The incidence of traumatic laryngeal injury in the United States is 1 case for every 30000 patients.1 Closed laryngeal injury (CLI) is rare, its prognosis is worse than penetrating trauma, and its mortality rate is up to 40%.2 This prognosis is related to the management of the airway (AW) whose prehospital mortality is up to 80%3 and to associated injuries.
In our ICU we provided care to 1363 patients from 2012 through 2016 and 6 of these patients showed CLI of extrinsic origin. The general characteristics, physical examination, management of the AW, radiologic findings, and treatment are shown in Table 1.
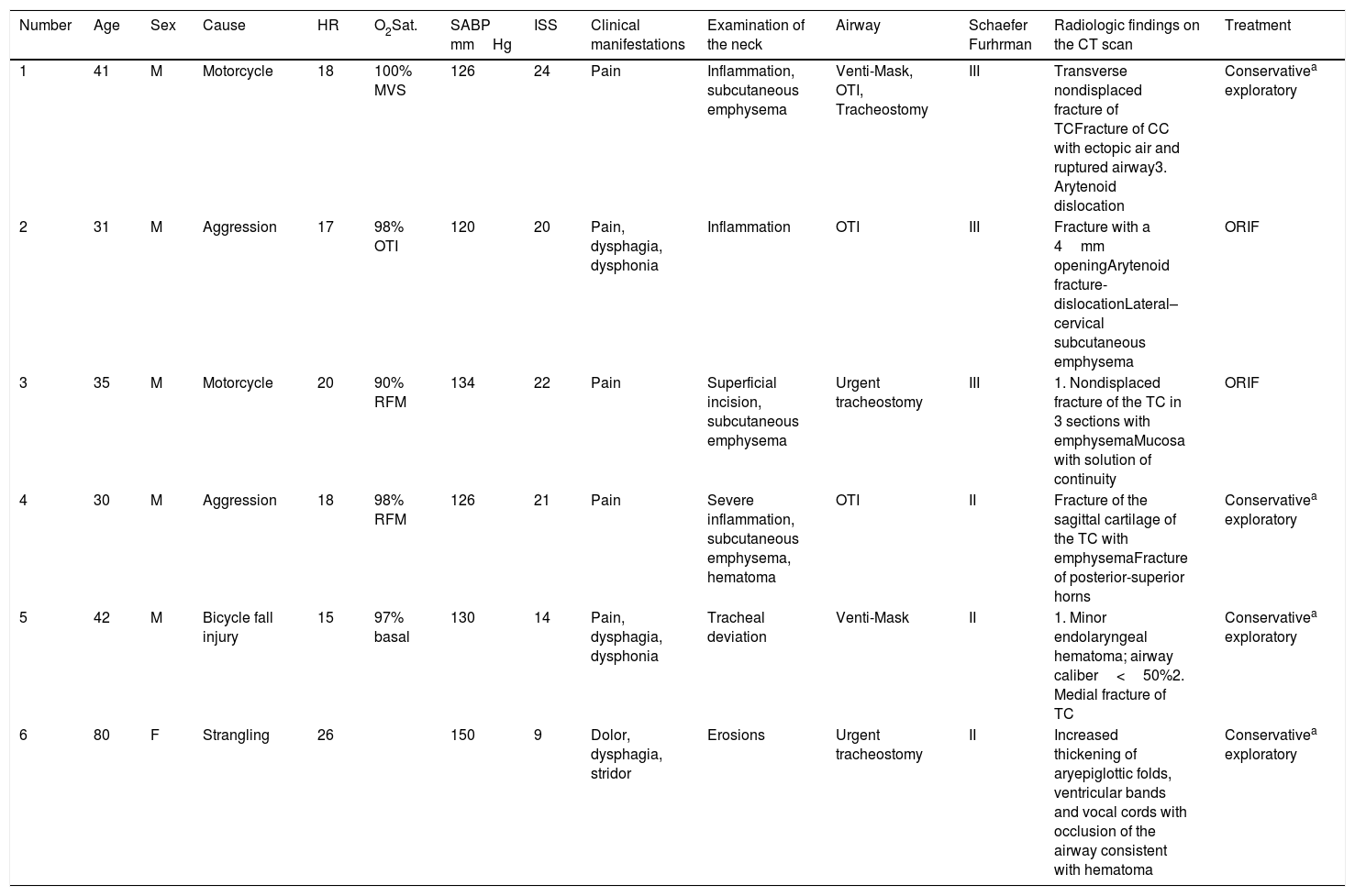
Characteristics and lesions of the patients: clinical management.
