To describe the incidence and main clinical characteristics of barotrauma during open lung ventilation (OLV).
DesignA retrospective, observational, descriptive study was made of 100 patients with acute respiratory failure and bilateral pulmonary infiltrates.
Interventions(1) A lung recruitment maneuver (LRM) with fixed ventilation pressure and progressive positive end-expiratory pressure (PEEP) elevations was carried out, followed by stepwise decreases until establishing open-lung PEEP at the value associated to maximum respiratory compliance; (2) assisted/controlled pressure ventilation to achieve a tidal volume of 6–8ml/kg; and (3) chest X-rays after LRM and daily for as long as respiratory failure persisted.
ResultsNine patients, 7 with pneumonia and 2 with chest trauma, developed barotrauma (2 subcutaneous emphysemas and 7 cases of pneumothorax), representing an overall incidence of 9% and 16% in patients with primary lung injury. In 7 patients barotrauma was only a radiological finding; in the other 2 patients, it manifested as bilateral and tension pneumothorax, inducing pulmonary hypoventilation without hemodynamic impairment. Only in these two cases was the ventilatory strategy modified. There were no differences in the airway pressures or volumes between patients with and without barotrauma. Mortality was similar in both groups.
ConclusionsBarotrauma was an exclusive complication of patients with primary lung injury, and the incidence in this group was high. In most cases, there were only radiological findings without clinical significance that did not require the suspension of OLV. Barotrauma was neither related to high pressures and volumes nor associated with increased mortality.
Describir la incidencia y principales características clínicas del barotrauma durante la ventilación mecánica con apertura pulmonar.
DiseñoEstudio retrospectivo, observacional, descriptivo, en 100 pacientes con insuficiencia respiratoria aguda e infiltrados pulmonares bilaterales.
Intervenciones1) maniobra de reclutamiento pulmonar (MRP) con presión de ventilación fija e incrementos progresivos de presión positiva al final de la espiración (PEEP), seguida de decrementos escalonados hasta establecer la PEEP de apertura en el valor asociado a la máxima distensibilidad respiratoria; 2) ventilación asistida/controlada por presión ajustada para un volumen tidal de 6-8ml/kg; y 3) radiografía de tórax después de la MRP y diariamente mientras persistió la insuficiencia respiratoria.
ResultadosNueve pacientes, 7 con neumonía y 2 con trauma torácico, desarrollaron barotrauma (2 enfisema subcutáneo y 7 neumotórax), lo cual supuso una incidencia total del 9% y del 16% en aquellos pacientes con lesión pulmonar primaria. En 7 pacientes fue tan solo de un hallazgo radiológico; en los otros dos, se manifestó como un neumotórax bilateral y a tensión, cursando con hipoventilación pulmonar. Únicamente en estos dos casos se modificó la estrategia ventilatoria. No hubo diferencias en las presiones ni en los volúmenes respiratorios entre pacientes con o sin barotrauma. La mortalidad fue similar en ambos grupos.
ConclusionesEl barotrauma resultó una complicación exclusiva de pacientes con lesión pulmonar primaria, en los que tuvo una incidencia elevada. En la mayoría de las ocasiones fue un hallazgo radiológico sin manifestaciones clínicas, manteniéndose la ventilación con apertura pulmonar. Su aparición no se relacionó con presiones ni volúmenes respiratorios mayores, ni se asoció a mayor mortalidad.
Pulmonary barotrauma is one of the most feared complications of mechanical ventilation, with an incidence that has decreased in recent years thanks to the adoption of protective ventilatory strategies based on a lowering of tidal volume and control of the airway pressures.1–5 Open lung ventilation (OLV) is a form of protective mechanical ventilation which nevertheless requires the use of high intrathoracic pressures,6 due both to lung recruitment maneuvering (LRM) through the transient application of high transpulmonary pressures, and to the use of a positive end-expiratory pressure (PEEP) sufficiently high to avoid the reappearance of lung collapse.7,8 In this context, some authors have drawn attention to the negative effect which the use of such elevated intrathoracic pressures may have, not only in relation to cardiocirculatory function, but also as refers to the development of pulmonary barotrauma.9,10
In September 2003 we adopted an open lung ventilation protocol based on the application of LRM via stepwise PEEP increments and decrements, and on the selection of open lung PEEP according to the maximum respiratory compliance (Cr). During a period of 89 months we applied this protocol to a large group of patients, conducting a retrospective analysis to determine the incidence and form of presentation of barotrauma, and to establish the main clinical and outcome characteristics of the patients who suffered this complication. Some of the results of this analysis have been previously presented in summarized form.11,12
Patients and methodsBetween September 2003 and January 2011, those patients with severe hypoxemic acute respiratory failure (defined as the incapacity to maintain peripheral oxygen saturation determined by pulsioximetry [SpO2]>90%, with PEEP≥10cmH2O and inhaled oxygen fraction [FiO2] 0.6 [SpO2/FiO2 ratio≤150],13 in the presence of bilateral lung infiltrates in the chest X-rays) were ventilated according to our open lung ventilation protocol. We excluded patients >80 and <16 years of age, previous barotrauma, advanced chronic pulmonary disease (including chronic obstructive pulmonary disease), uncontrollable progressive acidosis (pH<7.15), hemodynamic instability (defined as a mean systemic arterial pressure of <65mmHg despite vasoactive medication), acute heart failure, signs of intracranial hypertension, and end-stage disease. This retrospective study was approved by the Research Bioethics Subcommittee of SAS Hospital in Jeréz (Spain). Informed consent was not considered necessary, since the protocol was regarded as part of the usual management of these patients.
