The care of pediatric critical patients is constantly evolving. Moreover, it presents fundamental and necessary differences compared to the care of adult critical patients. This creates a scenario in which a continuous review of the evidence is essential. Specialists dedicated to caring for critically ill children need solid, practical, and up-to-date literature.
Therefore, this series of "Update" articles will review six topics of interest regarding pediatric critically ill patients. Training, care, and ethical aspects will be addressed through a series of review articles written by experts. The working methodology is described below, along with a summary of the articles that will be published in this series.
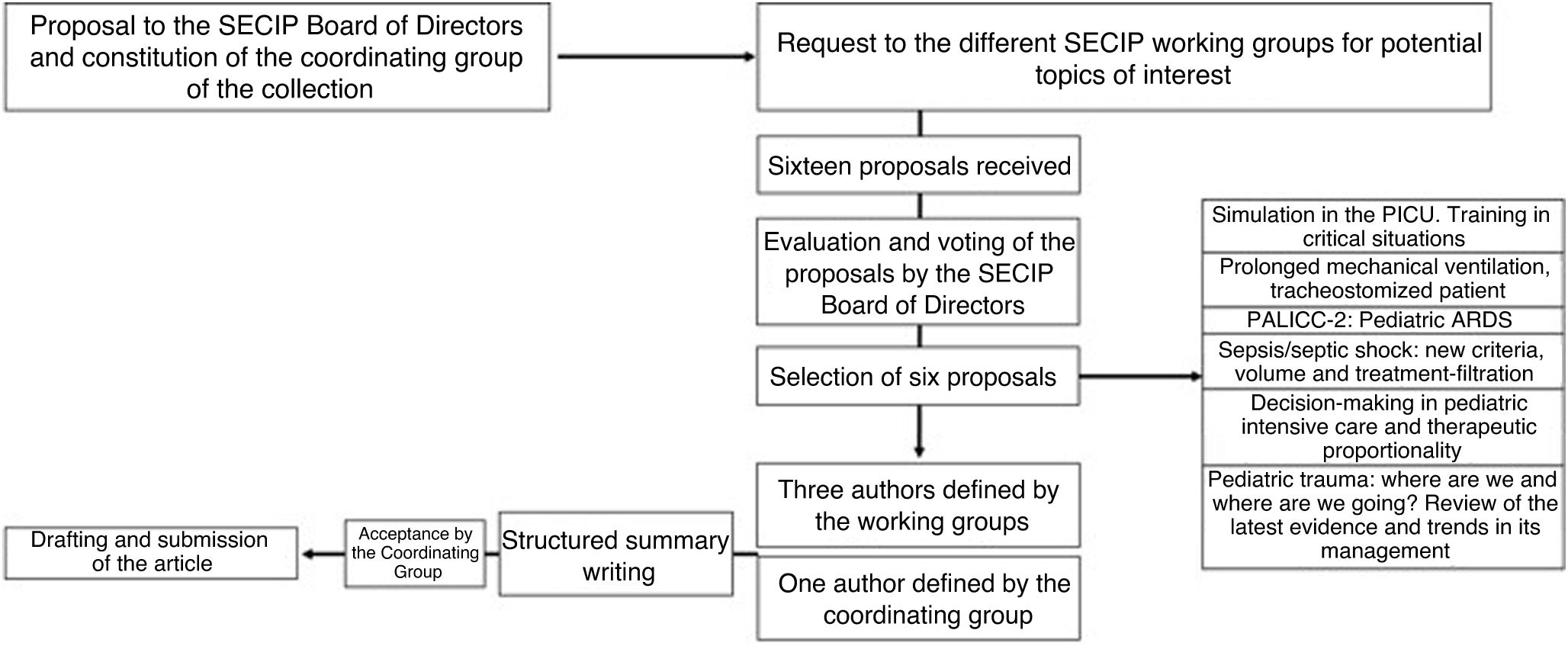
Working methodologyAfter the editorial board of Medicina Intensiva determined the relevance of the collection, a coordinating team was constituted. The team formalized a proposal to the Spanish Society of Pediatric Intensive Care (Sociedad Española de Cuidados Intensivos Pediátricos, SECIP). The SECIP requested suggestions for topics of interest to the different working groups. After submitting them to a vote, the SECIP Board of Directors selected six topics and authors were chosen to prioritize an interdisciplinary vision and the widest possible geographical representation.
Three of the authors for each article were chosen directly from the working groups. The SECIP Board of Directors designated the authorship if there were no candidates. Additionally, the group coordinating the collection proposed a fourth author whose main function would be to act as an internal reviewer of the manuscript during its drafting. The authors were also requested to provide a structured abstract of the article. Once the general structure was evaluated and accepted, the drafting process began for subsequent submission to the journal (Fig. 1).
