Vaccination of the population is a decisive factor in the management of a pandemic. In this respect, SARS-CoV-2 vaccination on a national and worldwide scale offers an opportunity to control the COVID-19 pandemic. Although most of the attention has focused on the capacity of the vaccination program to reduce mortality – this capacity having been confirmed in the case of the priority population groups targeted for vaccination – its impact upon the overburdened healthcare systems is also important.1
However, marked variation is to be expected in the impact of SARS-CoV-2 vaccination according to the different age groups included in the different phases of the vaccination program. Specifically, a decrease in mortality is to be expected among patients over 80 years of age, with a decrease in hospital admissions among those individuals close to 70 years of age, and a decrease in admissions to the Intensive Care Unit (ICU) in those close to 60 years of age.2
In this context, we aimed to analyze the impact of the SARS-CoV-2 vaccination program upon admissions to the ICU of a Spanish third-level hospital. A retrospective study was made of all cases hospitalized due to SARS-CoV-2 infection with admission to the ICU between 14 March 2020 and 9 June 2021. The study period was divided into annual calendar weeks for both years – starting in week 9 of 2020 and ending in week 23 of 2021.
The data were obtained from the COVID-19 patient registry of the Department of Intensive Care Medicine, following approval by the local Research Ethics Committee and the obtainment (written and/or by telephone) of informed consent from the patients/legal representatives, as well as from the information published by the health authorities of our region.3
The results are presented as percentages for categorical variables and as the mean and standard deviation (SD) and/or range for continuous quantitative variables. Comparisons of means between groups were made using the Student t-test for independent samples, with or without Welch's correction.
During the analyzed period, a total of 3961 patients were admitted to our hospital due to illness attributed to SARS-CoV-2 infection. A total of 563 patients over 18 years of age required admission to the ICU at some point during their stay (14.21%). The mean age of the patients admitted to the ICU was 63±13 years, and 69% were males. The mean duration of stay in the COVID-19 ICU was 14 days (range 1–85). The mortality rate in the ICU was 16% (6 patients currently remain admitted to the COVID-19 ICU).
The mean age in the pre-immunization period (509 patients) was 63.22±14 years, versus 58.88±16 in the post-immunization period (difference 4.34 years; 95% confidence interval [95%CI]: 1.84–6.83; p=0.0007). The mean age of the patients admitted to the ICU once 10% of the population had been immunized (53 patients) decreased to 52.35 (15) years (difference 10.87 years; 95%CI: 6.74–14.99; p=0.0001).