At the time of screening, the patients were being ventilated according to our conventional mechanical ventilation protocol for patients with acute lung injury (ALI): pressure controlled ventilation mode with ventilation pressure over PEEP adjusted for a tidal volume of 6–8ml/kg; sufficient inspiratory time to allow alveolar pressure and airway pressure to equilibrate at the end of inspiration14; PEEP titrated for maximum Cr15; and FiO2 for maintaining SpO2≥90%.
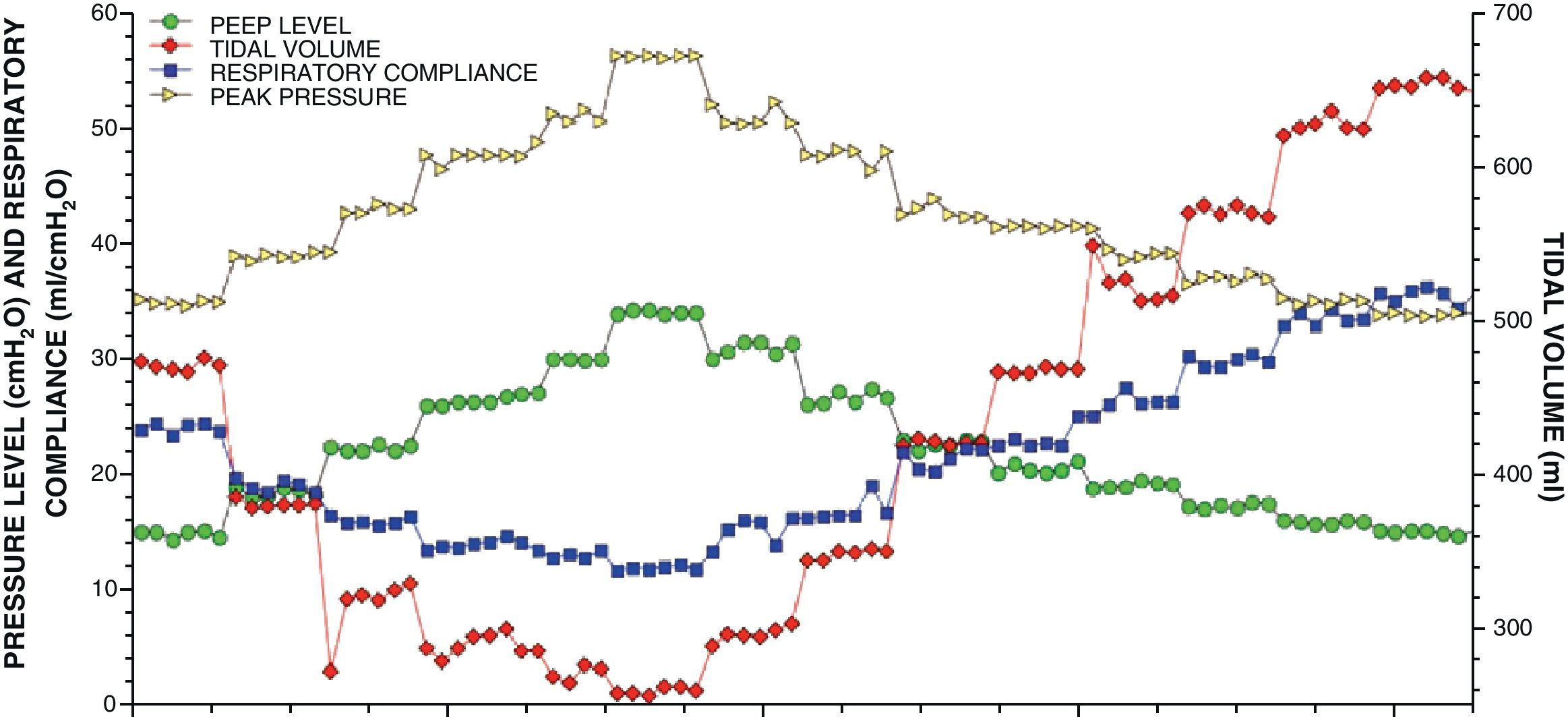
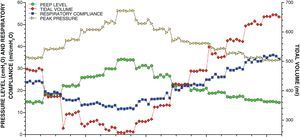
LRM was carried out by progressive PEEP increments (4cmH2O every 3min) until reaching 32–36cmH2O with a fixed ventilation pressure over PEEP (15–20cmH2O); the open lung PEEP was selected according to the maximum Cr measured during the PEEP decrement phase16,17 (Fig. 1). In 68 patients, the data referred to respiratory mechanics were recorded on a continuous basis every 30s using a spirometry module connected to the tracheal tube inlet (MCOVX, Datex-Ohmeda, Helsinki, Finland) and integrated in the patient bedside monitor. In the rest of the patients the data were obtained with the pressure and flow transducers of the ventilators. The most relevant aspects of LRM are described in detail in the accompanying article.18
After performing LRM and selecting the open lung PEEP, we maintained the pressure controlled ventilation mode with ventilation pressure for a tidal volume of 6–8ml/kg; respiratory frequency <35rpm; sufficient inspiratory time to allow alveolar pressure and airway pressure to equilibrate at the end of inspiration; and FiO2 for maintaining SpO2 between 90 and 96%. Although the time cycled pressure controlled mode was chosen during the most critical periods, the flow cycled pressure assisted or supported mode was used during the patient improvement and recovery phase. The withdrawal of open lung ventilation was carried out gradually, placing priority on the reduction of FiO2 and of ventilation pressure over the decrease in PEEP. The PEEP level was lowered in decrements of 2cmH2O (never more than 4cmH2O in the same day), provided there were no changes in tidal volume with the same ventilation pressure, or in SpO2 with the same FiO2. When any of these conditions were not met, we returned to the previous PEEP level, postponing the next attempt to reduce PEEP for at least 24h.
