To analyze the factors associated with the activation of the severe trauma care team (STAT) in patients admitted to the ICU, to measure its impact on care times, and to analyze the groups of patients according to activation and level of anatomical involvement.
DesignProspective cohort study of severe trauma admitted to the ICU. From June 2017 to May 2019. Risk factors for the activation of the STAT analysed with logistic regression and CART type classification tree.
SettingSecond level hospital ICU.
PatientsPatients admitted consecutively.
InterventionsNo.
Main variables of interestSTAT activation. Demographic variables. Injury severity (ISS), intentionality, mechanism, assistance times, evolutionary complications, and mortality.
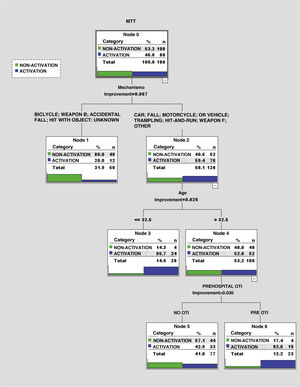
ResultsA total of 188 patients were admitted (46.8% of STAT activation), median age of 52 (37−64) years (activated 47 (27−62) vs not activated 55 (42−67) P = 0.023), males 84.0%. No difference in mortality according to activation. The logistic model finds as factors: care (16.6 (2.1−13.2)) and prehospital intubation (4.2 (1.8−9.8)) and severe lower extremity injury (4.4 (1.6−12.3)). Accidental fall (0.2 (0.1−0.6)) makes activation less likely. The CART model selects the type of trauma mechanism and can separate high and low energy trauma.
ConclusionsFactors associated with STAT activation were prehospital care, requiring prior intubation, high-energy mechanisms, and severe lower extremity injuries. Shorter care times if activated without influencing mortality. We must improve activation in older patients with low-energy trauma and without prehospital care.
Analizar los factores asociados a la activación del equipo de asistencia al trauma grave (EATG) en pacientes que ingresan en UCI, medir su repercusión en los tiempos de asistencia, y analizar los grupos de pacientes según activación y nivel de afectación anatómica.
DiseñoEstudio de cohortes prospectivo del trauma grave que ingresan en UCI. Desde junio 2017 a mayo 2019. Factores de riesgo de la activación analizados con regresión logística y árbol de clasificación tipo CART.
ÁmbitoUCI hospital de segundo nivel.
PacientesPacientes ingresados de forma consecutiva.
IntervencionesNinguna.
Variables de interés principalesActivación del EATG. Variables demográficas. Gravedad lesional (ISS), intencionalidad, mecanismo, tiempos de asistencia, complicaciones evolutivas y mortalidad.
ResultadosIngresaron un total de 188 pacientes (46,8% de activación EATG), edad mediana de 52(37–64) años (activados 47(27–62) vs no activados 55(42–67) p = 0,023), varones el 84,0%. No diferencias en la mortalidad según activación. El modelo logístico encuentra como factores: la atención (16,6(2,1–13,2)) e intubación prehospitalaria (4,2(1,8–9,8)) y, la lesión grave de extremidades inferiores (4,4(1,6–12,3)). Padecer una caída accidental (0,2(0,1–0,6)) hace menos probable la activación. El modelo CART selecciona el tipo de mecanismo del traumatismo y es capaz de separar los traumatismos de alta y baja energía.
ConclusionesLos factores asociados con activación del ETAG fueron la atención prehospitalaria, requerir intubación previa, mecanismos de alta energía y lesiones graves de extremidades inferiores. Menores tiempos de asistencia si activación sin influir en la mortalidad. Debemos mejorar la activación en pacientes mayores con traumatismos de baja energía y sin atención prehospitalaria.
Traumatic injuries are one of the leading causes of mortality and disability among the young population.1 To reduce these adverse events major trauma care systems (MTCS) should be planned and organized comprehensively. Despite the importance of MTCSs there is no national or international consensus on this regard or how to organize this care in the pre- and in-hospital setting.2,3
Having a multidisciplinary major trauma team (MTT) available and coordinated at hospital level with the presence of a leader distributing tasks per role among the different specialists (ER doctors, intensivists, anesthesiologists, surgeons and trauma doctors, nursing staff, etc.) has proven to reduce care times and increase the chances of survival among patients who sustain the most severe traumas.4,5
The involvement of the ICU as part of the MTT participating in early care and improving care times until the patient is eventually transferred and further care is administered is a basic element to improve the quality of healthcare in the management of severe trauma patients.6
The existence of activation protocols based on the identification of the patient’s instability, his physiological alterations (hemodynamic, neurological, and respiratory), and specific injuries based on their severity facilitate the proper activation of the MTT minimizing under and over-triage. We should mention that the key for this activation is the doctor’s criterion of prehospital and ER care.7,8
When a hospital implants an MTT program it should include all the mechanisms required to monitor its activity and analyze the issues that can improve the quality of healthcare.5,9
The objective of our study was to assess the factors associated with the activation of the major trauma team (MTT) in patients admitted to the ICU, measure their repercussion on care times, and analyze different groups of patients based on their activation and level of anatomical damage.
Material and methodsProspective, observational study conducted from June 2017 through May 2019 of patients admitted to the polyvalent ICU from Arnau de Vilanova de Lleida hospital, Lleida, Catalonia. Our hospital has been categorized as a level IIb center capable of providing care to severe trauma patients (ER surgical room, conventional radiology with CAT scan, general and orthopedic surgery) with intensive care and neurosurgery units available on a 27−7 basis.
The hospital ethics committee was briefed prior to conducting the study (CEIC No.-1997). It was decided that the patient’s informed consent would not be necessary since data collected were essential for diagnostic and follow-up purposes. Patients’ anonymity was guaranteed at any time.
Inclusion criteria: all patients >16 years with trauma requiring ICU admission for over 24 h. Exclusion criteria: patients treated or else transferred to a different center or with incomplete data.
