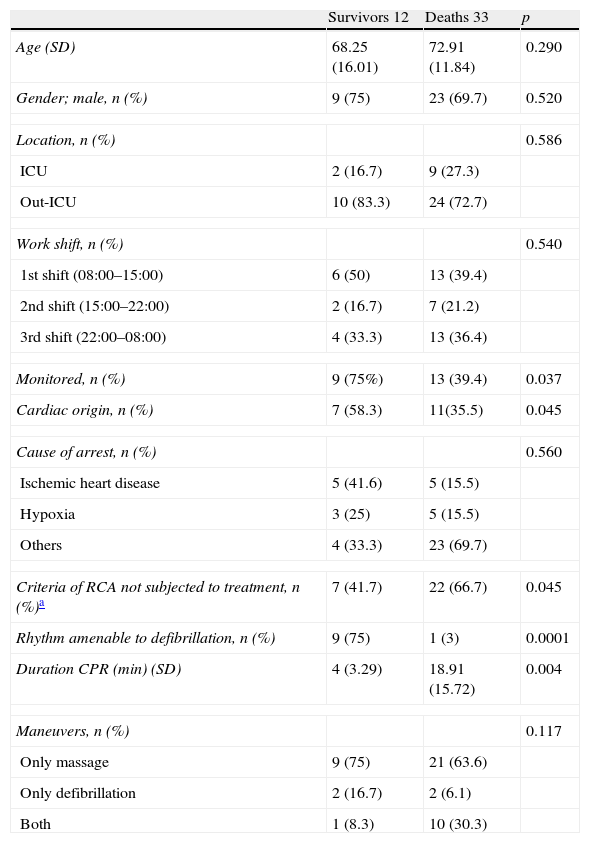
During the study period we registered 45 cardiac arrests (2.5 CA/1000 admissions); of these cases, 29 (64%) presented prior criteria of RCA that were either not treated or were not evaluated adequately by the CCD or ward physician. Of the patients who survived CA (12 cases), 58.3% (7 patients) had not received prior care referred to the observed RCA. Table 3 describes the demographic characteristics, establishing comparisons according to survival. In the multivariate analysis of the predictors of survival at hospital discharge among the patients who had suffered CA, including in the analysis those factors of statistical significance and of clinical relevance, we identified monitorization (odds ratio [OR]: 0.226; 95% confidence interval [95%CI]: 0.050–0.903; p<0.045) and cardiac rhythm amenable to defibrillation (OR: 0.5; 95%CI 0.009–0.134; p<0.002) as independent predictors of a good prognosis.
Demographic characteristics of the patient population with cardiac arrest during 2010.
| Survivors 12 | Deaths 33 | p | |
| Age (SD) | 68.25 (16.01) | 72.91 (11.84) | 0.290 |
| Gender; male, n (%) | 9 (75) | 23 (69.7) | 0.520 |
| Location, n (%) | 0.586 | ||
| ICU | 2 (16.7) | 9 (27.3) | |
| Out-ICU | 10 (83.3) | 24 (72.7) | |
| Work shift, n (%) | 0.540 | ||
| 1st shift (08:00–15:00) | 6 (50) | 13 (39.4) | |
| 2nd shift (15:00–22:00) | 2 (16.7) | 7 (21.2) | |
| 3rd shift (22:00–08:00) | 4 (33.3) | 13 (36.4) | |
| Monitored, n (%) | 9 (75%) | 13 (39.4) | 0.037 |
| Cardiac origin, n (%) | 7 (58.3) | 11(35.5) | 0.045 |
| Cause of arrest, n (%) | 0.560 | ||
| Ischemic heart disease | 5 (41.6) | 5 (15.5) | |
| Hypoxia | 3 (25) | 5 (15.5) | |
| Others | 4 (33.3) | 23 (69.7) | |
| Criteria of RCA not subjected to treatment, n (%)a | 7 (41.7) | 22 (66.7) | 0.045 |
| Rhythm amenable to defibrillation, n (%) | 9 (75) | 1 (3) | 0.0001 |
| Duration CPR (min) (SD) | 4 (3.29) | 18.91 (15.72) | 0.004 |
| Maneuvers, n (%) | 0.117 | ||
| Only massage | 9 (75) | 21 (63.6) | |
| Only defibrillation | 2 (16.7) | 2 (6.1) | |
| Both | 1 (8.3) | 10 (30.3) | |
SD, standard deviation; ICU, Intensive Care Unit.
