This is the case of a 27-yearl-old man admitted to the ICU in a state of coma following self-inflicted injury with insulin. Several insulin pens are found around him (1800 IU of fast-acting insulin, and 600 IU of glargine) plus an empty blister of diazepam. The patient’s GCS is 3, which is why orotracheal intubation is decided while the patient keeps his respiratory and hemodynamic stability.
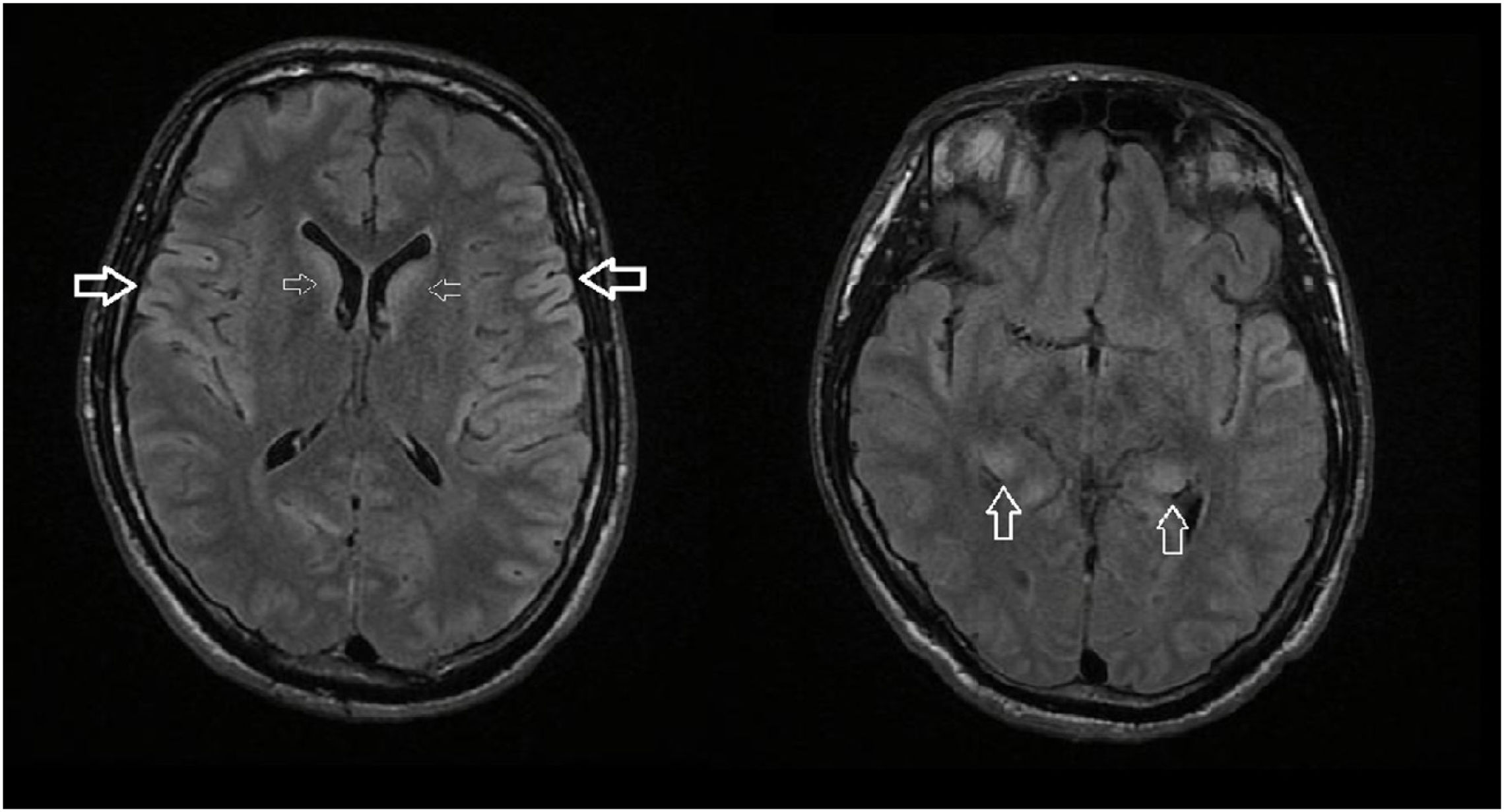
Within the first few days after admission, the patient presents with hard-to-control severe hypoglycemia while remains unresponsive to stimuli without confounding medication. Epileptiform activity is spotted on the EEG and then treated. The cerebral CT scan performed confirms the presence of brain swelling (Fig. 1).