Activation protocolThe activation of the MTT falls into the hands of the ER doctor after prior communication to the outpatient emergency services or primary assessment in the resuscitation ward. Protocol identifies those lesions considered specific, as well as the patient’s instability (see definitions in the following sections) as indicators for activation. Initially, the MTT includes an ER doctor, one intensivist, a trauma doctor, and a general surgeon. Major trauma patients admitted to the ICU and treated by a MTT were compared to those only treated at the ER and admitted to the ER following the intensivist’s decision. All patients were treated in full observance of the advanced trauma life support (ATLS) training program.
Variables collected at the ERUpon arrival at the ER, a patient is diagnosed as unstable if he shows, at least, 1 of the following states: hemodynamic instability (hypotension; SAT < 90 mmHg), need for hemoderivative transfusion and/or cardiac arrest; respiratory instability (SpO2 < 90% and/or mechanical ventilation), and neurological instability (GCS ≤ 8).10 Lesions eligible for MTT activation are those associated with cranial fractures, facial or neck wounds that can obstruct the airway, unstable pelvis and thorax, 2 or more fractures of long bones or amputations, and penetrating thoracic and abdominal wounds or round the neck area.11
Variables collected at ICU admissionVariables were collected on an electronic form (retrauci.org) including demographic data (sex and age) and use of antithrombotic drugs (antiplatelet and anticoagulant drugs); type of trauma sustained (closed or penetrating), and mechanism and intentionality. Type of outpatient care (emergency system, conventional ambulance or self-resources), and management of the airway.
The following variables were collected too: respiratory rate and oxygen saturation, arterial blood pressure, and neurological level (GCS) for estimate purposes (RTS).12 Trauma injuries were categorized based on the Abbreviated Injury Scale (AIS 2005) update 2008 for the estimate of anatomical severity (MAIS, ISS, NISS).13 The chances of survival were estimated using the TRISS methodology.14
Organ failure was defined as hemodynamic (SAP < 90 mmHg requiring volemia, hemoderivatives, and active support); trauma related coagulopathy (trauma with an increased prothrombin time or activated partial thromboplastin 1.5 times over control levels or fibrinogen values < 150 mg/dL) or thrombopenia < 100 000 µL within the first 24 h; respiratory (PO2/FiO2 ratio < 200) and renal failure according to the RIFLE categorization with 3 different levels of acute kidney injury: risk, injury, and failure based on changes to the plasma levels of creatinine or rhythm of diuresis.15
The type of care provided based on the need and type of surgery performed within the first 24 h, the administration of hemoderivatives, mechanical ventilation, and neuromonitorization techniques (ICP) are included here.
Follow-up of the ICU stay, and the 30-day mortality rate was conducted at the ICU and during admission to the hospital conventional ward.
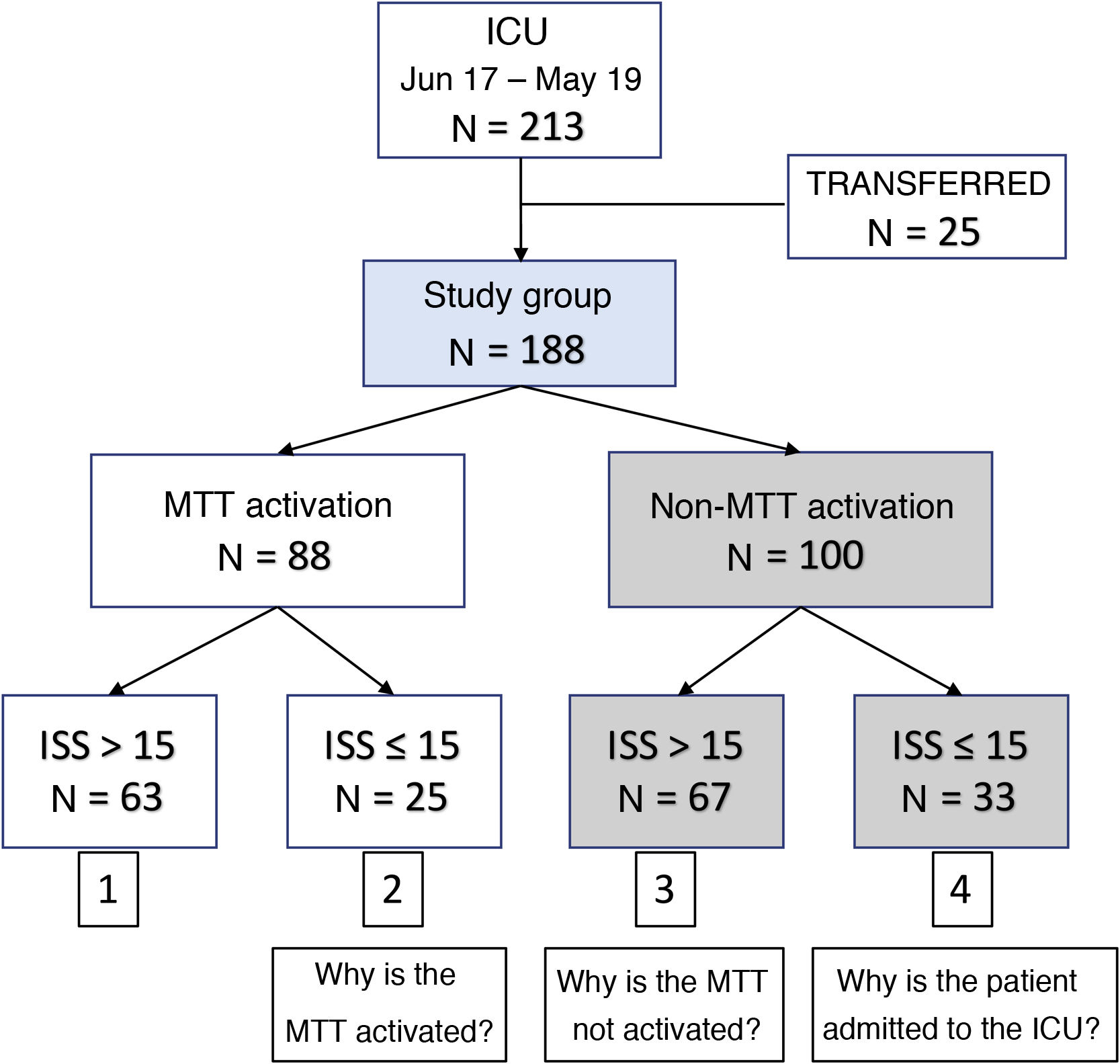
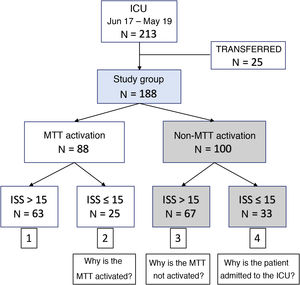
Based on the MTT activation and the ISS (cut–off value, 15) 4 different groups of patients were categorized:1 MTT activation and ISS > 152; MTT activation and ISS ≤ 153; non-MTT activation and ISS > 15; and4 non-MTT activation and ISS ≤ 15.