A total of 507 deaths were evaluated. We registered 35 unexpected deaths (6.9% of the total mortality), of which 32 occurred in the ward (UWD) and three in the CCD. Of the UWD, 24 (75%) were preceded by criteria of RCA not subjected to treatment or evaluated by either the CCD or the ward physician; two were preceded by criteria of RCA subjected to treatment; and 6 presented no criteria of RCA. A total of 34.4% of the deaths (11 patients) were evaluated as avoidable deaths. In 9 patients with criteria of RCA not subjected to treatment (13.8%) and in 10 unexpected deaths (31.3%), the nurse had expressed concern to the ward physician regarding the evolution of the patient.
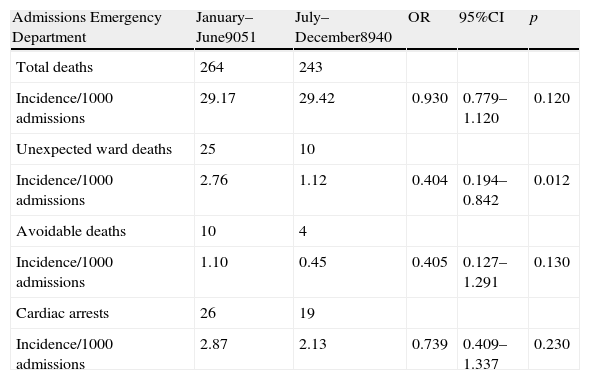
On comparing the two semesters of the year regarding the incidence of mortality and CA since the start of the project, a significant reduction in unexpected deaths was noted (OR: 0.404; 95%CI 0.194–0.842; p=0.012) in the second semester (Table 4).
Incidence of mortality and cardiac arrest in the two semesters of the year 2010.
| Admissions Emergency Department | January–June9051 | July–December8940 | OR | 95%CI | p |
| Total deaths | 264 | 243 | |||
| Incidence/1000 admissions | 29.17 | 29.42 | 0.930 | 0.779–1.120 | 0.120 |
| Unexpected ward deaths | 25 | 10 | |||
| Incidence/1000 admissions | 2.76 | 1.12 | 0.404 | 0.194–0.842 | 0.012 |
| Avoidable deaths | 10 | 4 | |||
| Incidence/1000 admissions | 1.10 | 0.45 | 0.405 | 0.127–1.291 | 0.130 |
| Cardiac arrests | 26 | 19 | |||
| Incidence/1000 admissions | 2.87 | 2.13 | 0.739 | 0.409–1.337 | 0.230 |
In the present study, a large percentage of cardiac arrests and unexpected deaths were preceded by criteria of RCA not subjected to treatment. These results coincide with those obtained by other authors.9–12A priori, it is logical to assume that an intervention during this period of time can improve the patient prognosis. However, different studies evaluating rapid response systems have yielded contradictory results that may be a consequence of the application of different methodological designs.13–15
There are not data supporting the idea that teams led by physicians are more effective than those supervised by nurses. Such systems make use of apparently very costly resources.14,15 In a special article published in 2010 in this journal, Murias et al.16 conducted an exhaustive review of the advantages of Telemedicine, regarding it as a complementing tool capable of improving the medical care offered by intensivists. Recently, Gómez-Tello et al.7 underscored the importance of the introduction of Medical Information Systems in the CCD. Our study is new in that it involves utilization of the MIS for rapidly responding to alarm situations. In Son Llàtzer Hospital, implementation of the MIS for the detection of RCA in hospitalized patients has given rise to a considerable cultural change as regards patient safety, thanks to the training program for hospital nurses and physicians (including intensivists). Launching of the project did not imply increased resource utilization for the hospital, and made it possible to increase the activity of the CCD, due to the large number of patients detected by the system on a daily basis, which otherwise would not have been systematically reviewed. This increase in intensive care activity (with the assessment of 25 alert activations a day) has not required the assignment of added material or human resources giving rise to associated cost increments.
