To identify the resources related to the care of critically ill patients in Spain, which are available in the units dependent of the Services of Intensive Care Medicine (ICM) or other services/specialties, analyzing their distribution according to characteristics of the hospitals and by autonomous communities.
DesignProspective observational study.
SettingSpanish hospitals.
ParticipantsHeads of the Services of ICM.
Main outcome variablesNumber of units and beds for critically ill patients and functional dependence.
ResultsThe total number of registries obtained with at least one Service of ICM was 237, with a total of 100,198 hospital beds. Level III (43.5%) and level II (35%) hospitals predominated. A total of 73% were public hospitals and 55.3% were non-university centers. The total number of beds for adult critically ill patients was 4,738 (10.3/100,000 inhabitants). The Services of ICM registered had available 258 Intensive Care Units (ICUs), with 3363 beds, mainly polyvalent ICUs (81%) and 43 intermediate care units. The number of patients attended in the Services of ICM in 2008 was 174,904, with a percentage of occupation of 79.5%.
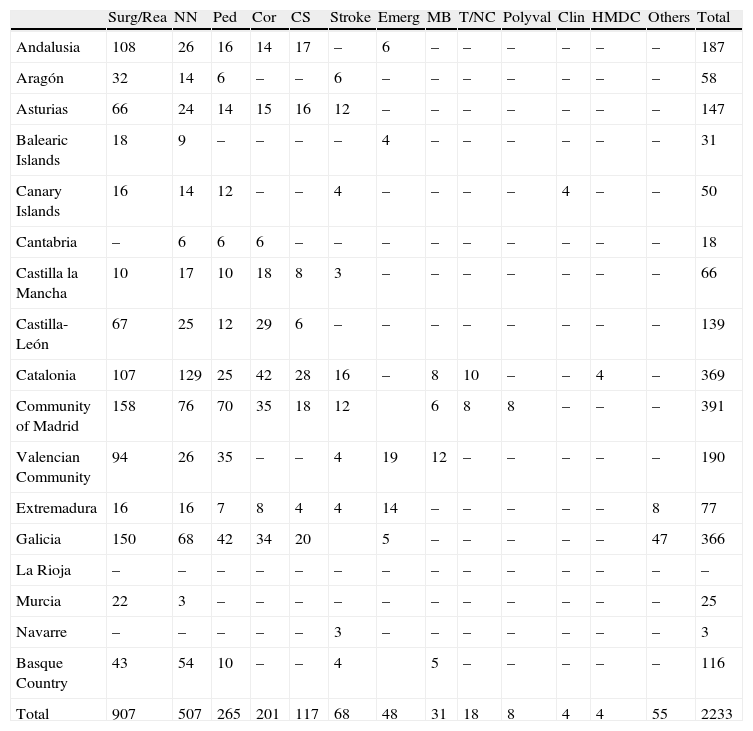
A total of 228 units attending critically ill patients, which are dependent of other services with 2233 beds, 772 for pediatric patients or neonates, were registered. When these last specialized units are excluded, there was a marked predominance of postsurgical units followed by coronary and cardiac units.
ConclusionsSeventy-one per cent of beds available in the Critical Care Units in Spain are characterized by attending severe adult patients, are dependent of the Services of ICM, and most of them are polyvalent.
Identificar los recursos existentes con relación a la atención de pacientes críticos en España, ubicados en unidades asistenciales dependientes de Servicios de Medicina Intensiva (SMI), o de otros servicios/especialidades, analizando su distribución según las características de los hospitales, y por comunidades autónomas.
DiseñoEstudio prospectivo, observacional.
ÁmbitoHospitales españoles.
ParticipantesJefes de SMI.
Variables de interés principalesNúmero de unidades y camas de pacientes críticos y dependencia funcional.
ResultadosEl número total de registros obtenidos con al menos un SMI fueron 237, con un total de camas hospitalarias de 100.198. Predominaron los hospitales de nivel III (43,5%) y nivel II (35%). El 73% de los hospitales fueron de gestión pública y el 55,3%, no universitarios. El número total de camas de críticos de adultos identificadas fue de 4.738 (10,3/100.000habitantes). Los SMI registrados disponen de 258 UCI, con 3.363 camas, predominando las UCI polivalentes (81%), y de 43 Unidades de Cuidados Intermedios. El número de pacientes atendidos en los SMI durante el año 2008 fue de 174.904, con un porcentaje de ocupación del 79,5%.
Se identificaron 228 unidades asistenciales que atienden pacientes críticos dependientes de otros servicios con 2.233 camas, 772 pediátricas o neonatales. Excluyendo estas últimas, hay un predominio marcado de unidades posquirúrgicas, seguido de unidades coronarias y de cirugía cardiaca.
ConclusionesEl 71% de las camas disponibles en las unidades de críticos en España, que atienden a pacientes adultos graves, son dependientes de los SMI y, en su mayoría, son polivalentes.