| Number | Age | Sex | Cause | HR | O2Sat. | SABP mmHg | ISS | Clinical manifestations | Examination of the neck | Airway | Schaefer Furhrman | Radiologic findings on the CT scan | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 41 | M | Motorcycle | 18 | 100% MVS | 126 | 24 | Pain | Inflammation, subcutaneous emphysema | Venti-Mask, OTI, Tracheostomy | III | Transverse nondisplaced fracture of TCFracture of CC with ectopic air and ruptured airway3. Arytenoid dislocation | Conservativea exploratory |
| 2 | 31 | M | Aggression | 17 | 98% OTI | 120 | 20 | Pain, dysphagia, dysphonia | Inflammation | OTI | III | Fracture with a 4mm openingArytenoid fracture-dislocationLateral–cervical subcutaneous emphysema | ORIF |
| 3 | 35 | M | Motorcycle | 20 | 90% RFM | 134 | 22 | Pain | Superficial incision, subcutaneous emphysema | Urgent tracheostomy | III | 1. Nondisplaced fracture of the TC in 3 sections with emphysemaMucosa with solution of continuity | ORIF |
| 4 | 30 | M | Aggression | 18 | 98% RFM | 126 | 21 | Pain | Severe inflammation, subcutaneous emphysema, hematoma | OTI | II | Fracture of the sagittal cartilage of the TC with emphysemaFracture of posterior-superior horns | Conservativea exploratory |
| 5 | 42 | M | Bicycle fall injury | 15 | 97% basal | 130 | 14 | Pain, dysphagia, dysphonia | Tracheal deviation | Venti-Mask | II | 1. Minor endolaryngeal hematoma; airway caliber<50%2. Medial fracture of TC | Conservativea exploratory |
| 6 | 80 | F | Strangling | 26 | 150 | 9 | Dolor, dysphagia, stridor | Erosions | Urgent tracheostomy | II | Increased thickening of aryepiglottic folds, ventricular bands and vocal cords with occlusion of the airway consistent with hematoma | Conservativea exploratory |
Bed rest, humidification, Anti-H2, and corticoids.
CC, cricoid cartilage; F, female; HR, heart rate; ISS, injury severity score; M, male; O2Sat.: oxygen saturation with oxygen delivery; ORIF, open reduction and internal fixation; OTI, orotracheal intubation; RFM, reservoir facial mask; SABP, systolic arterial blood pressure; T, trauma; TBI, traumatic brain injury; TC, thyroid cartilage; VMask, Venti-Mask at 40%.
Motorcycle accident. Patient transferred with Venti-Mask, with rigid Philadelphia cervical collar (PCC) and lateral cervical immobilizer with neck pain and subcutaneous emphysema, patent airway (PAW) and hemodynamic stability (HS). During the radiologic study, the patient developed dyspnea with decreased oxygen saturation that required orotracheal intubation (OTI) using the FROVA® intubating introducer with Cormack-Lehane grade iii. The study confirmed the presence of one transverse fracture without displacement of thyroid cartilage (TC) and cricoid cartilage (CC). It was decided to perform a surgical tracheostomy procedure.