All patients were ventilated with a Servo 300 (Siemens-Elema AB, Solna, Sweden) or Puritan Bennet 840 ventilator (Tyco Healthcare, Gosport, United Kingdom) connected to a closed system for the aspiration of secretions. Special care was taken to avoid disconnections of the respiratory circuit, establishing the indication of airway secretions aspiration in accordance with the presence of notches in the expiratory flow wave.19 Only in the case of open disconnection of the circuit (accidental, for patient transfer, or for performing fibrobronchoscopy) was new LRM performed and open lung ventilation was restarted. We applied permissive hypercapnia (provided the central venous pH was ≥7.15) and placement of the patient in prone decubitus, in accordance with the indications of the physicians in charge of the patient.
The ventilatory parameters immediately before and after LRM and during the following four days were obtained from the electronic records filed with the S/5 Collect program (Datex-Ohmeda, Helsinki, Finland), and from the hourly nursing annotations during the time of open lung ventilation. The diagnosis of barotrauma was established from the presence of pneumothorax or subcutaneous emphysema in the portable chest X-rays. To this effect, X-ray was obtained before and after LRM, and at least once a day for the duration of respiratory failure.
The statistical analysis was carried out using the MedCalc 11.1.7 package (MedCalc Software, Mariakerke, Belgium). The data are presented as the mean±deviation, with statistical significance being considered for P<0.05. Continuous variables were analyzed using the Student t-test or Mann–Whitney U-test, depending on their distribution (Agostino–Pearson test). In turn, dichotomic variables were analyzed using the chi-squared test or Fisher exact test.
ResultsA total of 100 patients were included during the study period: 64 males and 36 females. The mean age was 49±15 years, and the mean APACHE II score in the first 24h of admission was 18±7. Fifty-seven patients were considered to have primary lung injuries: pneumonia in 50 and chest trauma in 7. Among the remaining 43 patients, lung injury was considered to be secondary or of extrapulmonary origin in 29 cases, and of uncertain or multifactorial origin in 14 patients. Regarding the patients with pneumonia, no microorganism was isolated in 11 subjects, while in the remaining 39 patients the causal microorganisms were influenza virus A (H1N1) in 12 cases, Legionella pneumophila in 5, Pneumocystis jiroveci in 5, Streptococcus pneumoniae in 5, gramnegative microorganisms in 5 (4 cases of Pseudomonas aeruginosa and one case of Haemophilus influenzae), Varicella-zoster in 4, Staphylococcus aureus in 2, and Mycobacterium tuberculosis in one patient. Of these patients with pneumonia, 10 presented advanced hematological disease, including 7 with bone marrow transplantation, and 5 were infected with the human immunodeficiency virus (HIV).