There is scientific evidence that early identification and intervention in clinical situations characterized by physiological instability can prevent cardiac arrest, deaths and readmissions to the SMI.17,18 During the year of our study we recorded no decrease in the incidence of cardiac arrest. Monitorization and rhythms amenable to defibrillation were associated to an improved prognosis. These results are similar to those obtained by other investigators.19 A large percentage of patients with criteria of RCA not subjected to treatment or who were not adequately evaluated, and a large proportion of unexpected deaths, occurred during the first and second nursing shifts. These data suggest that we must intensify and improve our efforts to secure early care for such patients, offering monitorization and admission to the CCD where necessary, and must improve nursing and medical personnel training in the detection of high risk patients in the ward.
In the present study, the intensivists considered it appropriate to decide admission for treatment or monitorization in the case of those patients with criteria of RCA requiring early intervention on the part of the CCD. This observation points to the importance of the adoption of new strategies by the Extended Intensive Care Services (EICS),20,21 with the purpose of improving morbidity–mortality through the early detection of high risk patients outside the ICU. In our study, the most frequently detected criteria of RCA leading to admission to the CCD were respiratory failure and diminished consciousness. Other authors have reported similar findings.12,19,22,23 An important observation is the fact that nursing alerts represent an important percentage of the alerts referred to patients with criteria of RCA not subjected to treatment and unexpected deaths. Recently, the studies of Mitchel et al.24 and of the investigators of the MERIT and ANZICS studies25 concluded that it is of benefit to establish regular training programs for physicians and nurses, with a view to detecting these patients at risk and to secure early action. In our hospital, and in reference to all patients without life support limitations who require high oxygen concentrations (FiO2>50%) or suffer diminished consciousness, we have advised the physicians to examine each case jointly with the supervising physician, and to evaluate the advisability of early admission to the ICU. Future investigations in our field should attempt to unify the alert criteria and response times of the intensivists in an adequate cost-effectiveness scenario.
There is sufficient evidence that early intervention in patients with sepsis avoids progression to severe sepsis and septic shock.26,27 The clinical data suggest that those patients who develop sepsis in hospital wards may suffer a delay in treatment (fluid therapy, vasoactive drugs, antibiotic treatment, delayed admission to the CCD).28 In our study, sepsis was the etiology most commonly detected by the MIS. Although not the objective of our study, early transmission of the criteria of RCA through the MIS, and rapid action on the part of the CCD, could contribute to the early diagnosis and treatment of these patients, as evidenced by other authors.29
Among the main limitations of our study, mention must be made of the lack of data referred to the period prior to introduction of the MIS. The availability of such information, and evaluation of the patients treated by the ward physicians, would have allowed us to assess the impact of the intervention. Mention also must be made of the lack of measurement of the response times on the part of the intensivists. Other limitations in turn may be related to divulgation of the project among all the hospital nursing and medical personnel members, which in some cases undergo constant renewal. A study involving a larger number of patients is needed, with prolongation of the study period, in order to corroborate and consolidate our conclusions.
ConclusionsThe present study shows that the MIS can be a promising complementary tool in the daily work of the CCD that may contribute to improve the prognosis of patients admitted to hospital wards.
Conflicts of interestThe authors declare that they have no conflicts of interest.
The authors thank the interest, effort and dedication of the nursing team supervised by María Cano and Ana Pérez, the ward supervisors implicated in the project, the team of intensivists, medical personnel of the hospitalization wards, the medical personnel on duty, Medical Management and Informatics Department (supervised by Maria Ponseti). The RCA project would not have been possible without their collaboration. Our most sincere gratitude to all of them.
Please cite this article as: Socías Crespí L, et al. Aplicación de las Técnicas de Información y Comunicación para la detección de pacientes de alto riesgo: alarmas de rápida asistencia. Estudio piloto del Proyecto ARA-Son Llàtzer. Med Intensiva. 2013;37:19–26.