Time was measured in minutes: CAT scan time (since ER admission until the CAT scan was actually performed); ICU time (since ER admission until arrival at the ICU); and surgical time (since arrival at the ER until the patient is transferred to the operating room).
Statistical analysisVariables were expressed as median (interquartile range) or as percentages based on the type of variable. Groups were compared using the Mann–Whitney U test or the chi-square test (P values < .05 were considered statistically significant). A multivariant binary logistic regression model was used with variable results in the activation of the MTT. All variables were included based on their significance in the univariant analysis. A stepwise selection system was used for the ultimate selection of the variables included in the model. In addition, a multivariant model was used based on the CART (Classification and Regression Tree) classification algorithm that included the same variables and used a minimum number of registries of 25 in the terminal node and cross-validation as a stop criterion.16 Estimates were performed with the statistical software package SPSS (v.23).
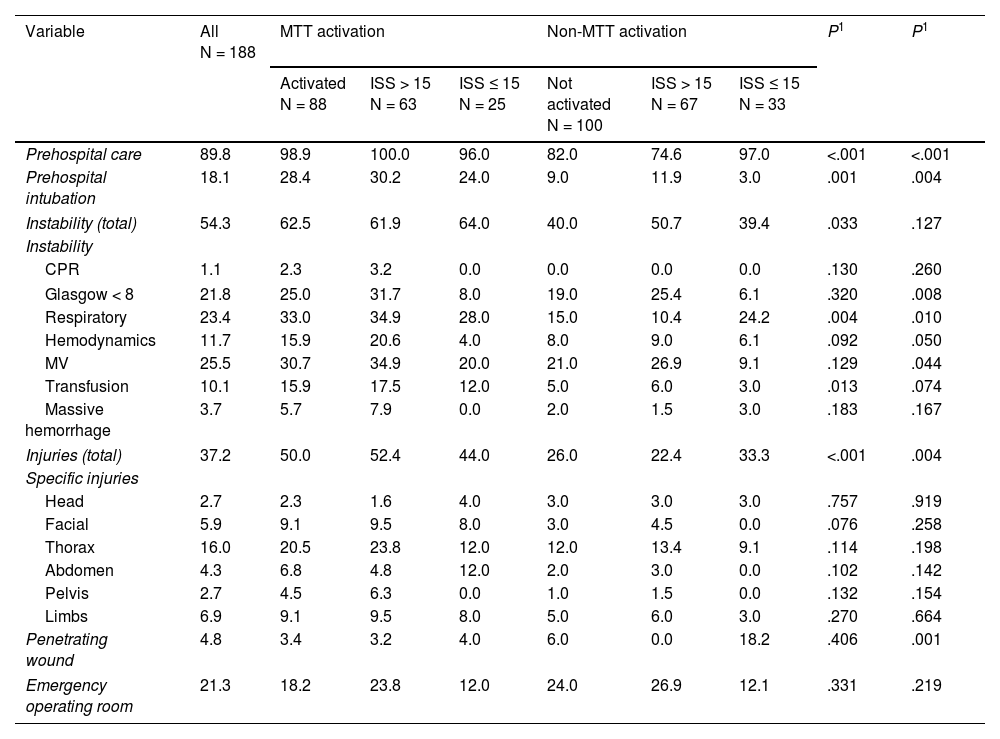
ResultsThe study group included 188 patients (Fig. 1). In 88 patients ICU admission (41.3%) followed the activation of the MTT. The overall mortality rate was 10.1%. Table 1 shows the demographic characteristics and type of trauma sustained. Table 2 shows the conditions of instability and type of injury sustained assessed upon arrival at the ER. Table 3 shows the procedures and surgeries performed on the patients.
