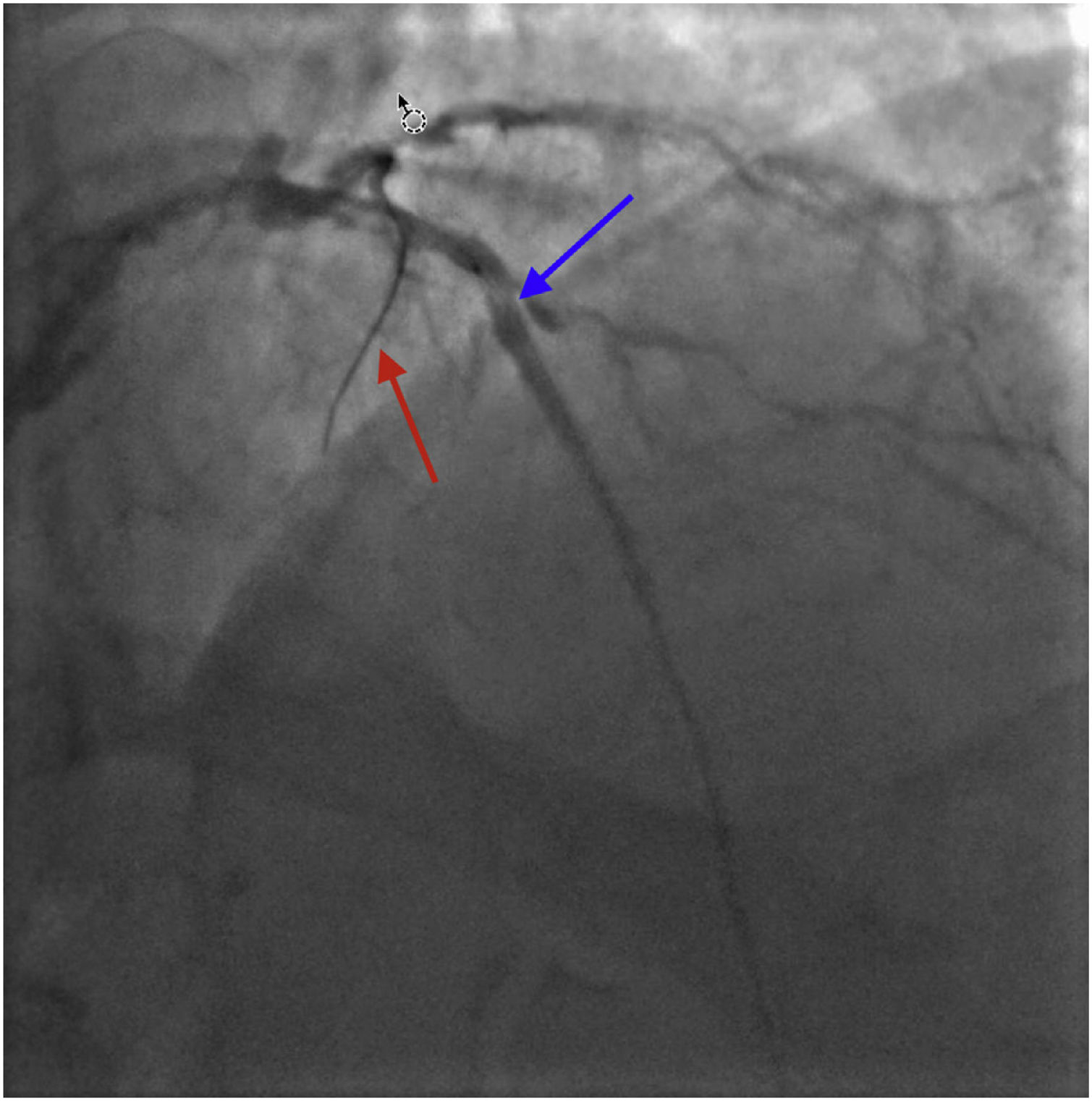
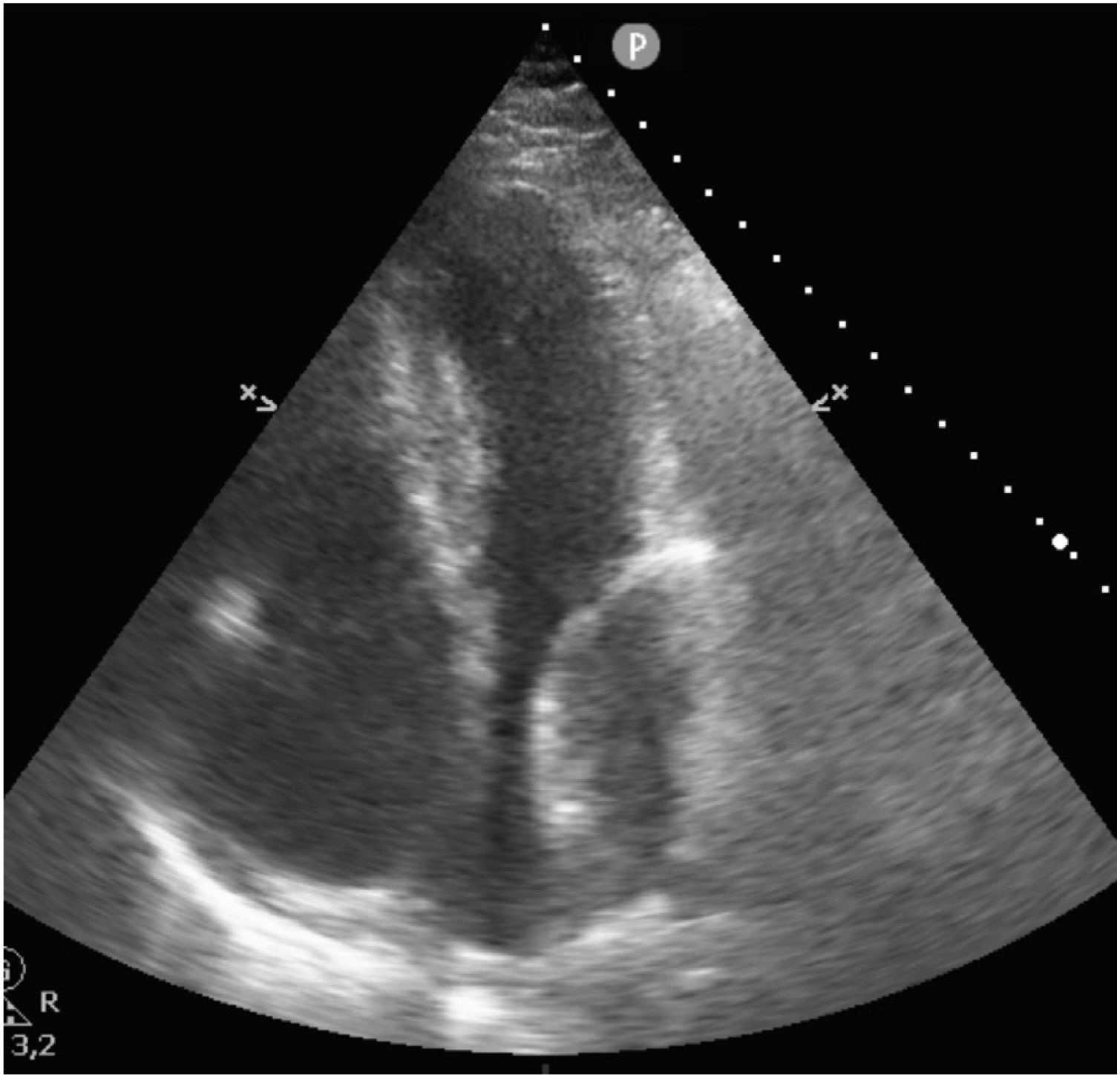
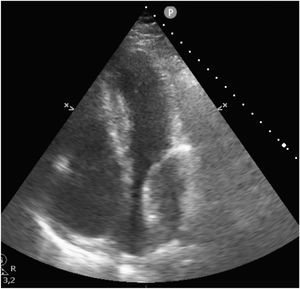
This is the case of an 80-year-old man with multiple cardiovascular risk factors admitted to the intensive care unit due to non-ST-segment elevation acute myocardial infarction. The coronary angiography performed reveals the presence of left main coronary artery and left anterior descending coronary artery disease. Revascularization is attempted through overlapping drug-eluting stent implantation (Fig. 1, blue arrow). Afterwards, the left circumflex artery is crossed with a guidewire (Fig. 1, red arrow). Procedure is uneventful. However, suddenly after the procedure the patient shows signs of heart failure. Transthoracic echocardiography confirms the presence of a 64mm×40mm mass—echolucent inside—with demarcated borders at left atrium lower level with a reduced size of such cavity compromising atrial filling consistent with left atrial wall hematoma (Fig. 2).