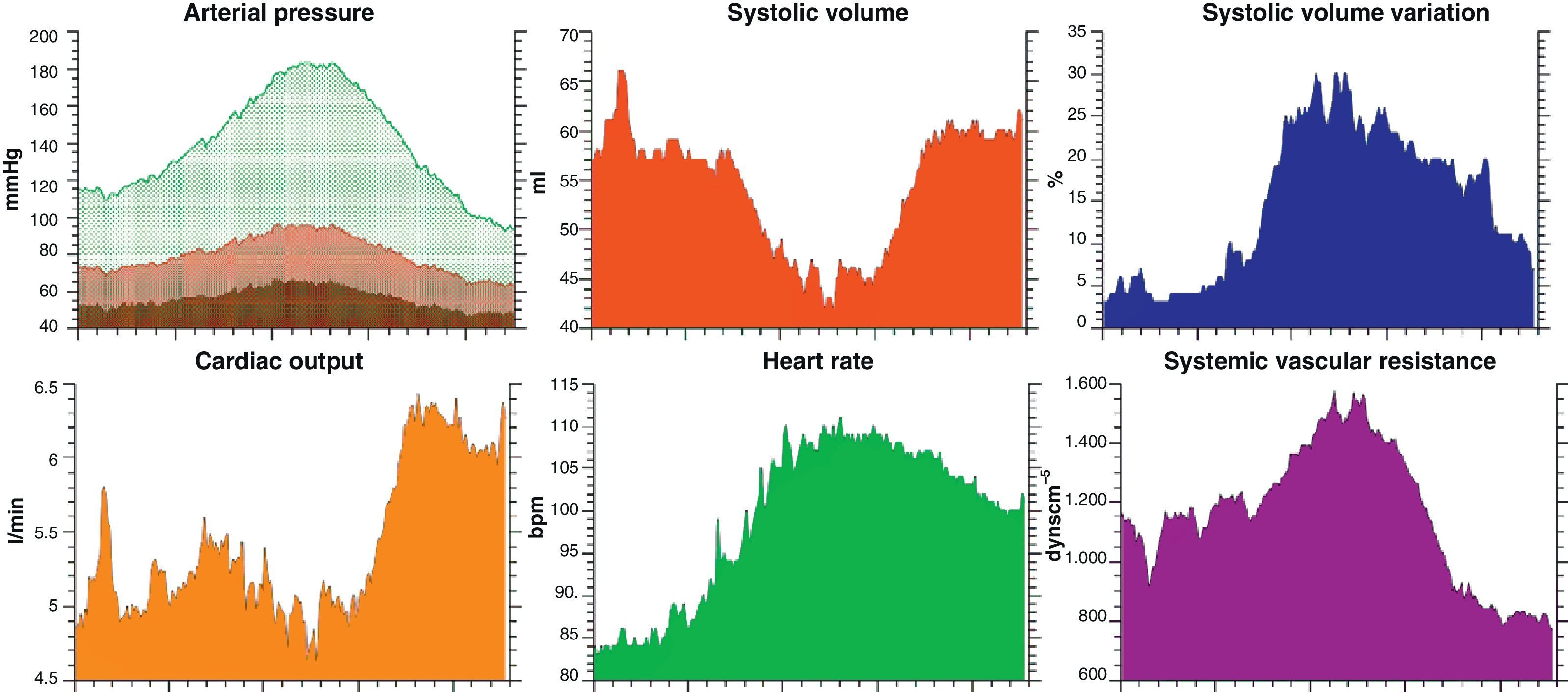
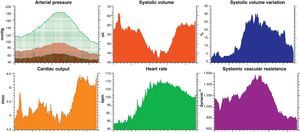
Global mortality in the ICU was 41%. Eight patients required tracheostomy and three needed rescue therapy with corticosteroids. Ventilation in prone decubitus was used in 43 patients. At the time of inclusion, 90 patients were subjected to advanced hemodynamic monitorization: 6 with a pulmonary artery catheter (Vigilance monitor, Edwards Lifesciences, LLC, Irvine, CA, USA), 20 with PiCCO plus or PiCCO2 (Pulsion Medical Systems, Munich, Germany) (Fig. 2), 42 with esophageal echodoppler (Hemosonic 100, Arrow Intl., Everett, USA), 16 with esophageal Doppler (CardioQ-ODM, Deltex Medical, Chichester, United Kingdom), and 6 patients with FloTrac-Vigileo (Edwards Lifesciences LLC, Irvine, CA, USA). A total of 51 patients were receiving treatment with noradrenalin, dobutamine or both, at the time of LRM and the start of open lung ventilation. Table 1 shows the main respiratory parameters of the 68 patients monitored with the lung function module, complemented by the nursing annotations during the subsequent four days.
Principal lung function parameters in the study population (n=68).
| Pre-LRM | Post-LRM | 24h OLV | 48h OLV | 72h OLV | 96h OLV | |
| PEEP (cmH2O) | 13.3±2.5 | 18.5±3.0* | 18.3±3.1* | 17.7±3.2* | 16.6±3.3* | 16.2±3.2* |
| Peak pressure (cmH2O) | 34.4±5.6 | 33.3±4.3 | 33.7±4.8 | 32.9±5.1 | 31.5±5.0† | 31.4±5.9† |
| Ventilation pressure (cmH2O) | 21.2±4.6 | 14.9±3.6* | 15.4±4.3* | 15.3±4.3* | 14.6±4.0* | 15.1±4.5* |
| Mean pressure (cmH2O) | 20.0±3.2 | 23.3±3.0* | 23.3±3.0* | 22.5±3.0* | 21.2±3.2 | 21.0±3.5 |
| Tidal volume (ml) | 473±92 | 448±100 | 475±89 | 477±103 | 494±96 | 498±106 |
| SpO2/FiO2 | 113±32 | 172±45* | 181±48* | 190±48* | 205±64* | 206±58* |
FiO2: inhaled oxygen fraction; PEEP: positive end-expiratory pressure; pre-LRM: values obtained immediately before pulmonary recruitment maneuvering; post-LRM: values obtained immediately after pulmonary recruitment maneuvering; SpO2: oxygen saturation determined by pulsioximetry; OLV 24h, 48h, 72h and 96h: values obtained after the first 24, 48, 72 and 96h of open lung ventilation.
P<0.0001.
P<0.001 with respect to the pre-LRM value.