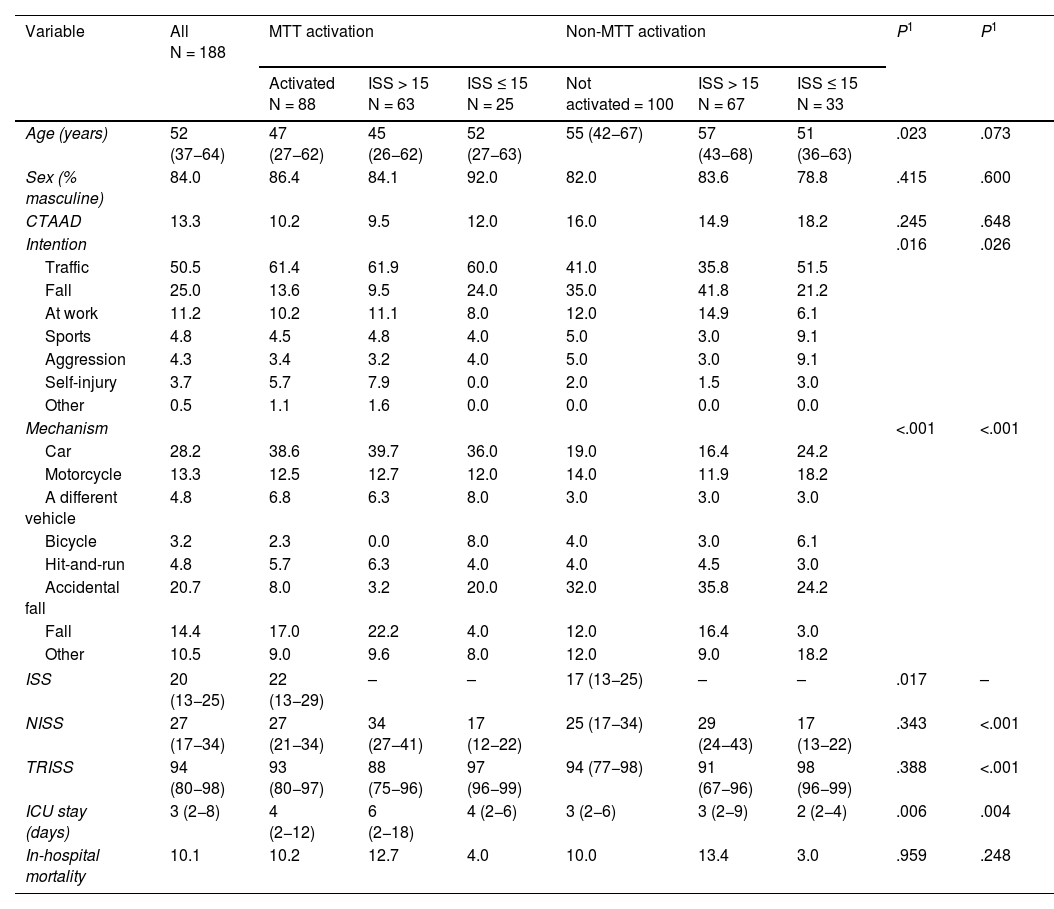
Demographic characteristics of trauma patients with ICU admission (N = 188) based on MTT activation and the ISS.
| Variable | All N = 188 | MTT activation | Non-MTT activation | P1 | P1 | ||||
|---|---|---|---|---|---|---|---|---|---|
| Activated N = 88 | ISS > 15 N = 63 | ISS ≤ 15 N = 25 | Not activated = 100 | ISS > 15 N = 67 | ISS ≤ 15 N = 33 | ||||
| Age (years) | 52 (37−64) | 47 (27−62) | 45 (26−62) | 52 (27−63) | 55 (42−67) | 57 (43−68) | 51 (36−63) | .023 | .073 |
| Sex (% masculine) | 84.0 | 86.4 | 84.1 | 92.0 | 82.0 | 83.6 | 78.8 | .415 | .600 |
| CTAAD | 13.3 | 10.2 | 9.5 | 12.0 | 16.0 | 14.9 | 18.2 | .245 | .648 |
| Intention | .016 | .026 | |||||||
| Traffic | 50.5 | 61.4 | 61.9 | 60.0 | 41.0 | 35.8 | 51.5 | ||
| Fall | 25.0 | 13.6 | 9.5 | 24.0 | 35.0 | 41.8 | 21.2 | ||
| At work | 11.2 | 10.2 | 11.1 | 8.0 | 12.0 | 14.9 | 6.1 | ||
| Sports | 4.8 | 4.5 | 4.8 | 4.0 | 5.0 | 3.0 | 9.1 | ||
| Aggression | 4.3 | 3.4 | 3.2 | 4.0 | 5.0 | 3.0 | 9.1 | ||
| Self-injury | 3.7 | 5.7 | 7.9 | 0.0 | 2.0 | 1.5 | 3.0 | ||
| Other | 0.5 | 1.1 | 1.6 | 0.0 | 0.0 | 0.0 | 0.0 | ||
| Mechanism | <.001 | <.001 | |||||||
| Car | 28.2 | 38.6 | 39.7 | 36.0 | 19.0 | 16.4 | 24.2 | ||
| Motorcycle | 13.3 | 12.5 | 12.7 | 12.0 | 14.0 | 11.9 | 18.2 | ||
| A different vehicle | 4.8 | 6.8 | 6.3 | 8.0 | 3.0 | 3.0 | 3.0 | ||
| Bicycle | 3.2 | 2.3 | 0.0 | 8.0 | 4.0 | 3.0 | 6.1 | ||
| Hit-and-run | 4.8 | 5.7 | 6.3 | 4.0 | 4.0 | 4.5 | 3.0 | ||
| Accidental fall | 20.7 | 8.0 | 3.2 | 20.0 | 32.0 | 35.8 | 24.2 | ||
| Fall | 14.4 | 17.0 | 22.2 | 4.0 | 12.0 | 16.4 | 3.0 | ||
| Other | 10.5 | 9.0 | 9.6 | 8.0 | 12.0 | 9.0 | 18.2 | ||
| ISS | 20 (13−25) | 22 (13−29) | – | – | 17 (13−25) | – | – | .017 | – |
| NISS | 27 (17−34) | 27 (21−34) | 34 (27−41) | 17 (12−22) | 25 (17−34) | 29 (24−43) | 17 (13−22) | .343 | <.001 |
| TRISS | 94 (80−98) | 93 (80−97) | 88 (75−96) | 97 (96−99) | 94 (77−98) | 91 (67−96) | 98 (96−99) | .388 | <.001 |
| ICU stay (days) | 3 (2−8) | 4 (2−12) | 6 (2−18) | 4 (2−6) | 3 (2−6) | 3 (2−9) | 2 (2−4) | .006 | .004 |
| In-hospital mortality | 10.1 | 10.2 | 12.7 | 4.0 | 10.0 | 13.4 | 3.0 | .959 | .248 |
Values expressed as percentages or median (interquartile range). CTAAD, chronic treatment with antiplatelet and anticoagulant drugs; ISS, Injury Severity Score; NISS, New Injury Severity Score; TRISS, Trauma and Injury Severity Score. P value1: With the chi-square test or the Mann–Whitney U test (comparison between the MTT activation and non-MTT activation group). P value2: With the chi-square test or the Kruskal–Wallis test (4 group comparison).