Intensive Care Medicine is one of the principal elements in modern healthcare systems, and represents the last link in the chain of critical patient care. A growing demand for critical care is expected in the coming years, and an important percentage of the population will have to be attended in Departments of Intensive Care Medicine (DICMs), where the mortality rate is inevitably high, and where an important proportion of all healthcare resources are consumed.1 Current hospitals, with a tendency to significantly reduce the number of available beds, have increased their activities in Intensive Care Medicine in recent years. This discipline is therefore in growing demand and implies important healthcare costs. In the United States, it has been estimated that over one-half of the population will require admission to an Intensive Care Unit (ICU) at some point in life, and that an important percentage of these patients will die in such Units, consuming 0.66% of the gross domestic product of the country.2 This increase in demand, along with the limitation of resources, makes it necessary to precisely establish the availability of such services.
On the other hand, specific situations occasionally may arise in which the demand for critical care increases unexpectedly–as in the recent influenza A pandemic.
Previous studies have demonstrated the difficulty of obtaining reliable information referred to critical care beds, and point to the need to seek such information through different data sources.3 In this context, the lack of up-to-date information, and particularly the dynamic nature of the data, make it difficult to obtain accurate statistics.
The variability of the definitions used, and the heterogeneous organizational models in critical patient care, in turn make it difficult to compare data among different studies, and obstruct the obtainment of reliable information for decision making referred to planning and management destined to adapt the resources to the current and future demands.
The Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC), being aware of these needs, designed the present study to identify the existing resources for the care of critically ill patients in Spain. Specifically, the study examines the number of DICMs, Critical Care Units (CCUs) and critical care beds dependent upon the DICMs, as well as the care Units that attend critical patients dependent upon other Departments/specialties, and conducts an analysis of their distribution according to the characteristics of the hospitals, and by regions or Spanish Autonomous Communities.
Materials and methodsThe study was carried out from the central offices of the SEMICYUC.
Identification and collection of information on the Departments of Intensive Care Medicine and Intensive Care UnitsData collection was carried out between October 2010 and April 2011, in different phases:
- -
Phase 1. The initial identification of DICMs and ICUs was made from the databases of the SEMICYUC (list of 285 centers), Autonomous Community Societies, the general hospital catalog of the Spanish Ministry of Health (907 centers), and the list of centers participating in the severe influenza A study (a specific pandemic phase survey).
- -
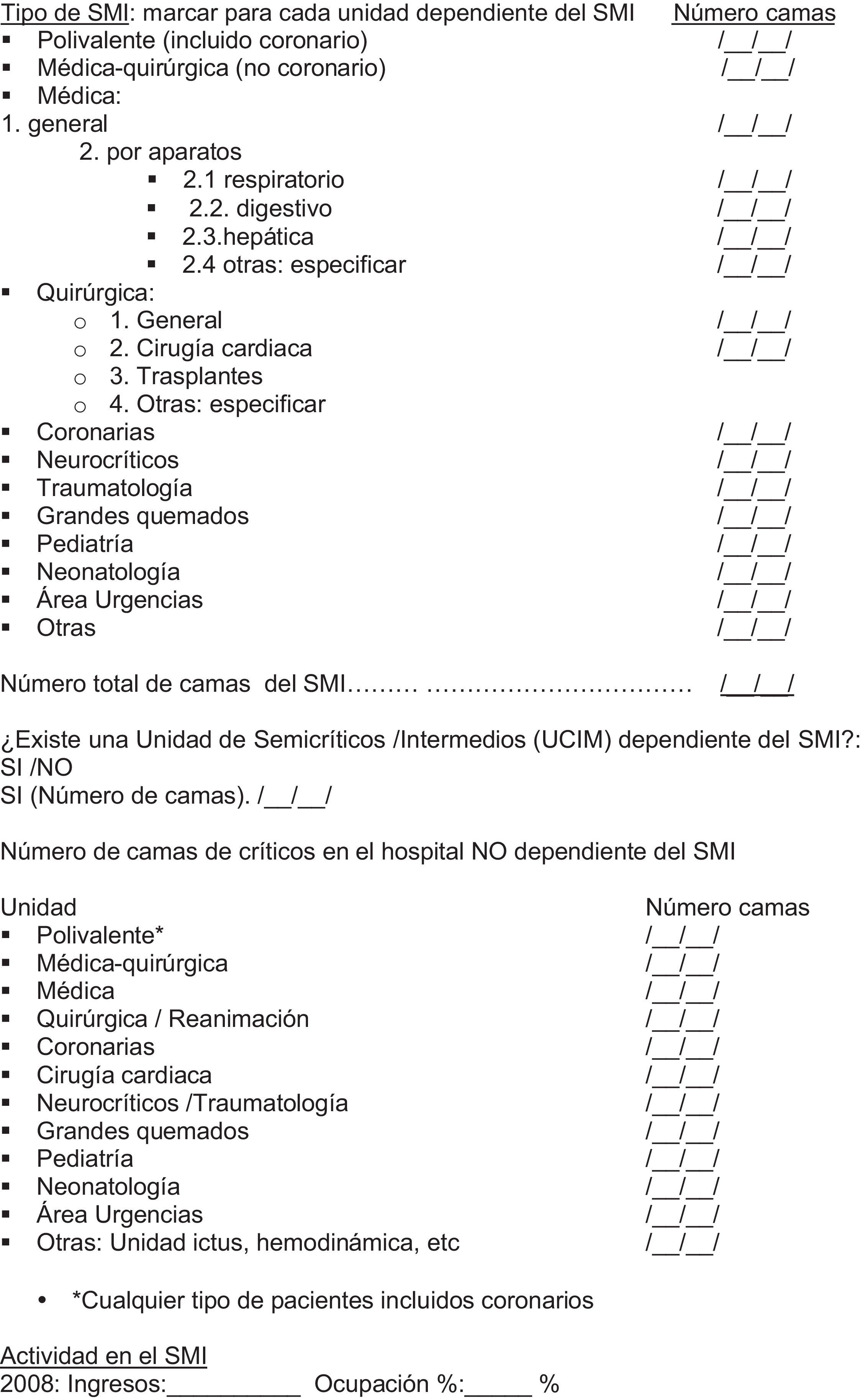
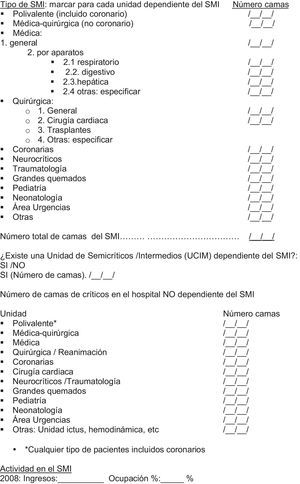
Phase 2. An e-mail was sent to all the registered DICMs, inviting the Director or Head of Department to complete an epidemiological survey (Annex 1). Provided there were no doubts or uncertainties in the replies obtained, these Departments were included in the registry.