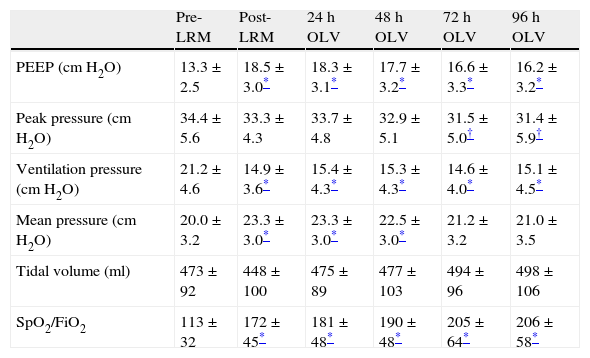
With the application of LRM and the start of open lung ventilation, Cr increased from 25.1±8.3ml/cmH2O (95%CI 23–27ml/cmH2O) to 31.5±9.7ml/cmH2O (95%CI 29–34ml/cmH2O) (P<0.0001), and the PEEP level and mean airway pressure increased, with a drop in ventilation pressure (Table 1).
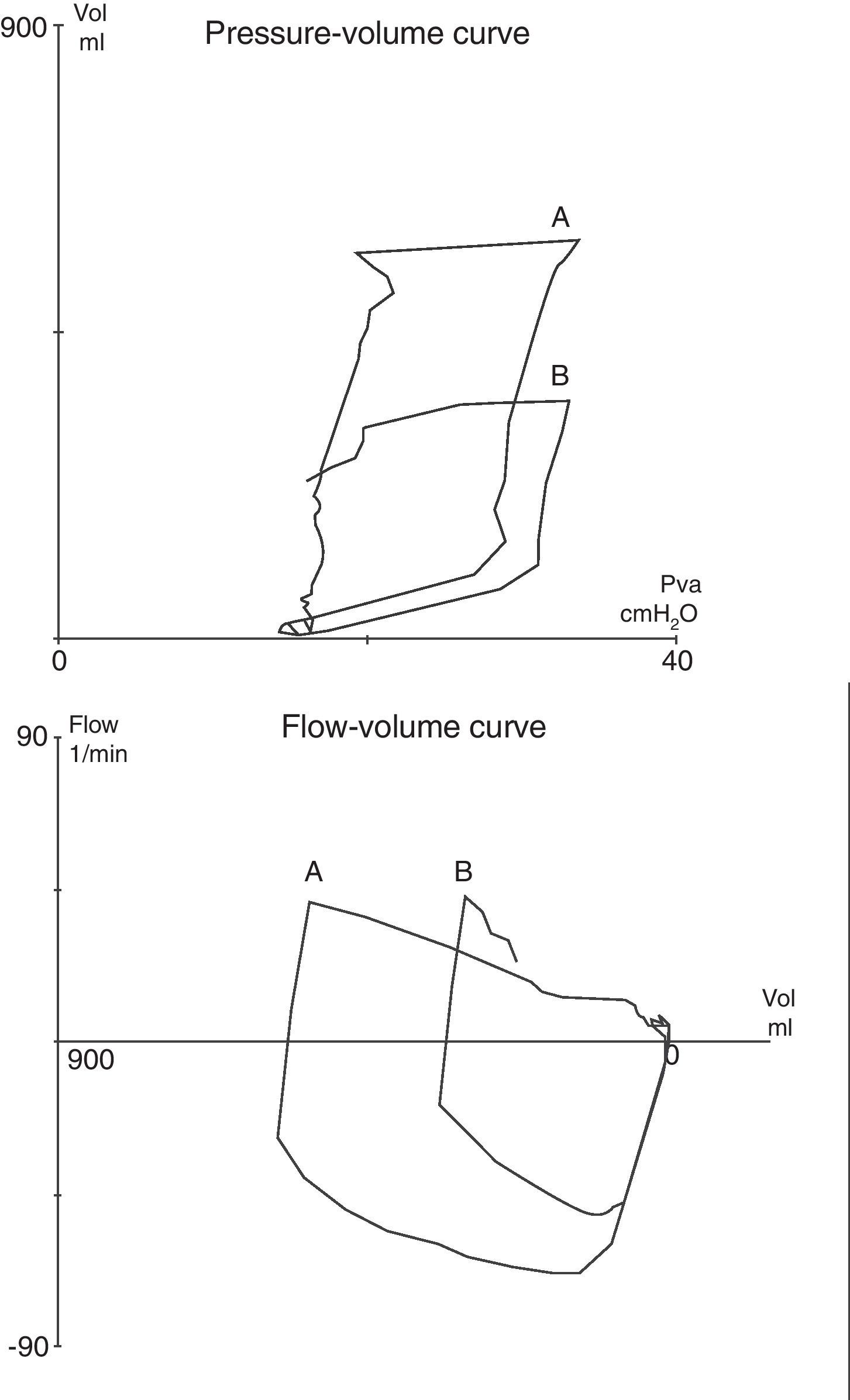
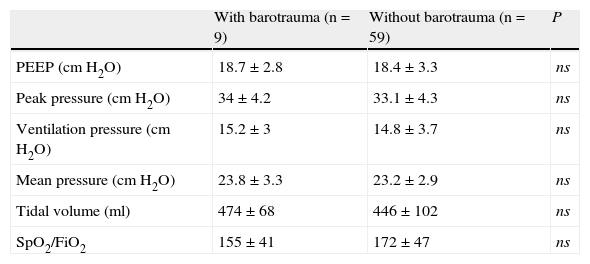
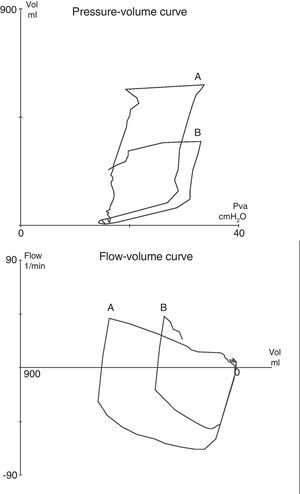
Barotrauma was detected in 9 of the 100 patients (9%): pneumothorax in 7 cases (7%) and subcutaneous emphysema in two cases. On establishing comparisons with the patients without barotrauma, no significant differences were found in the main ventilatory measures (Table 2). Likewise, mortality was similar in both groups (55% vs 40%; P=ns). Clinically, barotrauma was suspected in only two patients: one with tension pneumothorax and another with bilateral pneumothorax. As these patients were ventilated in pressure-controlled mode, they both showed an important reduction (≈50%) in tidal volume with pulmonary hypoventilation–though without changes in airway pressures or relevant hemodynamic alterations (Fig. 3). The placement of a pleural drain in both cases revealed the appearance of a bronchopleural fistula; as a result, open lung ventilation was suspended, and only one of these patients survived. In the remaining 7 patients, barotrauma constituted a finding of the control chest X-ray study, with no respiratory or hemodynamic changes. Accordingly, once the pleural drain had been placed and the posterior X-ray study confirmed resolution of the pneumothorax without bronchopleural fistulization, open lung ventilation was maintained. In the three of these 7 patients who survived, barotrauma appeared immediately after LRM (one with subcutaneous emphysema and two with pneumothorax), while in the four patients who died (one with subcutaneous emphysema and 3 with pneumothorax), barotrauma appeared on days 2, 11, 17 and 26 after starting open lung ventilation. In no patient was a direct relationship established between death and barotrauma, though when the latter manifested after the first week of open lung ventilation, all the affected subjects died.
Principal lung function parameters corresponding to the mean value of the first four days of open lung ventilation of the patients with and without barotrauma.
| With barotrauma (n=9) | Without barotrauma (n=59) | P | |
| PEEP (cmH2O) | 18.7±2.8 | 18.4±3.3 | ns |
| Peak pressure (cmH2O) | 34±4.2 | 33.1±4.3 | ns |
| Ventilation pressure (cmH2O) | 15.2±3 | 14.8±3.7 | ns |
| Mean pressure (cmH2O) | 23.8±3.3 | 23.2±2.9 | ns |
| Tidal volume (ml) | 474±68 | 446±102 | ns |
| SpO2/FiO2 | 155±41 | 172±47 | ns |
FiO2: inhaled oxygen fraction; PEEP: positive end-expiratory pressure; SpO2: oxygen saturation determined by pulsioximetry.