Activation criteria based on stability and specific lesions seen at the ER of trauma patients with ICU admission (N = 188) based on MTT activation and the ISS.
| Variable | All N = 188 | MTT activation | Non-MTT activation | P1 | P1 | ||||
|---|---|---|---|---|---|---|---|---|---|
| Activated N = 88 | ISS > 15 N = 63 | ISS ≤ 15 N = 25 | Not activated N = 100 | ISS > 15 N = 67 | ISS ≤ 15 N = 33 | ||||
| Prehospital care | 89.8 | 98.9 | 100.0 | 96.0 | 82.0 | 74.6 | 97.0 | <.001 | <.001 |
| Prehospital intubation | 18.1 | 28.4 | 30.2 | 24.0 | 9.0 | 11.9 | 3.0 | .001 | .004 |
| Instability (total) | 54.3 | 62.5 | 61.9 | 64.0 | 40.0 | 50.7 | 39.4 | .033 | .127 |
| Instability | |||||||||
| CPR | 1.1 | 2.3 | 3.2 | 0.0 | 0.0 | 0.0 | 0.0 | .130 | .260 |
| Glasgow < 8 | 21.8 | 25.0 | 31.7 | 8.0 | 19.0 | 25.4 | 6.1 | .320 | .008 |
| Respiratory | 23.4 | 33.0 | 34.9 | 28.0 | 15.0 | 10.4 | 24.2 | .004 | .010 |
| Hemodynamics | 11.7 | 15.9 | 20.6 | 4.0 | 8.0 | 9.0 | 6.1 | .092 | .050 |
| MV | 25.5 | 30.7 | 34.9 | 20.0 | 21.0 | 26.9 | 9.1 | .129 | .044 |
| Transfusion | 10.1 | 15.9 | 17.5 | 12.0 | 5.0 | 6.0 | 3.0 | .013 | .074 |
| Massive hemorrhage | 3.7 | 5.7 | 7.9 | 0.0 | 2.0 | 1.5 | 3.0 | .183 | .167 |
| Injuries (total) | 37.2 | 50.0 | 52.4 | 44.0 | 26.0 | 22.4 | 33.3 | <.001 | .004 |
| Specific injuries | |||||||||
| Head | 2.7 | 2.3 | 1.6 | 4.0 | 3.0 | 3.0 | 3.0 | .757 | .919 |
| Facial | 5.9 | 9.1 | 9.5 | 8.0 | 3.0 | 4.5 | 0.0 | .076 | .258 |
| Thorax | 16.0 | 20.5 | 23.8 | 12.0 | 12.0 | 13.4 | 9.1 | .114 | .198 |
| Abdomen | 4.3 | 6.8 | 4.8 | 12.0 | 2.0 | 3.0 | 0.0 | .102 | .142 |
| Pelvis | 2.7 | 4.5 | 6.3 | 0.0 | 1.0 | 1.5 | 0.0 | .132 | .154 |
| Limbs | 6.9 | 9.1 | 9.5 | 8.0 | 5.0 | 6.0 | 3.0 | .270 | .664 |
| Penetrating wound | 4.8 | 3.4 | 3.2 | 4.0 | 6.0 | 0.0 | 18.2 | .406 | .001 |
| Emergency operating room | 21.3 | 18.2 | 23.8 | 12.0 | 24.0 | 26.9 | 12.1 | .331 | .219 |
CPR, cardiopulmonary resuscitation; MV, mechanical ventilation. Values expressed as percentage or median (interquartile range). P value1: With the chi-square test or the Mann–Whitney U test (comparison between the MTT activation and non-MTT activation group). P value2: With the chi-square test or the Kruskal–Wallis test (4 group comparison).
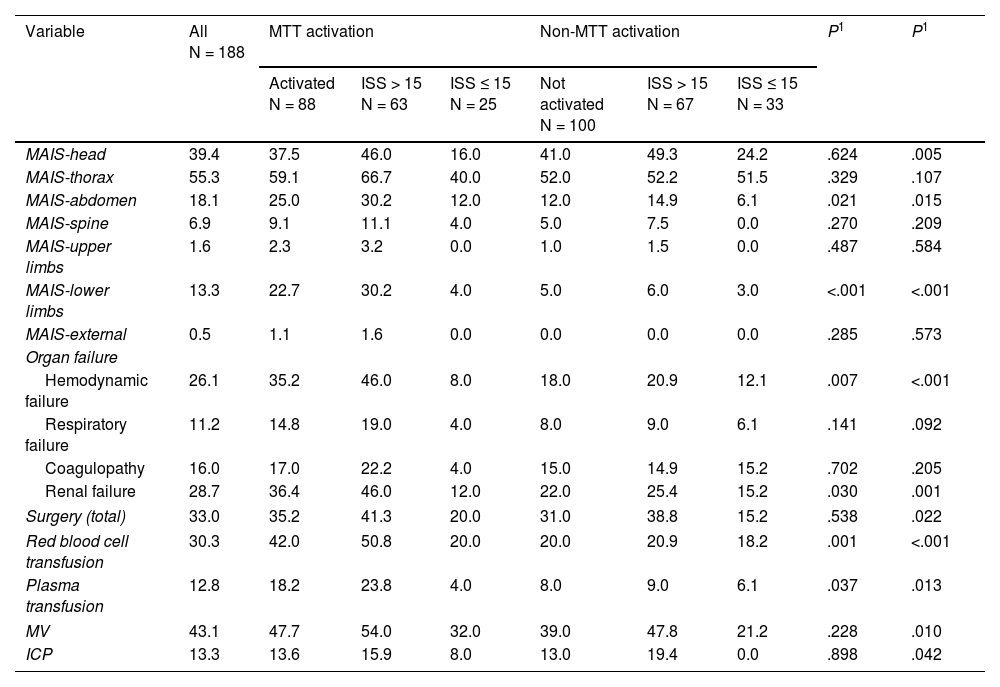
Anatomical alteration, organ failure, and procedures performed in trauma patients with ICU admission (N = 188) based on MTT activation and the ISS.