- -
Phase 3. In those cases in which there were doubts, or when the survey was not completed at first request, a second recruitment attempt was made by telephone contact, with the purpose of collecting the necessary data or clarifying doubts referred to the information received.
- -
Phase 4. The data were contrasted by the Presidents of the different regional or Autonomous Community Societies pertaining to the national Scientific Society.
The following variables were analyzed: hospital (address, city, telephone, fax, web, corresponding Autonomous Community), number of beds in the hospital, hospital level (I, II, III), type of center (public, private, mixed), category (university or otherwise), information on the Head of Department (e-mail, contact telephone), and type and number of beds in the DICM. In those cases in which more than one Unit was dependent upon the DICM (ICU or CCU), we recorded the type and number of beds in each. The ICUs were classified as follows: clinical–surgical (including Coronary Units), clinical–surgical (non-Coronary Units), clinical, surgical, cardiac surgery, transplants, coronary, neurocritical, traumatology, major burns, pediatrics, neonatology, emergencies area, and as the total number of beds in the DICM. We likewise documented the activity of the DICM in relation to the number of admissions, and percentage occupation during the year 2008. On the other hand, we recorded the type of Units and the number of critical care beds not dependent upon the DICM, and which were classified as follows: polyvalent, clinical–surgical, medical, surgical/resuscitation, coronary, cardiac surgery, neurocritical/traumatology, major burns, pediatrics, neonatology, emergencies area, Stroke Unit, hemodynamics, and others.
DefinitionsThe hospitals were classified as corresponding to three different levels, based on the definitions established by the guide for the coordination, evaluation and management of Departments of Intensive Care Medicine, published by the Spanish INSALUD in 19973: level i (district), level ii (specialties), level iii (regional).4
Critical Care Unit or Intensive Care UnitA differentiated physical space in which critical patients are attended. These Units can be polyvalent or specialized in the management of certain diseases.
Department of Intensive Care MedicineA hospital Department directly dependent upon the hospital medical-management board, and directed by an intensivist. The DICM in turn can be composed of different CCUs.
Intermediate Care UnitA hospital area with sufficient technical and humans means to provide patient monitoring and care at a level lower than in the ICU, but far higher than in conventional hospital wards. Those dependent upon the DICM have been included.
A given DICM may be composed of one or more Units all dependent upon the same DICM.
A DICM may comprise different structural units (ICU) or areas within the hospital, provided they are under the supervision of the same Director or Head of Department.
A hospital may have different DICMs (different managements) and other CCUs not forming part of the DICM as such. Depending on the organizational characteristics of each hospital center, critical patients may be attended by other Departments separate from the DICM.
Data processing and statistical analysis was carried out using MS Excel (2003). Qualitative variables are reported with the corresponding percentage distribution.
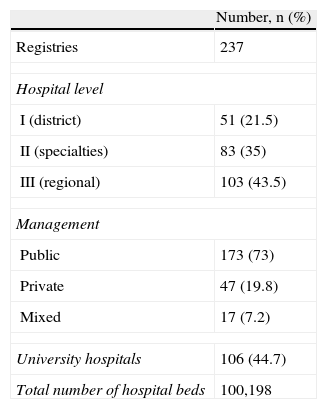
ResultsA total of 237 centers had at least one DICM. We did not include hospitals lacking a DICM, or the 48 hospitals that failed to answer the survey. There was a predominance of level iii hospitals (43.5%), followed by level ii hospitals (35%). In turn, most of the hospitals (73%) were public centers belonging to the Spanish National Health System. A little over one-half of the hospitals (55.3%) were non-university centers. The total number of hospital beds was 100,198 (Table 1).