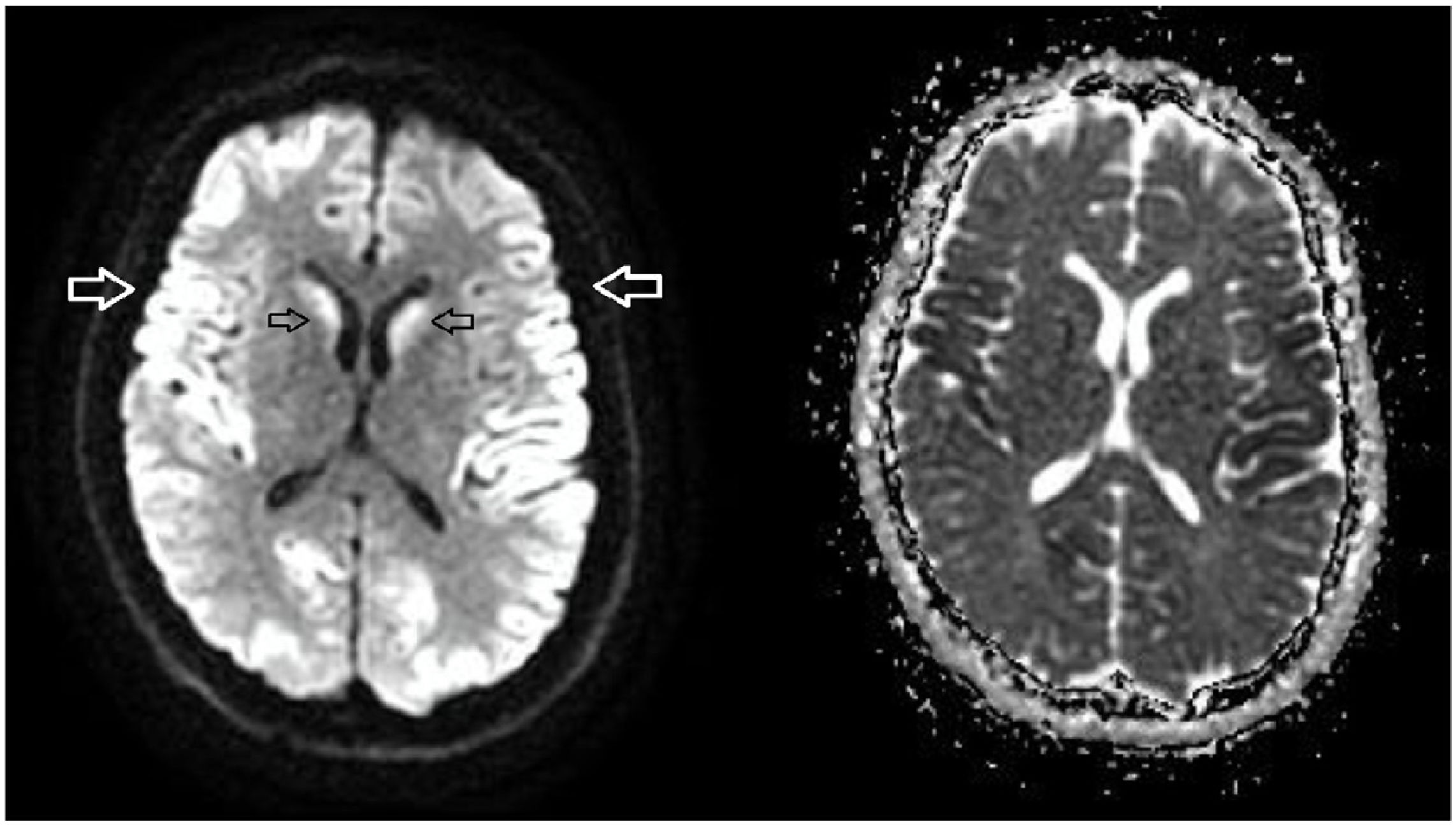
A cerebral MRI is performed following suspected hypoglycemic encephalopathy. The cerebral MRI shows findings that are specific to such condition such as hyperintensity in the symmetric and bilateral Flair sequence in the frontal and parietal cortex, and in both caudate nuclei and hypocampi (Fig. 2: the arrows point at the parietal cerebral cortex, the caudate nuclei, and both hippocampi), and diffuse restriction in such areas (Fig. 3; arrows point at the parietal cortex and caudate nuclei in the diffusion sequence showing diffusion restriction in the adjacent ADC map).