Pressure–volume (at top) and flow–volume (at bottom) tracings obtained in patient 6: (A) at baseline, and (B) during tension pneumothorax. As the patient was ventilated in pressure-controlled mode, the appearance of pneumothorax manifested as an acute drop in tidal volume, without changes in the airway pressures.
In all patients who developed barotrauma, the lung injury was of primary origin (7 cases of pneumonia and 2 cases of chest trauma)–this representing a barotrauma incidence in this subgroup of patients of 16% (14% of the patients with pneumonia and 28% of the patients with chest trauma). Within this subgroup with primary lung injuries, the mortality rate was similar in patients with and without barotrauma (55 vs 56%; P=ns). The most relevant data of the patients who developed barotrauma are presented below:
Patient 1: Aged 23 years, with morbid obesity and bilateral community-acquired pneumonia (H. influenzae). Bilateral subcutaneous emphysema was detected from the first X-rays after LRM, while being ventilated with PEEP 24cmH2O and a ventilation pressure of 16cmH2O. Open lung ventilation was maintained, with a favorable course and weaning from ventilation 9 days later.
Patients 2 and 3: Aged 19 and 58 years, respectively, both with severe chest trauma. LRM was performed immediately after tracheal intubation, with identification from the first X-rays of a small unilateral apical pneumothorax in both patients. Pleural drainage was carried out, with ventilatory support comprising PEEP 17 and 21cmH2O and a ventilation pressure of 15 and 10cmH2O, respectively. Both patients evolved favorably, with weaning from ventilation on days 6 and 7.
Patient 4: Aged 39 years and diagnosed with acute myeloid leukemia (M4FAB), subjected to allogenic transplantation 15 months earlier. Graft-versus-host disease treated with immune suppressors, with late post-transplantation disease relapse complicated by pneumonia (P. jiroveci). A pneumomediastinum and unilateral subcutaneous emphysema were identified from the second X-ray study made after LRM (24h later), while ventilated with PEEP 14cmH2O and a ventilation pressure of 16cmH2O. On day 5 the patient suffered hemorrhagic cerebral infarction in the territory of the right middle cerebral artery, which rapidly led to a fatal outcome.
Patient 5: Aged 38 years with HIV infection (stage 3C, viral load 129,000copies/ml) and pneumonia due to P. jiroveci. On day 5 of open lung ventilation (PEEP 14cmH2O and a ventilation pressure of 10cmH2O) the patient developed bilateral pneumothorax with an episode of lung hypoventilation without hemodynamic involvement. The placement of two chest drains was required, with the suspension of open lung ventilation to lower the airway pressures. The patient died three days later due to refractory septic shock (blood cultures positive for Candida glabrata).