| Variable | All N = 188 | MTT activation | Non-MTT activation | P1 | P1 | ||||
|---|---|---|---|---|---|---|---|---|---|
| Activated N = 88 | ISS > 15 N = 63 | ISS ≤ 15 N = 25 | Not activated N = 100 | ISS > 15 N = 67 | ISS ≤ 15 N = 33 | ||||
| MAIS-head | 39.4 | 37.5 | 46.0 | 16.0 | 41.0 | 49.3 | 24.2 | .624 | .005 |
| MAIS-thorax | 55.3 | 59.1 | 66.7 | 40.0 | 52.0 | 52.2 | 51.5 | .329 | .107 |
| MAIS-abdomen | 18.1 | 25.0 | 30.2 | 12.0 | 12.0 | 14.9 | 6.1 | .021 | .015 |
| MAIS-spine | 6.9 | 9.1 | 11.1 | 4.0 | 5.0 | 7.5 | 0.0 | .270 | .209 |
| MAIS-upper limbs | 1.6 | 2.3 | 3.2 | 0.0 | 1.0 | 1.5 | 0.0 | .487 | .584 |
| MAIS-lower limbs | 13.3 | 22.7 | 30.2 | 4.0 | 5.0 | 6.0 | 3.0 | <.001 | <.001 |
| MAIS-external | 0.5 | 1.1 | 1.6 | 0.0 | 0.0 | 0.0 | 0.0 | .285 | .573 |
| Organ failure | |||||||||
| Hemodynamic failure | 26.1 | 35.2 | 46.0 | 8.0 | 18.0 | 20.9 | 12.1 | .007 | <.001 |
| Respiratory failure | 11.2 | 14.8 | 19.0 | 4.0 | 8.0 | 9.0 | 6.1 | .141 | .092 |
| Coagulopathy | 16.0 | 17.0 | 22.2 | 4.0 | 15.0 | 14.9 | 15.2 | .702 | .205 |
| Renal failure | 28.7 | 36.4 | 46.0 | 12.0 | 22.0 | 25.4 | 15.2 | .030 | .001 |
| Surgery (total) | 33.0 | 35.2 | 41.3 | 20.0 | 31.0 | 38.8 | 15.2 | .538 | .022 |
| Red blood cell transfusion | 30.3 | 42.0 | 50.8 | 20.0 | 20.0 | 20.9 | 18.2 | .001 | <.001 |
| Plasma transfusion | 12.8 | 18.2 | 23.8 | 4.0 | 8.0 | 9.0 | 6.1 | .037 | .013 |
| MV | 43.1 | 47.7 | 54.0 | 32.0 | 39.0 | 47.8 | 21.2 | .228 | .010 |
| ICP | 13.3 | 13.6 | 15.9 | 8.0 | 13.0 | 19.4 | 0.0 | .898 | .042 |
Values expressed as percentages. AIS, Abbreviated Injury Scale; ICP, intracranial pressure MAIS: Values of AIS ≥ 3; MV, mechanical ventilation. OTS, Orthopedic trauma surgery. P value1: With the chi-square test (comparison between the MTT activation and non-MTT activation group). P value2: With the chi-square test (4 group comparison).
Tables 1–3 show the differences (gray column) of the variables studied between the groups with and without MTT activation. Patients who activated the MTT were younger, had a higher rate of prehospital care, sustained high-energy traumas (car crashes), had less low-energy accidental falls, more damage to the abdomen and lower limbs, more repercussions associated with organ failures, and a greater need for transfusion of red blood cells and plasma. Also, more neurosurgeries and trauma interventions were performed on them too. In addition, these patients had a greater severity based on the ISS and longer ICU stays. No differences were found regarding mortality (10.2% vs 10.0%; P = .959).
Patient groups based on MTT activation and the ISSFig. 1 shows the 4 groups of patients studied based on MTT activation and the ISS. Tables 1–3 show the differences found (columns in white background color).
Patients from group#1 (MTT activation and ISS > 15) were younger, had received more prehospital care, and had sustained high-energy traumas with more physiological and organ repercussions.
Group#2 (MTT activation and ISS ≤ 15) had similar values regarding age and prehospital care with less physiological and organ repercussions.
Patients from group#3 (non-MTT activation and ISS > 15) were older patients with less prehospital care, more low-energy accidental falls, and more neurological damage. They needed more neurosurgeries (even decompressive craniotomies) but had less organ repercussions compared to the first group.
Finally, group#4 (non-MTT activation and ISS ≤ 15) included patients with more physiological and organ stability, more penetrating injuries (even more bladed weapon mechanisms), some neurological damage, more thoracic damage, and less need for procedures being performed on them.
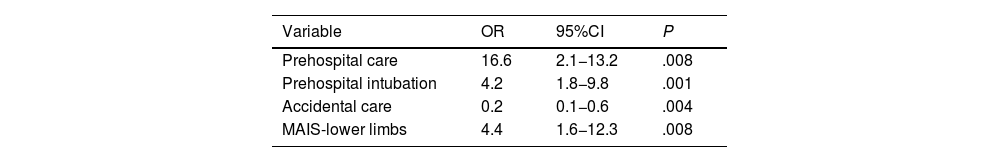
Factors associated with MTT activationTable 4 shows the factors associated with MTT activation in the logistic regression model. We should mention that sustaining accidental falls is a factor that makes activation less likely. Prehospital care and intubation are factors that trigger the MTT activation while severe injuries to the lower limbs also trigger activation.
Logistic regression model of factors affecting the activation of the major trauma team (MTT).
| Variable | OR | 95%CI | P |
|---|---|---|---|
| Prehospital care | 16.6 | 2.1−13.2 | .008 |
| Prehospital intubation | 4.2 | 1.8−9.8 | .001 |
| Accidental care | 0.2 | 0.1−0.6 | .004 |
| MAIS-lower limbs | 4.4 | 1.6−12.3 | .008 |
CI, confidence interval; MAIS, AIS values ≥ 3; OR, odds ratio.