The total number of critical care beds was 5596. After excluding the beds corresponding to neonatology, pediatrics and Stroke Units, this figure decreased to 4738. Adjustment to the Spanish population census of 1 April 2011 (46,148,605 inhabitants) in turn yielded 10.3 beds per 100,000 inhabitants.
Table 2 reports the Autonomous Communities, the number of DICMs surveyed, and the number of hospital beds.
Distribution of the number of hospital beds and Departments of Intensive Care Medicine surveyed among the different Autonomous Communities.
| Hospital beds | DICM | |
| Andalusia | 13,056 | 32 |
| Aragon | 3178 | 6 |
| Asturias | 5116 | 6 |
| Balearic Islands | 3007 | 8 |
| Canary Islands | 3132 | 8 |
| Cantabria | 847 | 1 |
| Castilla la Mancha | 3736 | 10 |
| Castilla-León | 6684 | 11 |
| Catalonia | 14,363 | 38 |
| Community of Madrid | 18,277 | 45 |
| Valencian Community | 10,278 | 32 |
| Extremadura | 2358 | 5 |
| Galicia | 8952 | 15 |
| La Rioja | 630 | 1 |
| Murcia | 2499 | 7 |
| Navarre | 610 | 2 |
| Basque Country | 3475 | 10 |
| Total | 100,198 | 237 |
DICM: Department of Intensive Care Medicine.
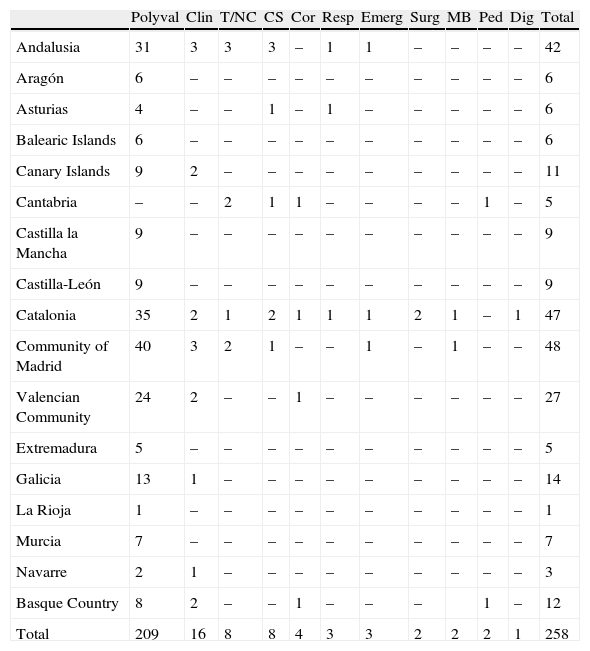
In the 237 registered centers, the DICMs comprised 258 ICUs or CCUs dependent upon the DICM, with 3363 available beds. The number of patients attended in these Units in the year 2008 totaled 174,904, with a percentage occupation of the Departments of 79.5%. The number of Intermediate Care Units dependent upon the DICM was 43.
Table 3 shows the number and type of CCUs dependent upon the DICM, and their distribution among the different Spanish regions or Autonomous Communities. A clear predominance of polyvalent ICUs is observed (clinical–surgical and coronary) (n=209, 81%), with a dominant presence in CCUs in the Communities of Madrid, Catalonia, Andalusia and Valencia, which account for 62.2% of the total.
Units dependent upon the Departments of Intensive Care Medicine. Number and type of ICUs according to Autonomous Communities.
| Polyval | Clin | T/NC | CS | Cor | Resp | Emerg | Surg | MB | Ped | Dig | Total | |
| Andalusia | 31 | 3 | 3 | 3 | – | 1 | 1 | – | – | – | – | 42 |
| Aragón | 6 | – | – | – | – | – | – | – | – | – | – | 6 |
| Asturias | 4 | – | – | 1 | – | 1 | – | – | – | – | – | 6 |
| Balearic Islands | 6 | – | – | – | – | – | – | – | – | – | – | 6 |
| Canary Islands | 9 | 2 | – | – | – | – | – | – | – | – | – | 11 |
| Cantabria | – | – | 2 | 1 | 1 | – | – | – | – | 1 | – | 5 |
| Castilla la Mancha | 9 | – | – | – | – | – | – | – | – | – | – | 9 |
| Castilla-León | 9 | – | – | – | – | – | – | – | – | – | – | 9 |
| Catalonia | 35 | 2 | 1 | 2 | 1 | 1 | 1 | 2 | 1 | – | 1 | 47 |
| Community of Madrid | 40 | 3 | 2 | 1 | – | – | 1 | – | 1 | – | – | 48 |
| Valencian Community | 24 | 2 | – | – | 1 | – | – | – | – | – | – | 27 |
| Extremadura | 5 | – | – | – | – | – | – | – | – | – | – | 5 |
| Galicia | 13 | 1 | – | – | – | – | – | – | – | – | – | 14 |
| La Rioja | 1 | – | – | – | – | – | – | – | – | – | – | 1 |
| Murcia | 7 | – | – | – | – | – | – | – | – | – | – | 7 |
| Navarre | 2 | 1 | – | – | – | – | – | – | – | – | – | 3 |
| Basque Country | 8 | 2 | – | – | 1 | – | – | – | 1 | – | 12 | |
| Total | 209 | 16 | 8 | 8 | 4 | 3 | 3 | 2 | 2 | 2 | 1 | 258 |
CS: cardiac surgery; Cor: coronary; Dig: digestive; MB: major burns; Clin: clinical; Ped: pediatric; Polyval: polyvalent (clinical/surgical/coronary); Surg: surgical; Resp: respiratory; T/NC: trauma/neurocritical; Emerg: emergencies.