Topics of the seriesSimulation in pediatric intensive careIntegrating medical simulation into clinical practice improves coordination and care while avoiding healthcare errors. Emergency and resuscitation contexts were among the first to use simulation in the healthcare settings. Barriers to its universalization include cost, its difficult integration into work schedules, and a lack of prior training.1 Despite these challenges, simulation is undoubtedly an essential tool for improving the quality of care for critically ill patients, regardless of their age or condition. In Spain, the SimuSECIP group has played a key role in developing and disseminating simulation techniques.2 This series will review the available evidence on the use of simulation in pediatric patients. Practical examples will also be presented to improve understanding of the current state of the art and to enhance its application in training and care.
Prolonged mechanical ventilationMedical advances, an increase in complex chronic diseases, and lower mortality rates have led to a rise in the number of patients requiring prolonged mechanical ventilation (MV).3 These patients require complex care resources for extended periods. Their management must be optimized, from the indication of tracheostomy and the ventilator weaning process, to respiratory, nutritional, and neurodevelopmental recovery.4 At the same time, the unnecessary prolongation of MV varies among Pediatric Intensive Care Units (PICUs) and is associated with more complications. This scenario poses economic and organizational challenges that require concrete policies. This article will review the current evidence on prolonged MV and its application in clinical practice.
SepsisSepsis poses a clinical challenge. To reduce mortality and morbidity, therapeutic guidelines have standardized its management, emphasizing the importance of early identification and the need for a rapid and, above all, effective clinical response.5
The article in this collection will review how these strategies have led to the individualized application of inotropic agents, a conservative approach to transfusions and expansion measures, and the early use of renal replacement techniques when indicated in pediatric patients.5,6 There will also be a focus on the rational use of antimicrobials with close monitoring of their pharmacokinetics.7 Finally, in the search for personalized care in the context of sepsis, the discussion will comment on how modulation of the inflammatory response and the detection of clinical and leukocyte phenotypes are currently fields of great research interest.5
Decision makingMaking decisions for critically ill children is challenging. It is essential to consider the patient's best interests, level of maturity, and values. These factors should align with the criteria, principles, and values of the parents, caregivers, and healthcare professionals. Therefore, it is crucial to develop skills that prevent bias, prejudice, misconceptions, and paternalism.8
As support for organic functions advances, it is necessary to constantly define proportionality according to reasonable objectives by establishing time-limited action plans and therapeutic efforts. It is crucial to define when a treatment is futile and should be withdrawn or not initiated, especially in cases involving complex, technology-dependent, or non-technology-dependent chronic pediatric patients. In these cases, quality of life and a focus on wellness are priority concerns. In cases of conflict or difficult decisions, consultation with the Healthcare Ethics Committee can provide expert support.8 This collection will review the ethical principles that should guide PICU care and resource management.
PALICC-2: pediatric acute respiratory distress syndromeOver the last 60 years, acute respiratory distress syndrome (ARDS) has been the subject of consensus conferences, definitions, research, and constant updates.9 In pediatric intensive care, the last 10 years have marked a paradigm shift. In effect, there has been a shift from relying on criteria developed by intensivists for adult patients to criteria designed by pediatric intensivists for the pediatric population. This progress materialized with the publication of the PALICC guidelines in 2015 and their update in 2023.10 The chapter dedicated to pediatric ARDS will delve into the new recommendations from a descriptive perspective, with a critical and objective view.
Pediatric traumaUpdating the management of pediatric polytraumatized patients is essential due to the appearance of new recommendations such as the XABCDE protocol, adaptations in cardiopulmonary resuscitation, damage control, and new transfusion guidelines.11 These strategies aim to optimize care and improve outcomes for critically injured children. However, the evidence in adults is not always applicable to children due to differences in physiology and injury response.12 Unquestioningly, adapting protocols designed for adults may compromise the safety and effectiveness of treatment for pediatric patients. This article of the collection will review the relevance of these trends to identify evidence-based medical decisions appropriate for the pediatric population.
ConclusionsFor the above mentioned reasons, the group coordinating this collection hopes that it will be both enjoyable and practical. We believe that focusing on the care of critically ill children is a fair and even mandatory exercise. Since "children are not small adults", it is reasonable to conclude that their intensive care is far from being a diminutive adaptation of how their elders are treated.
CRediT authorship contribution statementAGS drafted the text, wrote sections, designed the layout, adapted the document to the editorial standards, contributed and added the bibliography, and reviewed the final document. YLF, AMV and MJSL participated in the drafting of the text, contributed to the bibliography, and corrected and reviewed the final document.
Declaration of Generative AI and AI-assisted technologies in the writing processArtificial intelligence was not used.
Financial supportNo funding was received.
The authors have no conflicts of interest.