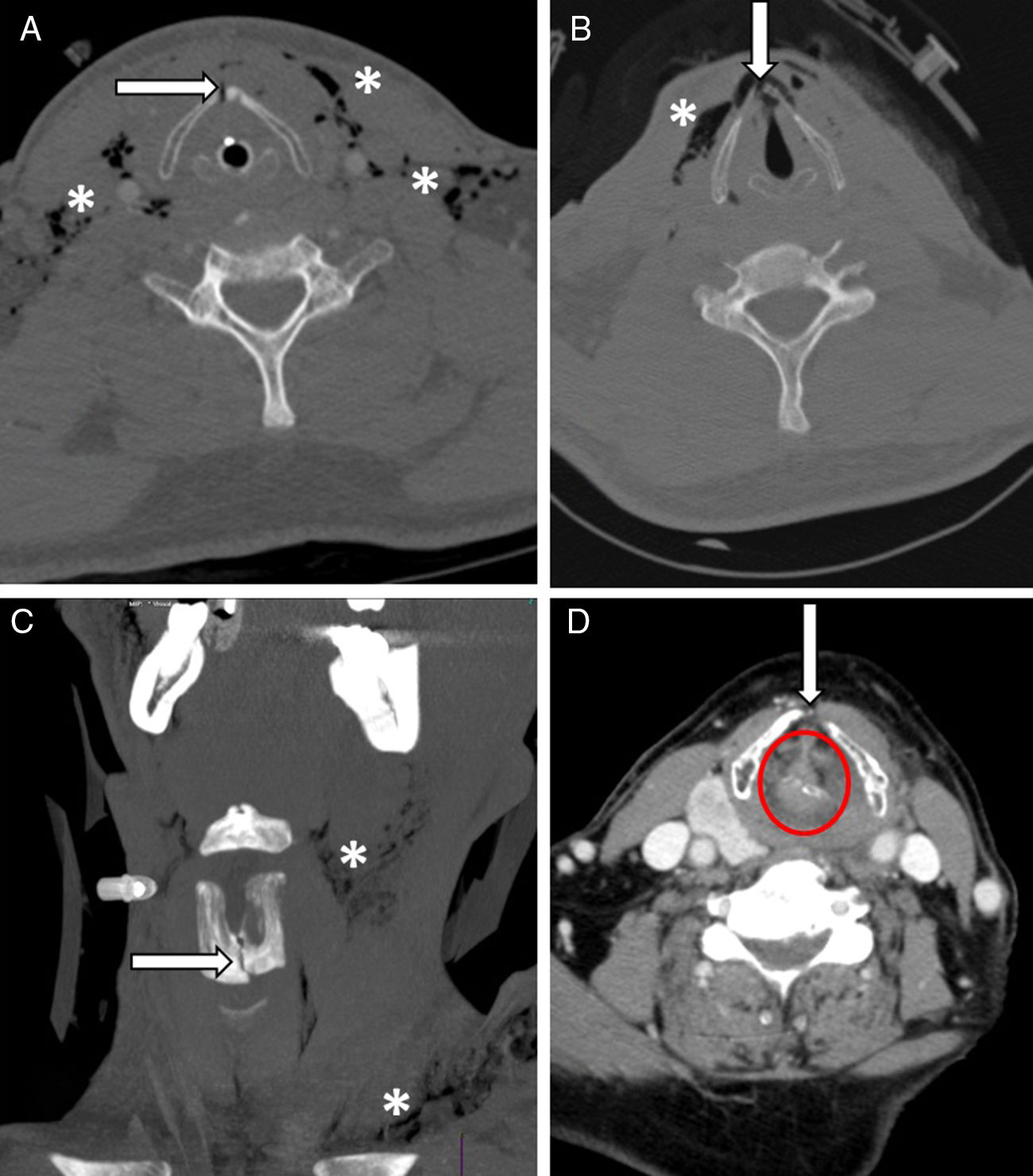
Case #2Patient transferred from a different hospital after being involved in a fight and complaining of pain, dysphagia and dysphonia, but PAW. The computed tomography scan confirmed the fracture of the TC with a 4mm separation between the fragments and fracture-luxation of the arytenoid cartilage (Fig. 1). Since surgery was not an option in this center, one OTI was performed and the patient was transferred to our hospital (where another CT scan was performed due to lost images that confirmed the aforementioned findings) wearing a PCC stabilizer. The ear, nose and throat (ENT) unit of our hospital was contacted, and they performed open reduction and internal fixation (ORIF) surgery.
(A) Case #2. Fracture of thyroid cartilage with a 4mm opening (arrow) and subcutaneous emphysema (asterisk). (B) Case #3: nondisplaced fracture of the thyroid cartilage with solution of continuity (arrow) and subcutaneous emphysema (asterisk). (C) Case #4: sagittal fracture of the thyroid cartilage with solution of continuity (arrow) and cervical emphysema (asterisk). (D) Case #6: hematoma and edema with occlusion of the airway (arrow).