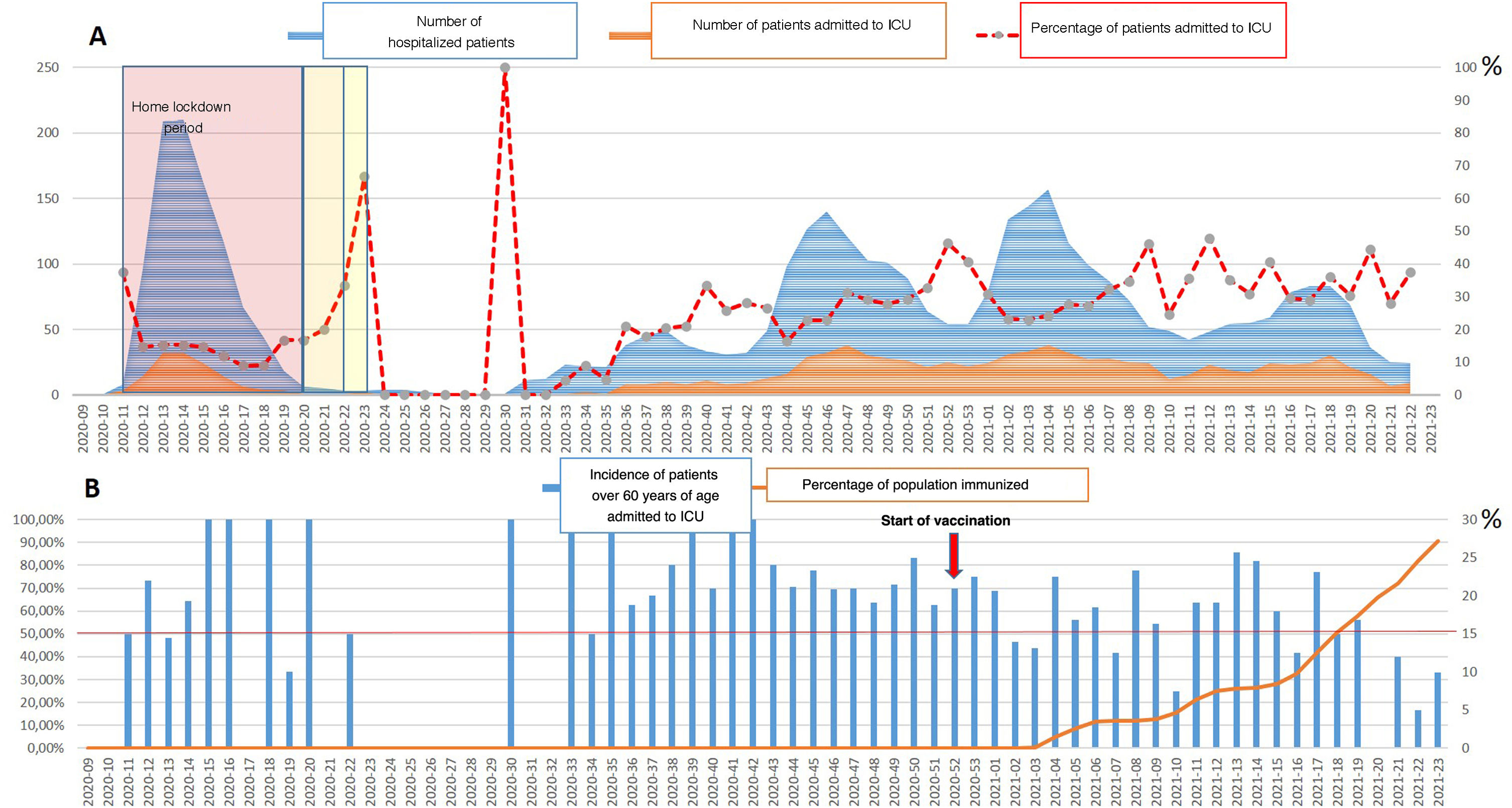
As can be seen in Fig. 1B, the percentage of patients over 60 years of age admitted to the ICU due to SARS-CoV-2 disease dropped to below 50% since the time when 17% of the population had been immunized. This circumstance was not observed in the period immediately following the adoption of the home lockdown measures (Fig. 1A).
Time scale (annual calendar weeks) for describing admissions to hospital and admissions to the ICU due to SARS-CoV-2 disease, and for assessing the impact of adult vaccination upon admission to the ICU. (A) Time scale showing the number of patients admitted to hospital due to COVID-19 (blue area) and the number of patients admitted to the COVID-19 ICU (orange area); the red dotted line shows the percentage of patients admitted to the COVID-19 ICU with respect to the number of hospitalized patients. The transparent red area reflects the home lockdown time. (B) Time scale with overlapping bars representing the percentage of patients over 60 years of age admitted to the ICU in each analyzed week, while the solid orange line reflects the percentage of immunized patients in the population. The red arrow marks the week of start of the vaccination period.
The age of the patients admitted to the ICU due to SARS-CoV-2 disease is not only independently correlated to mortality among such individuals,4 but has been recognized as a factor associated with excess mortality not directly attributed to SARS-CoV-2 in this group of patients.5
On the other hand, the data obtained suggest that the efforts made before vaccination to control the spread of the virus through personal measures (reduction of interpersonal contact, physical distancing, washing of hands and wearing of masks) or national initiatives (travel restrictions, closing of schools and lockdowns) may have suppressed transmission to some point, but did not modify the basis of the pandemic.2
Our data are consistent with the main preliminary reports that evidence a decrease in COVID-19 cases and serious illness in populations with a high vaccination rate. An evaluation by the United Stated CDC in 24 hospitals found COVID-19 vaccination to be 64% effective in preventing hospitalization due to COVID-19 among partially vaccinated adults ≥65 years of age, and 94% effective in the case of fully vaccinated adults ≥65 years of age.6,7
One of the main limitations of our analysis is that concomitant effects were not taken into account – including the spread of more transmissible SARS-CoV-2 variants, the use of recommended therapies that have experienced modifications over time,8 and the implementation and relaxation of prevention policies at community level.
Financial supportThe present study has received no financial support.
Please cite this article as: González-Castro A. Impacto de la vacunación en los ingresos en una unidad de cuidados intensivos por COVID-19 en un hospital de tercer nivel. Medicina Intensiva 2022;46:406–407.