Patient 6: Aged 36 years and admitted due to bilateral pneumonia (S. pneumoniae). Early LRM was performed, with the development of tension pneumothorax three days later, while ventilated with PEEP 16cmH2O and a ventilation pressure of 16cmH2O. Clinically, the patient presented lung hypoventilation without cardiocirculatory repercussions. A chest drain was placed, with identification of a bronchopleural fistula equivalent to 40–50% of the tidal volume, requiring the suspension of open lung ventilation to maximally lower the pressures in the airway. The thoracic computed tomography study confirmed necrotizing pneumonia. The patient required a percutaneous tracheostomy and mechanical ventilation during 19 days, with a favorable outcome.
Patient 7: Aged 54 years, with liver cirrhosis of alcoholic origin and bilateral pneumonia, but without isolation of any causal microorganism. On day 3 of mechanical ventilation, LRM was performed and open lung ventilation was started (PEEP 22cmH2O and a ventilation pressure of 14cmH2O), with an initially favorable course. The patient condition posteriorly worsened, with signs of new lung infection. Repeat LRM was therefore performed on day 11. On this occasion we selected PEEP 18cmH2O and a ventilation pressure of 20cmH2O. Three days later, right apical pneumothorax was detected from the thoracic computed tomography scan, which confirmed necrotizing pneumonia, and a pleural drain was placed. The patient died 48h later with fever (41°C) and refractory shock.
Patient 8: Aged 42 years and diagnosed with acute myeloid leukemia, subjected to allogenic bone marrow transplantation. The patient developed bilateral pneumonia, without isolation of any causal microorganism. The most likely diagnosis was therefore taken to be acute idiopathic pneumonia syndrome. LRM proved necessary on several occasions due to refractory severe hypoxemia. On day 26 of open lung ventilation, and after having performed new LRM, the chest X-rays detected right apical pneumothorax, which was drained without changes in lung function. The patient developed multiorgan failure and died 6 days later.
Patient 9: Aged 35 years, with morbid obesity and severe bilateral pneumonia due to influenza virus A (H1N1) infection. From admission, the patient was placed in prone decubitus with PEEP 18cmH2O, maintained during the first 48h due to the severity of the hypoxemia. LRM was performed on day 3, with open lung PEEP 28cmH2O. Although the procalcitonin value was 0.3 upon admission, by day 3 it had exceeded 100. Co-existing severe bacterial infection was therefore suspected. Blood and bronchial aspirate cultures revealed Candida albicans and extended spectrum β-lactamase (ESBL) producing Klebsiella pneumoniae. On day 17 of open lung ventilation, while ventilated with PEEP 20cmH2O and a ventilation pressure of 26cmH2O, the chest X-rays revealed right pneumothorax that was evacuated with a pleural drain. The patient died as a result of septic shock 12 days later – the blood cultures being positive for Enterococcus faecium.
DiscussionIn this study of 100 patients with severe respiratory failure and bilateral lung infiltrates subjected to open lung ventilation with lung recruitment maneuvering (LRM) (via stepwise PEEP increments and decrements, and the selection of open lung PEEP according to the maximum Cr), barotrauma had an incidence of 9% (pneumothorax in 7%). It exclusively affected patients with primary lung injury (pneumonia and chest trauma); as a result, the incidence in this subgroup was high (16%). In most cases barotrauma was identified from the control X-rays, without respiratory or hemodynamic changes, and with no need to suspend open lung ventilation. The appearance of barotrauma was not related to greater respiratory pressures or volumes, and was not associated to increased mortality.
Barotrauma remains one of the most serious complications in patients subjected to mechanical ventilation, with a reported incidence of up to 48% in the first series of patients with acute respiratory distress syndrome1 – though recent studies involving protective ventilatory strategies have recorded a much lower incidence (≈10%).2–5 When such strategies are moreover complemented by LRM and open lung PEEP, the incidence of barotrauma remains low: 7% in the pioneering work of Amato et al.,7 and 11.2% in the Lung Open Ventilation Study, which included 475 patients subjected to an open lung ventilation strategy.20 These results are consistent with our own findings, although our LRM protocol and the way of titrating open lung PEEP were different, with a greater pressure-time product21 and a higher open lung PEEP level (18.5±3cmH2O vs 16.3±0.7 and 14.6±3.4cmH2O in the study of Amato and in the Lung Open Ventilation Study, respectively). However, neither of these studies offered a detailed description or comparative analysis of the patients who developed barotrauma.