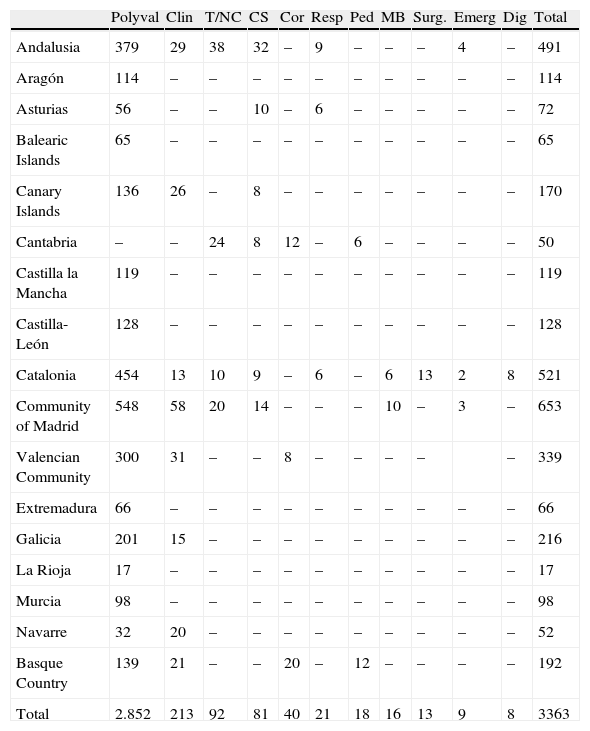
Table 4 in turn describes the number of beds according to the type of ICU in the Units dependent upon the DICMs. The largest number of beds correspond to the polyvalent Units, with a total of 2852, representing 84.8% of the resources, followed by the clinical ICUs, traumatologic/neurocritical Units and cardiac surgery Units, which respectively account for 6.3%, 2.7% and 2.4%.
Units dependent upon the Departments of Intensive Care Medicine. Number of beds according to type of ICU.
| Polyval | Clin | T/NC | CS | Cor | Resp | Ped | MB | Surg. | Emerg | Dig | Total | |
| Andalusia | 379 | 29 | 38 | 32 | – | 9 | – | – | – | 4 | – | 491 |
| Aragón | 114 | – | – | – | – | – | – | – | – | – | – | 114 |
| Asturias | 56 | – | – | 10 | – | 6 | – | – | – | – | – | 72 |
| Balearic Islands | 65 | – | – | – | – | – | – | – | – | – | – | 65 |
| Canary Islands | 136 | 26 | – | 8 | – | – | – | – | – | – | – | 170 |
| Cantabria | – | – | 24 | 8 | 12 | – | 6 | – | – | – | – | 50 |
| Castilla la Mancha | 119 | – | – | – | – | – | – | – | – | – | – | 119 |
| Castilla-León | 128 | – | – | – | – | – | – | – | – | – | – | 128 |
| Catalonia | 454 | 13 | 10 | 9 | – | 6 | – | 6 | 13 | 2 | 8 | 521 |
| Community of Madrid | 548 | 58 | 20 | 14 | – | – | – | 10 | – | 3 | – | 653 |
| Valencian Community | 300 | 31 | – | – | 8 | – | – | – | – | – | 339 | |
| Extremadura | 66 | – | – | – | – | – | – | – | – | – | – | 66 |
| Galicia | 201 | 15 | – | – | – | – | – | – | – | – | – | 216 |
| La Rioja | 17 | – | – | – | – | – | – | – | – | – | – | 17 |
| Murcia | 98 | – | – | – | – | – | – | – | – | – | – | 98 |
| Navarre | 32 | 20 | – | – | – | – | – | – | – | – | – | 52 |
| Basque Country | 139 | 21 | – | – | 20 | – | 12 | – | – | – | – | 192 |
| Total | 2.852 | 213 | 92 | 81 | 40 | 21 | 18 | 16 | 13 | 9 | 8 | 3363 |
CS: cardiac surgery; Cor: coronary; Dig: digestive; MB: major burns; Clin: clinical; Ped: pediatric; Polyval: polyvalent (clinical/surgical/coronary); Surg: surgical; Resp: respiratory; T/NC: trauma/neurocritical; Emerg: emergencies.