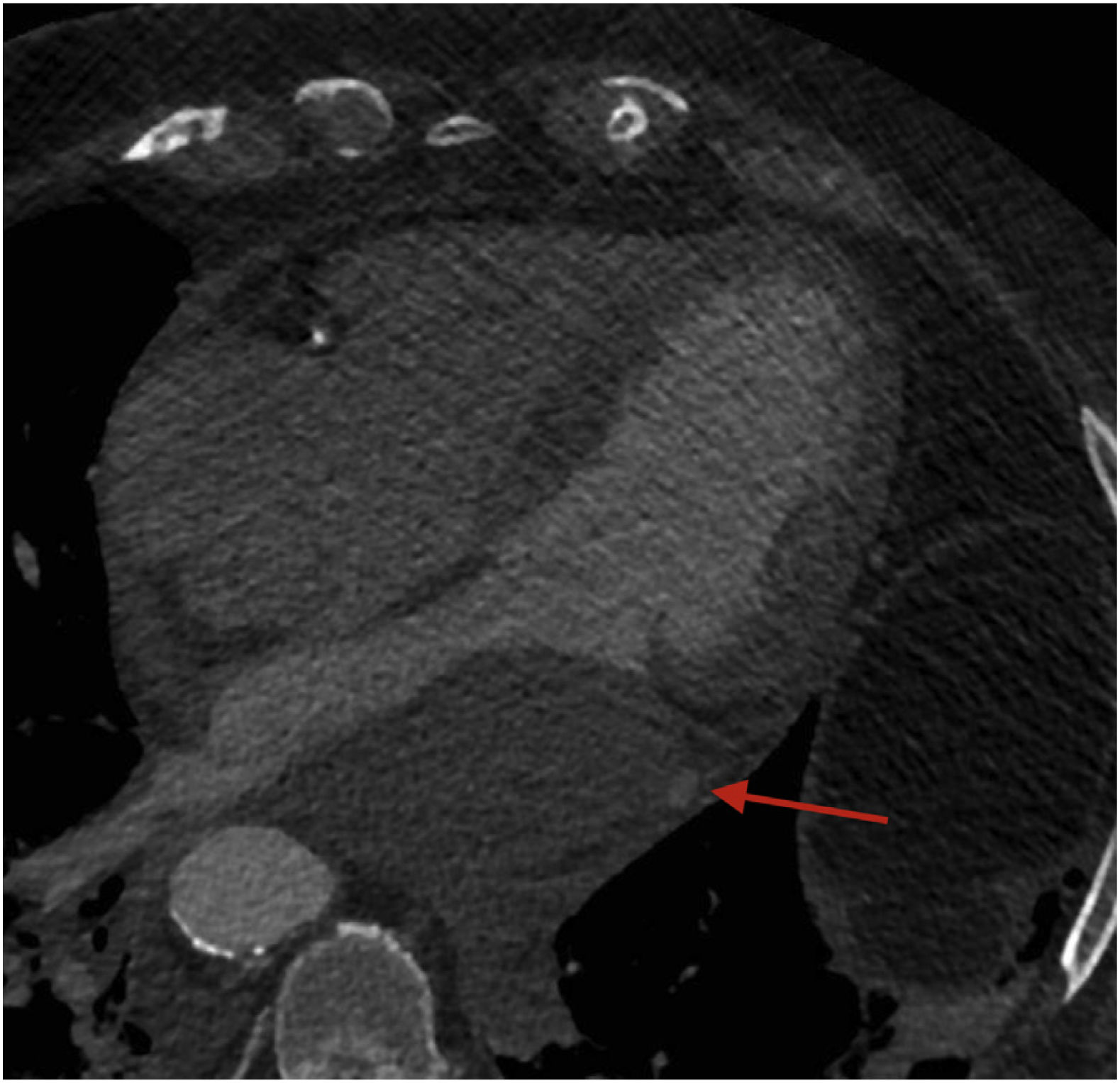
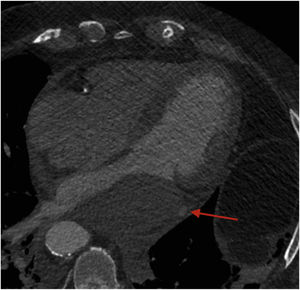
The coronary computed tomography angiography (CCTA) (Fig. 3) performed to complete the study confirms the presence of the hematoma and contrast material leak across the left circumflex artery possibly due to the perforation of the vessel during coronary angiography.
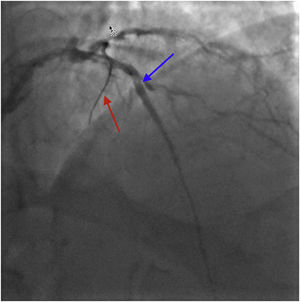
After optimal medical therapy is administered, the patient progressively stabilizes from both the clinical and hemodynamic standpoint. Two weeks later, a new follow-up coronary angiography is performed and confirms the proper condition of the stents previously implanted without any angiographic leaks at that time.