In our series, pneumonia was the most frequent cause of lung injury in the patients with barotrauma, with a pneumothorax incidence of 10% (5/50), which is similar to the percentage reported by Boussarsar et al. in a group of 116 patients.4 Pneumonia can favor the development of barotrauma through different mechanisms. Firstly, in patients with P. jiroveci infection, as in patients 4 and 5 of our series, subpleural necrosis facilitates the formation of large cysts and their subsequent rupture, with the frequent development of pneumothorax (in both spontaneous and mechanical ventilation)–with a reported incidence of 47% and a high percentage of bilateral pneumothorax (37%).22,23 Apart from this infection, necrosis of the lung tissues can also complicate infection due to other microorganisms such as S. pneumoniae or anaerobic bacteria. This is common among alcoholic patients,24 as in patients 6 and 7 of our series. Lastly, another differentiating feature of pneumonia with respect to other forms of respiratory failure, particularly those of extrapulmonary origin, is the fact that lung consolidation predominates over lung collapse–as a result of which the recruitment potential is lower, and therefore the transpulmonary pressures during LRM are higher, with an increased risk of overdistension and barotrauma.25–28
In addition to the 6 patients with pneumonia, two patients with chest trauma and severe bilateral lung contusion also suffered barotrauma–in both cases detected immediately after LRM, without having to suspend open lung ventilation, and with a favorable outcome. Chest trauma has been considered a risk factor for barotrauma, particularly in relation to barotrauma manifesting in the first 24h of mechanical ventilation,29 as was the case in these two patients. Therefore, although some authors have found that open lung ventilation can be safely used in chest trauma patients,30 other investigators consider chest trauma to be an exclusion criterion for such ventilation.31
Lastly, in patients 7 and 8 of our series, LRM was repeated after the second week of mechanical ventilation (on days 14 and 22, respectively), preceding the appearance of barotrauma. According to the observations of Gattinoni et al.,1 the structural changes that occur after the third week facilitate the appearance of barotrauma, thus requiring us to be particularly careful in this evolutive phase of lung injury. Accordingly, the maintenance of open lung ventilation beyond two weeks with repeated LRM probably exerted a direct influence upon the generation of barotrauma in these patients.
Pulmonary barotrauma is usually identified from routine X-ray studies,24 though it is sometimes accompanied by changes in the ventilatory parameters (worsened oxygenation and increased airway pressure), and less frequently by circulatory collapse in the case of tension pneumothorax.29,32 In 7 of our 9 patients, barotrauma was clinically silent and was identified from the control X-rays. In only two patients (one with tension pneumothorax and the other with bilateral pneumothorax) was it accompanied by suspect clinical manifestations. In both cases, barotrauma was characterized by pulmonary hypoventilation without hemodynamic alterations other than a slight increase in heart rate. In the 5 patients in which pneumothorax developed without changes in pulmonary function, and its radiological resolution was confirmed after pleural drainage, open lung ventilation was continued without reappearance of pneumothorax or bronchopleural fistulization. Only in the two patients in which the condition was accompanied by pulmonary hypoventilation did we have to modify the ventilatory strategy due to the presence of a bronchopleural fistula.29,33
Our study is not without limitations. Firstly, this is a retrospective survey based on the review of databases, electronic records and clinical histories–some of which could not be retrieved for detailed evaluation (including one patient with pneumothorax). Secondly, open lung ventilation, while generally accepted and implemented in our ICU, was not applied in all the patients who met the corresponding inclusion criteria. We are therefore unable to rule out the possibility that patient selection (in some cases on an arbitrary basis) might have conditioned the results obtained. Lastly, we based the diagnosis of barotrauma exclusively on the presence of pneumothorax and subcutaneous emphysema, neglecting other no less important forms of barotrauma due to the difficulties sometimes found in interpreting the portable X-ray findings in our setting.34 As a result, the diagnosis of barotrauma may not have been correctly established in all the patients. This was confirmed in one case where a thoracic computed tomography scan proved necessary. Nevertheless, despite these limitations, we consider that our study contributes information of relevance for clinicians wishing to use this form of ventilation. Firstly, we recommend remaining alert to the appearance of this complication, particularly in patients with primary lung injury and, more specifically, in those with pneumonia, particularly involving a necrotizing type such as infection due to P. jiroveci, where the risk of barotrauma is so high that LRM and open lung ventilation probably should not be used. Secondly, we consider that the early application of LRM (<24h of evolution) should be avoided in patients with chest trauma, in the same way as late LRM (>2 weeks) in the global population, since at this time there possibly are already structural changes that increase lung vulnerability and make barotrauma more likely. On the other hand, if we choose pressure controlled ventilatory modes, we must rule out barotrauma on evidencing hypoventilation episodes secondary to a lowering of tidal volume, even if there are no hemodynamic changes. Lastly, and in accordance with our own experience, we do not consider it necessary to suspend open lung ventilation when radiological signs of barotrauma appear, and the existence of bronchopleural fistulization, or cardiocirculatory or lung ventilation impairment is discarded.
In conclusion, in our series of 100 patients subjected to LRM and open lung ventilation, barotrauma exclusively affected individuals with primary lung injury, in which the incidence was high (16%). In most cases, barotrauma was a finding of the control X-rays studies, without respiratory or hemodynamic changes, and without having to suspend open lung ventilation. The appearance of barotrauma was not related to greater respiratory pressures or volumes, and was not associated to increased mortality.
Conflict of interestM. Ignacio Monge-Garcia is an Edwards Lifesciences consultant. The rest of the authors declare no conflicts of interest.
Please cite this article as: Gil Cano A, et al. Incidencia, características y evolución del barotrauma durante la ventilación mecánica con apertura pulmonar. Med Intensiva. 2012;36:335–42.