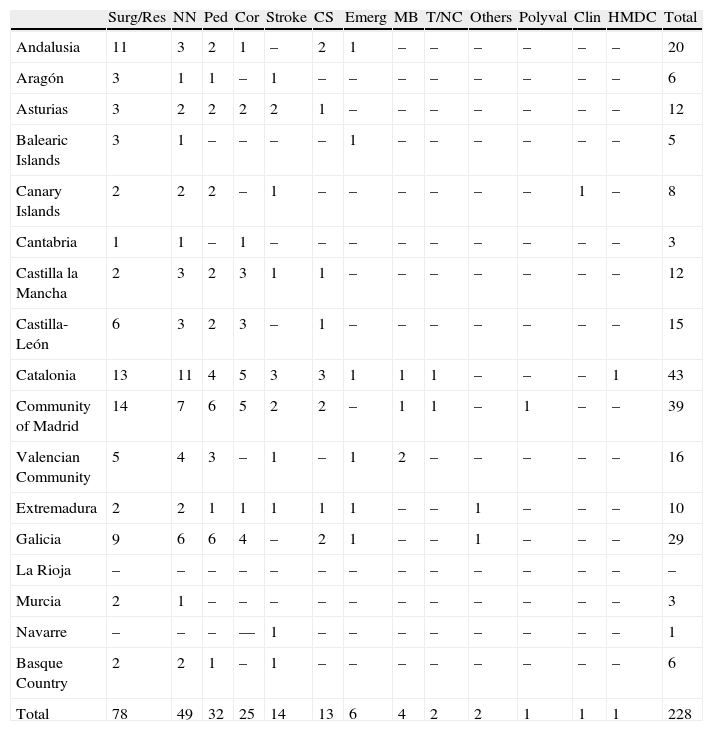
The Units attending critical patients and which are dependent upon other Departments or specialties (i.e., not dependent upon the DICM) are shown in Table 5, where the type and number of these Units are reflected, along with their distribution according to Autonomous Communities. The total number of Units analyzed was 228–the most numerous being Surgical/Postoperative Resuscitation Units (n=78, 34.2%), followed by Neonatal Units (n=49, 21.4%), Pediatric ICUs (n=32, 14%), Coronary Units (n=25, 10.9%) and Stroke Units (n=14, 6.1%).
Units not dependent upon the Departments of Intensive Care Medicine. Number and type of care area according to Autonomous Community.
| Surg/Res | NN | Ped | Cor | Stroke | CS | Emerg | MB | T/NC | Others | Polyval | Clin | HMDC | Total | |
| Andalusia | 11 | 3 | 2 | 1 | – | 2 | 1 | – | – | – | – | – | – | 20 |
| Aragón | 3 | 1 | 1 | – | 1 | – | – | – | – | – | – | – | – | 6 |
| Asturias | 3 | 2 | 2 | 2 | 2 | 1 | – | – | – | – | – | – | – | 12 |
| Balearic Islands | 3 | 1 | – | – | – | – | 1 | – | – | – | – | – | – | 5 |
| Canary Islands | 2 | 2 | 2 | – | 1 | – | – | – | – | – | – | 1 | – | 8 |
| Cantabria | 1 | 1 | – | 1 | – | – | – | – | – | – | – | – | – | 3 |
| Castilla la Mancha | 2 | 3 | 2 | 3 | 1 | 1 | – | – | – | – | – | – | – | 12 |
| Castilla-León | 6 | 3 | 2 | 3 | – | 1 | – | – | – | – | – | – | – | 15 |
| Catalonia | 13 | 11 | 4 | 5 | 3 | 3 | 1 | 1 | 1 | – | – | – | 1 | 43 |
| Community of Madrid | 14 | 7 | 6 | 5 | 2 | 2 | – | 1 | 1 | – | 1 | – | – | 39 |
| Valencian Community | 5 | 4 | 3 | – | 1 | – | 1 | 2 | – | – | – | – | – | 16 |
| Extremadura | 2 | 2 | 1 | 1 | 1 | 1 | 1 | – | – | 1 | – | – | – | 10 |
| Galicia | 9 | 6 | 6 | 4 | – | 2 | 1 | – | – | 1 | – | – | – | 29 |
| La Rioja | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Murcia | 2 | 1 | – | – | – | – | – | – | – | – | – | – | – | 3 |
| Navarre | – | – | – | –– | 1 | – | – | – | – | – | – | – | – | 1 |
| Basque Country | 2 | 2 | 1 | – | 1 | – | – | – | – | – | – | – | – | 6 |
| Total | 78 | 49 | 32 | 25 | 14 | 13 | 6 | 4 | 2 | 2 | 1 | 1 | 1 | 228 |
CS: cardiac surgery; Cor: coronary; MB: major burns; HMDC: hemodynamics; Clin: clinical; NN: neonatology; Ped: pediatric; Polyval: polyvalent (clinical/surgical/coronary); Surg/Res: surgical/resuscitation; T/NC: trauma/neurocritical; Emerg: emergencies.
Table 6 describes the number of beds of these CCUs not dependent upon the DICM. The total number of beds was 2233, with a clear predominance of postoperative beds (n=907), followed by Neonatology Units (n=507), Pediatric ICUs (n=265), Coronary Units (n=201), and Cardiac Surgery Units (n=117). The Communities of Madrid, Catalonia, Galicia and Valencia were the four leading regions regarding the number of CCUs and operative beds. The Surgical/Resuscitation Units were mainly located in the Autonomous Communities of Madrid, Galicia, Andalusia and Catalonia, while the Coronary Units were found to be grouped in the Communities of Catalonia, Madrid, Galicia, Castilla-León and Castilla la Mancha.