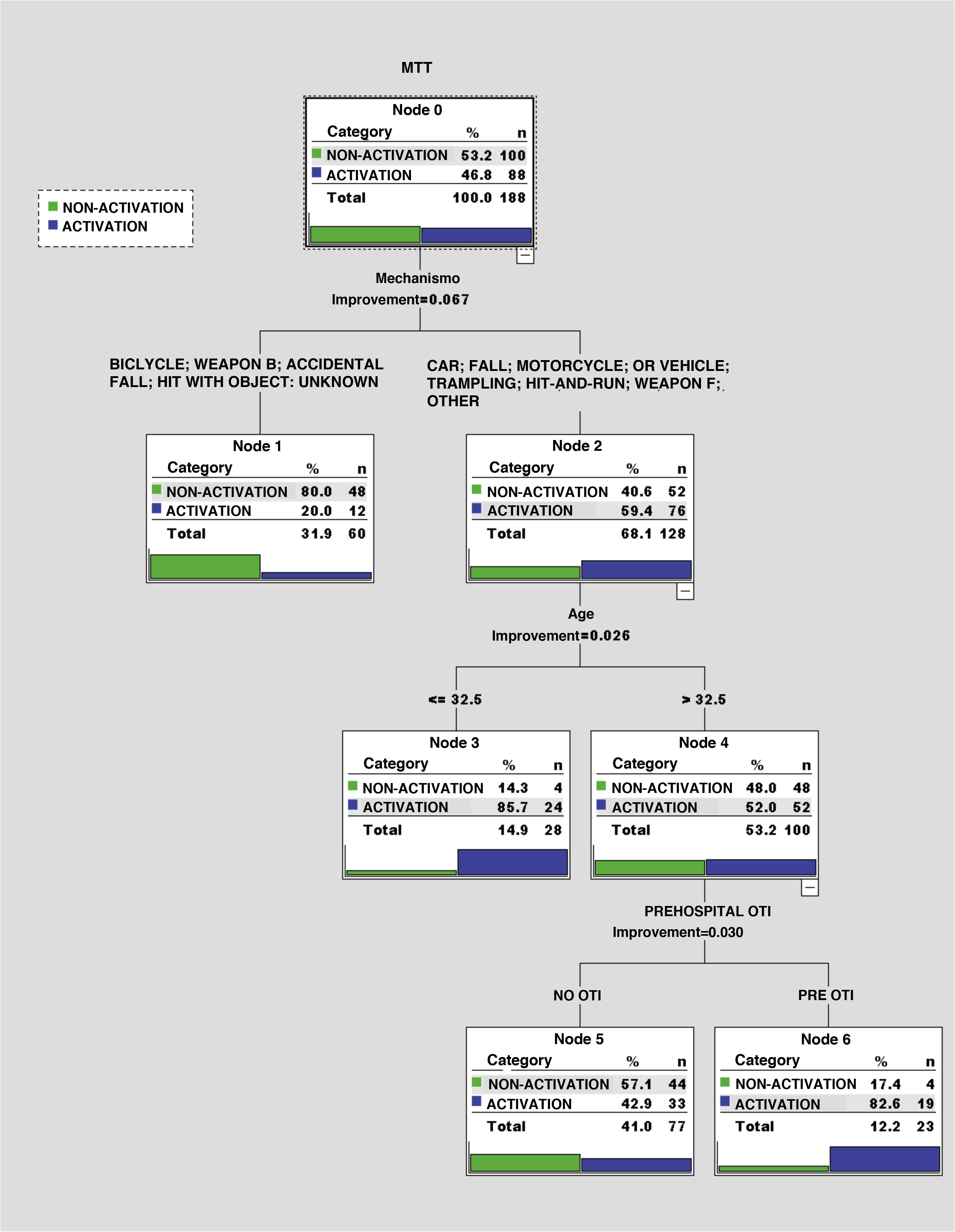
The CART model (Fig. 2) selects the type of mechanism causing the trauma as the first variable including a distinction between low- and high-energy traumas. The high-energy group selects age (cut-off value, 32.5 years) while, in the elderly, a distinction is made based on prehospital OTI. It achieves 4 groups of patients with chances of MTT activation between 20.0% and 82.6%.
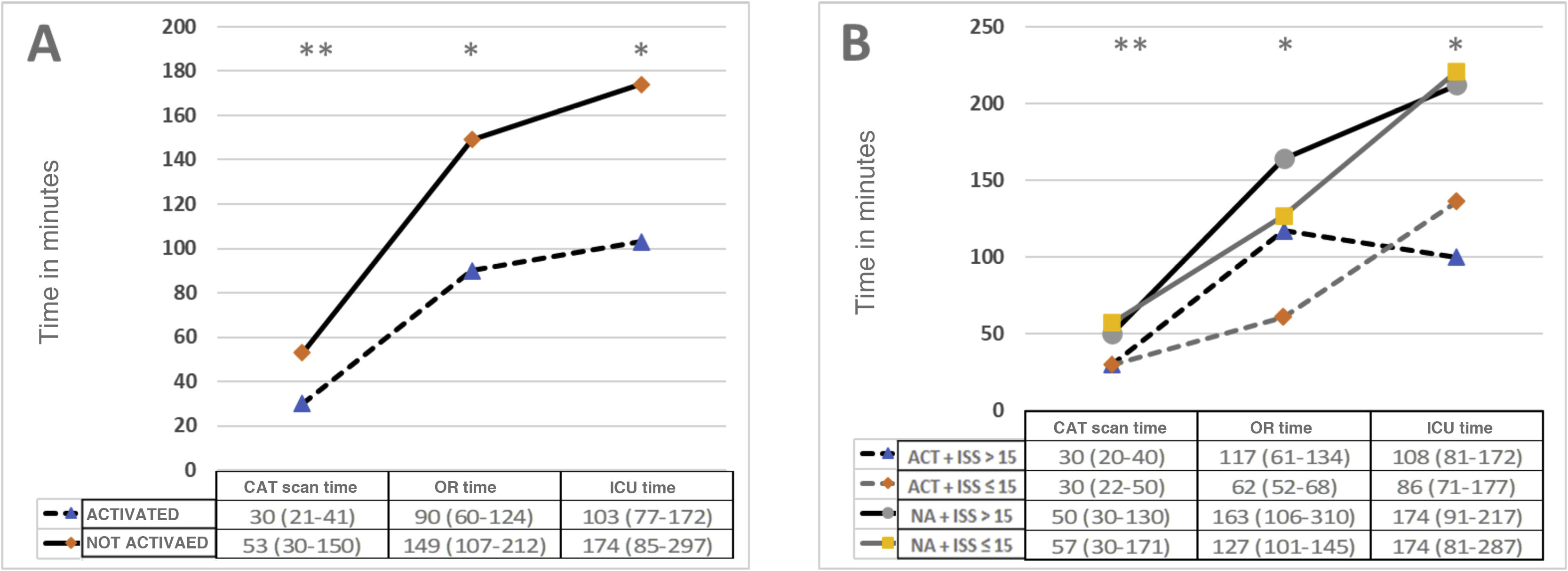
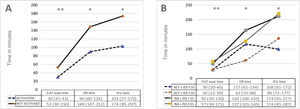
Study of MTT activation timesFig. 3 shows the intervention time results based on the activation-non-activation groups (A) and the 4 groups described. Activation reduces all intervention times. By categorizing into 4 groups, we can see that the one with the shortest times of all is group #2 (MTT activation and ISS ≤ 15) while the one with the longest times is group #3 (non-MTT activation and ISS > 15).