Motorcycle accident. Patient transferred with reservoir facial mask and PCC. The patient was in pain and showed 2 incised and lacerated wounds in the anterior region of the neck with spontaneous air leak and significant subcutaneous emphysema. The chest X-ray performed confirmed the presence of one pneumothorax that started with HS but showed progressive dyspnea that required chest drain in situ. The CT scan showed 3 lines of fractures in the TC and solution of continuity of the mucosa (Fig. 1B). The patient was transferred with PAW straight to the operating room where tracheostomy and ORIF procedures were performed.
Case #4Physical aggression transferred with reservoir facial mask. The patient showed facial edema and cervical emphysema and complained of pain and dysphonia. Since the AW was compromised, it was decided to proceed with an urgent OTI with Airtraq® using the FROVA® intubating introducer with Cormack-Lehane grade iv. The CT scan confirmed the presence of one sagittal fracture of the TC, cervical emphysema, and pneumomediastinum in continuity (Fig. 1C). The ENT unit was consulted, and conservative treatment was recommended.
Case #5Bicycle fall injury. The patient complained of dysphagia, dysphonia and cervical pain. Patient transferred on Venti-Mask and lateral cervical immobilization. Tracheal deviation and inflammation at tracheal level was confirmed so PPC immobilization was decided. With PAW, the CT scan confirmed the presence of one nondisplaced fracture of the left TC. The ENT unit performed one endoscopy using a flexible fiberscope that revealed the presence of one pharyngeal hematoma and cortical integrity at the TC fissure level, which is why it was decided to proceed with conservative treatment.
Case #6Attempted strangulation that led to loss of consciousness and sphincter relaxation, which is why the patient went back to the hospital after recovery. The patient complained of cervical pain, dysphonia and laryngeal stridor. After being examined at the ER, the patient was administered hydrocortisone and then transferred with Venti-Mask at 40% for a CT scan that confirmed the hematoma-induced AW collapse and the presence of swelling (Fig. 1D) and tachypnea after the study, which is why we were called to act. Since the OTI was difficult, the operating room was notified to perform one tracheostomy procedure.
The incidence of CLI was 0.4% of our admissions. Pain and dysphonia were the most common symptoms of all, while subcutaneous emphysemas and soft tissue enlargements were the most characteristic signs. Although they are usually the most common signs of all,4 they may be absent during the first medical examination, and even the coexistence of other associated wounds, such as the presence of pneumothorax, can mask and delay diagnosis with the corresponding prognostic consequences.5 Five (5) out of the 6 patients had other traumas being the maxillofacial trauma the most common of all and consistent with the cases described by medical literature.6
The management of the AW is a priority in these patients, being the transfer to the closest center available a priority in the case of an emergency for the management of the AW. The way to do this is still controversial, however, we should distinguish between the existence or not of respiratory compromise. However, in life-threatening situations there is no clear-cut recommendation on the management of the AW. In our own experience, we used the protocol for the management of difficult airway established for OTI procedures, and only proceeded with the surgical AW when the implementation of the former protocol was not possible and the patient could not be ventilated manually.7 We should remember here that both techniques, or ventilation, can aggravate the wounds and require the immediate replacement or isolation of the AW through surgical tracheostomy8 or this procedure should be the primary urgent AW isolation technique as it was the case with 50% of our patients.
After securing the patency of the AW, cervical management and HS, the patient should be transferred for radiologic study purposes with a CT scan. All wounds were categorized as stage ii and iii; in these wounds, the TC fracture was found in 83.3% of the patients, well above the 37% recorded by Becker et al.9 However, the presence of small hematomas or minimum solutions of continuity of the laryngeal mucosa can be difficult to see on a radiologic study, thereby underestimating the actual incidence of CLI.
The definitive treatment of the wounds should be guided following Schaefer-Fuhrman classification. Cases #2 and #3 required urgent ORIF surgery, since the early surgical management of patients with a surgical indication has proven to bring beneficial effects to these patients’ clinical progression, which makes it is the most importance aspect of the care provided at a capable center.10
With our series of cases we wanted to conclude that CLI is an uncommon entity where clinical suspicion, the optimal early management of the airway, and multidisciplinary care in a capable center may impact positively the prognosis of patients.
Please cite this article as: Viejo-Moreno R, García-Fuentes C, Mudarra-Reche C, Terceros-Almanza LJ, Chico-Fernández M. Lesión laríngea en el traumatismo cervical cerrado. Med Intensiva. 2019;43:503–507.