Units not dependent upon the Departments of Intensive Care Medicine. Number of beds according to type of care area.
| Surg/Rea | NN | Ped | Cor | CS | Stroke | Emerg | MB | T/NC | Polyval | Clin | HMDC | Others | Total | |
| Andalusia | 108 | 26 | 16 | 14 | 17 | – | 6 | – | – | – | – | – | – | 187 |
| Aragón | 32 | 14 | 6 | – | – | 6 | – | – | – | – | – | – | – | 58 |
| Asturias | 66 | 24 | 14 | 15 | 16 | 12 | – | – | – | – | – | – | – | 147 |
| Balearic Islands | 18 | 9 | – | – | – | – | 4 | – | – | – | – | – | – | 31 |
| Canary Islands | 16 | 14 | 12 | – | – | 4 | – | – | – | – | 4 | – | – | 50 |
| Cantabria | – | 6 | 6 | 6 | – | – | – | – | – | – | – | – | – | 18 |
| Castilla la Mancha | 10 | 17 | 10 | 18 | 8 | 3 | – | – | – | – | – | – | – | 66 |
| Castilla-León | 67 | 25 | 12 | 29 | 6 | – | – | – | – | – | – | – | – | 139 |
| Catalonia | 107 | 129 | 25 | 42 | 28 | 16 | – | 8 | 10 | – | – | 4 | – | 369 |
| Community of Madrid | 158 | 76 | 70 | 35 | 18 | 12 | 6 | 8 | 8 | – | – | – | 391 | |
| Valencian Community | 94 | 26 | 35 | – | – | 4 | 19 | 12 | – | – | – | – | – | 190 |
| Extremadura | 16 | 16 | 7 | 8 | 4 | 4 | 14 | – | – | – | – | – | 8 | 77 |
| Galicia | 150 | 68 | 42 | 34 | 20 | 5 | – | – | – | – | – | 47 | 366 | |
| La Rioja | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Murcia | 22 | 3 | – | – | – | – | – | – | – | – | – | – | – | 25 |
| Navarre | – | – | – | – | – | 3 | – | – | – | – | – | – | – | 3 |
| Basque Country | 43 | 54 | 10 | – | – | 4 | 5 | – | – | – | – | – | 116 | |
| Total | 907 | 507 | 265 | 201 | 117 | 68 | 48 | 31 | 18 | 8 | 4 | 4 | 55 | 2233 |
CS: cardiac surgery; Cor: coronary; MB: major burns; HMDC: hemodynamics. Clin: clinical; NN: neonatology; Ped: pediatric; Polyval: polyvalent (clinical/surgical/coronary); Surg/Rea: surgical/resuscitation; T/NC: trauma/neurocritical; Emerg: emergencies.
On excluding the neonatology and pediatric beds, and the Stroke Units, the number of adult critical patient beds dependent or not upon the DICM was seen to be 3345 and 1393, respectively, representing 71%, of the adult critical patient beds registered.
DiscussionBased on different information sources, we have been able to update the SEMICYUC databases referred to the DICMs of the 237 hospitals of different levels and categories in Spain that answered the questionnaire–this figure representing a response rate of 83%.
In recent years there has been a growing demand for critical patient care. The planning and management of the critical care sector, which is associated to very important resource consumption, has therefore become a challenge for the healthcare systems.
The increased need of beds for patients of this kind is due to a number of factors, including progressive aging of the population, with increased comorbidities, and particularly increased expectations as to what Intensive Care Medicine is able to offer.5 Furthermore, exceptional situations over the years6 and also recently in the form of the influenza A pandemic, have generated alarm among the health authorities, which have suddenly come to question the capacity of the existing resources to respond to an unexpected increase in demand.7
On the other hand, countries such as the United States8 and Norway9 have already evidenced the difficulty of covering this generalized increase in demand–which is expected to grow even more in the coming years–and the impossibility of offering quality standard care by intensivists for all critical patients.10
Some authors have underscored the implications of the availability of either too many or too few critical care beds, assessing the risk-benefit impact for both patients and for society in extreme resource situations. In this sense, comparisons have been made with the Starling curve, though this issue remains the subject of debate.11
There is a clear need for precise knowledge of the existing resources for critical patient care, and for reliable and dynamic data with the purpose of seeking solutions allowing effective, safe and efficient resources adjustment to the current and future needs.
This study has attempted to address the above issue in the concrete case of Spain, based on the registry and analysis of certain structural aspects, with the purpose of knowing the current number of DICMs and ICUs, the type of Units and the number of available beds, and of other hospital Departments and specialties that attend critical patients without functional dependence upon the DICMs.
Few studies have been made on the identification of resources for critical patient care, and many of the existing publications offer incomplete and sometimes inconsistent results. The fact is that many countries lack complete and reliable official information on the existing intensive care beds. Some countries such as the United Kingdom have a state registry, while in others such as Germany, the corresponding Scientific Societies manage such data.12
Another of the main limitations in analyzing the data is the broad heterogeneity of the definitions used by the different registries in defining the functional structures,13 as well as the existence of different organizational models referred to critical patient care, and which makes it even more difficult to obtain contrasted information.