Care times (CAT scan, OR, and ICU). Values as median seen on the tables as interquartile range. A: Distinguished based on MMT activation or not. B: Distinguished based on the activation of the MTT and level of severity with an ISS cut-off value. ACT, activated; NA, not activated. Significant differences (*); P < .05 and (**) P < .01 based on the Mann–Whitney U test or the Kruskal–Wallis test.
This study shows the experience of MTT implantation to improve the quality of healthcare of severe trauma patients who are eventually admitted to the ICU. The factors involved in MTT activation were studied too. Also, it was demonstrated that care times shorten when the MTT becomes activated.
All healthcare processes should be monitored, assessed, and rooms for improvement sought.17 A key factor in the proper organization of a MTT is proper early triage based on updated activation protocols that assess the severity of physiological parameters (GCS motor < 6, HR > SAT, SpO2 < 90%), striking anatomical injuries (active bleeding, cranial deformity, suspected spinal, thoracic or pelvic injury, fracture of 2 or more long bones), and high-energy lesion mechanism.8,10,11 Monitoring under and over-triage is a quality indicator in the healthcare process of trauma patients.7
Traditionally, the Cribari Matrix has been used to assess the proper triage of severe trauma (ISS > 15) that should be handled by the MTT. It is considered that we should never go over 5% of under-triage and over 35% of over-triage.18
In our study, only 41.3% of the patients admitted to the ICU were treated by the MTT. However, we should mention that 32.4% of the patients admitted to the ICU had ISSs < 15. Based on the quality criteria published by SEMICYUC in 2017, 95% of the patients with severe trauma (Revised Trauma Score (RTS) in the early selection ≤ 11 points and/or Injury Severity Score (ISS) score > 15 admitted to the ICU should be treated at the intensive care unit.17 Other experiences in different centers should be explored to establish the final ideal percentage of patients who should be treated by the MTT before being admitted to the ICU.
Fig. 1 includes 3 questions asked depending on activation and the level of anatomical damage based on the ISS. The answer to the first question is that these patients, though more stable, often sustain high-energy trauma and are treated by prehospital care teams. The second question has to do with the fact that the MTT is not activated for being older patients with low-energy traumas, and with less prehospital care. And the answer to the third question is that it is a group of patients admitted for monitorization purposes basically.
The factors associated with the activation of the MTT were patients initially treated by a prehospital emergency team who required previous intubation and had sustained severe injuries to the lower limbs, mainly pelvic fractures. The CART model establishes that high-energy traumas have more chances of MTT activation compared to younger or intubated patients in the prehospital setting. Proper triage of prehospital emergency teams and good communication with the hospital setting can improve the previous activation of the MTT.8,19
We should mention that the only factor associated with the non-activation of the MTT was patients who had sustained accidental falls without activation of any prehospital units. Elderly patients on anticoagulant drugs who accidentally fall have high morbidity and mortality rates are a subgroup of patients who should be included in the activation protocols. In our series, mean age was higher in the subgroup of patients in whom the MTT was not activated.20,21
Currently, MTTs have proven capable of improving care times in trauma patients.22 In our own experience, MTT activation significantly reduced CAT scan times, emergency surgeries, and the patient ultimate transfer time to the intensive care unit. Although our experience found no mortality differences, recent studies establish a correlation between delayed ICU admissions and higher mortality rates, and with the importance of providing critical care outside the ICU setting.23
Our results give us a series of recommendations like how important it is to have updated activation protocols agreed between different prehospital care teams and ER teams. Activation criteria should be monitored and assessed to analyze the over-triage of patients treated.
The main study limitation is that it was conducted at a single center with its specific clinical and demographic characteristics. Also, the limited size of the sample could impact the generalization of results. Another limitation is that patients treated by the MTT not admitted to the ICU were not followed.
In conclusion, establishing major trauma teams at hospital level with good communication between all the units involved in severe trauma care reduces care times. Treatment by emergency teams with orotracheal intubation capabilities in the prehospital setting after a high-energy car crash with injuries to the lower limbs plays a key role in the activation of the MTT. We should improve MTT activation in elderly patients who sustain low-energy traumas and are not treated by emergency teams.
Authors’ contributionsNM, JT, and LS were involved in the study design. JT, LS, NM, MB. GJ, JV, JR, AP, and DM analyzed and interpreted data, and were involved in data mining and the manuscript review process. All the authors read and approved the manuscript final version.
Conflicts of interestNone whatsoever.