In a multicenter study analyzing the variability of critical care in North America and Western Europe, Spain was seen to contribute 258 ICUs with 3628 beds, this representing 8.2 ICU beds per 100,000 inhabitants, and 2.5% of the global hospitalization beds.14
Although there are partial references to the availability of beds in different countries, until recently there had been no grouped and comparative data referred to the European setting. The study published by Rhodes et al.12 was designed to identify the number of critical care beds available, and the variability among different European countries. The study included ICU and intermediate care beds, and excluded beds in private centers and specific Units such as Coronary Units, Stroke Units and Dialysis Units. The results indicated the existence of 73,585 critical care beds, representing 2.8% of all acute patient beds, with an average of 11.5 beds per 100,000 inhabitants. This contrasts significantly with the 28 beds per 100,000 inhabitants in the United States in the year 2010.15 There are large differences among countries, with a very high number of population-corrected critical care beds in Germany (29.2 beds/100,000 inhabitants) and a very low number in Portugal (4.2 beds/100,000 inhabitants) (i.e., 6.9 times more in one country than in the other). Spain ranks in an intermediate position, with 9.7 beds/100,000 inhabitants.
In our study, the number of identified critical care beds was 4738, excluding the geriatric and neonatal population, and Stroke Units. After adjusting for the Spanish population census of 1 April 2011 (46,148,605 inhabitants), this represents a total of 10.3 beds/100,000 inhabitants. These ascendant differences are probably explained by the exclusion of critical care beds in private centers and Coronary Units in the aforementioned European study, and in a sense validate the results of the registry of the SEMICYUC.
Different critical care models have been developed since the 1950s, when it became apparent that critical patient survival is improved when such individuals are treated in specific areas allowing monitorization and the adoption of supportive measures in cases of organ dysfunction. These constructs range from open models with the contribution of intensivists as consultants, to models such as that found in Spain, in which Intensive Care Medicine is a primary specialty, and the Units are staffed mainly by specialists in Intensive Care Medicine. While not without debate, there is sufficient scientific evidence that critical patient management by intensivists exerts a positive effect upon the results obtained.16 Some recent studies have demonstrated that the presence of an intensivist during the night shift in open organizational models reduces mortality.17 In addition, such a presence in closed Units could have an impact upon other intermediate outcome variables such as a reduction of adverse events, the duration of mechanical ventilation, and the stay in the ICU. These results in turn could have an impact upon the final outcomes, and could contribute to lessen the associated costs.18
Another issue that has been debated in relation to the organizational models refers to the care of critical patients in very specialized Units versus more polyvalent Units – recent studies having evidenced the benefits afforded by the latter.19 In our setting, the results of the registry show a clear predominance of polyvalent ICUs (78.5%) (clinical–surgical and coronary) in the case of Units dependent upon a DICM. In contrast, specialized Units represent a low percentage in the case of structures not dependent upon the DICM (particularly postoperative, coronary and cardiac surgery Units).
Among the 237 centers surveyed, the results obtained show the number of critical adult patient beds (excluding Stroke Units) to be 4738, of which 3345 depend upon the DICM, and the rest are distributed in variable number among different specialties. These data imply that 71% of the adult critical patient beds registered are dependent upon the DICM, in contrast to other previously reported statistics.20
ConclusionsReliable official registries are needed in order to allow a dynamic assessment of the resources available for critical patient care. In addition, consensus-based definitions are required in order to allow the comparison of clinical practice and the different organizational models.
The results of this study show that 71% of the beds available in Units that care for critically ill adult clinical–surgical patients are dependent upon the DICM, and that most such Units in turn are of a polyvalent nature.
Conflicts of interestAt the time of the survey, María Cruz Martín, Cristóbal León, José Cuñat and Frutos del Nogal were representing member of the Autonomous Community Societies, President, Vice-President and Vice-Secretary of the SEMICYUC, respectively.
Thanks are due to the administrative team of the SEMICYUC for its work and interest in this project.
Each registry refers to a Department of Intensive Care Medicine (DICM) of a hospital center. The registry is to be completed by the Director or Head of the DICM. The DICM can be composed of different structural units (ICU) or areas within the hospital, provided they are all supervised by the same Director or Head of Department. A hospital can have different DICMs (different managements) and other CCUs not forming part of the DICM as such.
What information is collected?
Data on the hospital: To be completed by SEMICYUC
- -
Name of the hospital
- -
Mailing address
- -
Province
- -
Autonomous Community
- -
Telephone
- -
Fax
- -
Website
Other column:
- -
Number of hospital beds:
- -
Level of the hospital: I, II, III
- -
Type: public, private, mixed
- -
University hospital: yes/no
Data on the DICM
- -
Name of the Head of Department
- -
Contact e-mail
- -
Telephone DICM
How many Units conform the DICM?:
- 1.
One
- 2.
Several: how many: number:
Please cite this article as: Martín MC, León C, Cuñat J, del Nogal F. Recursos estructurales de los Servicios de Medicina Intensiva en España. Med Intensiva. 2013;37:443–451.