Estimating the height of a person while standing up is considered the gold standard. However, due to the special characteristics of critically ill patients, this method cannot be used. The common practice followed by the Spanish intensive care units (ICU) is visual estimation even though it has proven inaccurate,1,2 and far from the clinical recommendations made.
Other methods used through indirect measurements like long bone measurement—ulna length or arm span—are closer to the standard of reference that is the visual method or the measuring tape.3–6 However, these are difficult to implement due to immobilizations, the presence of medical devices or swelling.
One of the main utilities of height in critically ill patients is to estimate the patient’s ideal weight so it can be applied to the tidal volume (TV) calculation. Protective ventilation reduces the number of infections, mortality, days on mechanical ventilation, and is associated with less pulmonary damage, and a slower progression of the acute respiratory distress syndrome (ARDS).7–9 Inaccurate height measurements can, therefore, be a source of error regarding the implementation of this ventilatory strategy.
This paper exposes the concordance of 2 methods (visual and laser-based) with the gold standard (height measuring device) to obtain the height of critically ill patients. Also, it illustrates its potential implication by estimating the patient’s ideal weight and TV.
Using the convenience sampling method, a series of patients admitted to the critical care unit with a diagnosis of myocardial infarction (Killip I) were included from October 2018 through July 2019 since this type of patient facilitates height measurement in bipedalism in the same ICU within the first 24/48 hours after admission.
After signing the written informed consent, the patient’s treating nurse was asked to conduct a visual estimation of the patient’s height in the supine position. Afterwards, a member from the research team used the Bosch® Zamo laser distance measuring tool with a reach of up to de 0.15 m to 20 m, and a ± 3 mm accuracy. Measurement was performed with the patient in the supine position while his head rested in the Frankfurt horizontal plane (eye socket and auditory meatus in the same horizontal plane), upper extremities attached to both sides of the trunk, no pillow while the measuring tool pointed to the patient’s head. The end of the bed was used as the limit so that the patient’s soles could touch the end of the bed. Then, a different member from the team who was blinded to the results previously reported established the patient’s height using Seca® height measuring system (bodymeter 206)—built in Germany—with a measuring range from 0 cm to 220 cm and an accuracy of ± 5 mm. The patient was placed in bipedalism, barefoot with both heels together, body position on a steady-state, arms and shoulders relaxed, and head in the Frankfurt horizontal plane.
The patient’s ideal weight (IW) was estimated using the following formula:10
- •
Ideal weight (males) = 50 kg + [0.91 × height in cm − 152.4 cm]
- •
Ideal weight (women) = 45.5 kg + [0.91 × height in cm − 152.4 cm]
Once the IW was known, the TV was estimated at a rate of 6 mL per kg of ideal weight.
Differences > 10% of the TV between methods were considered significant differences.
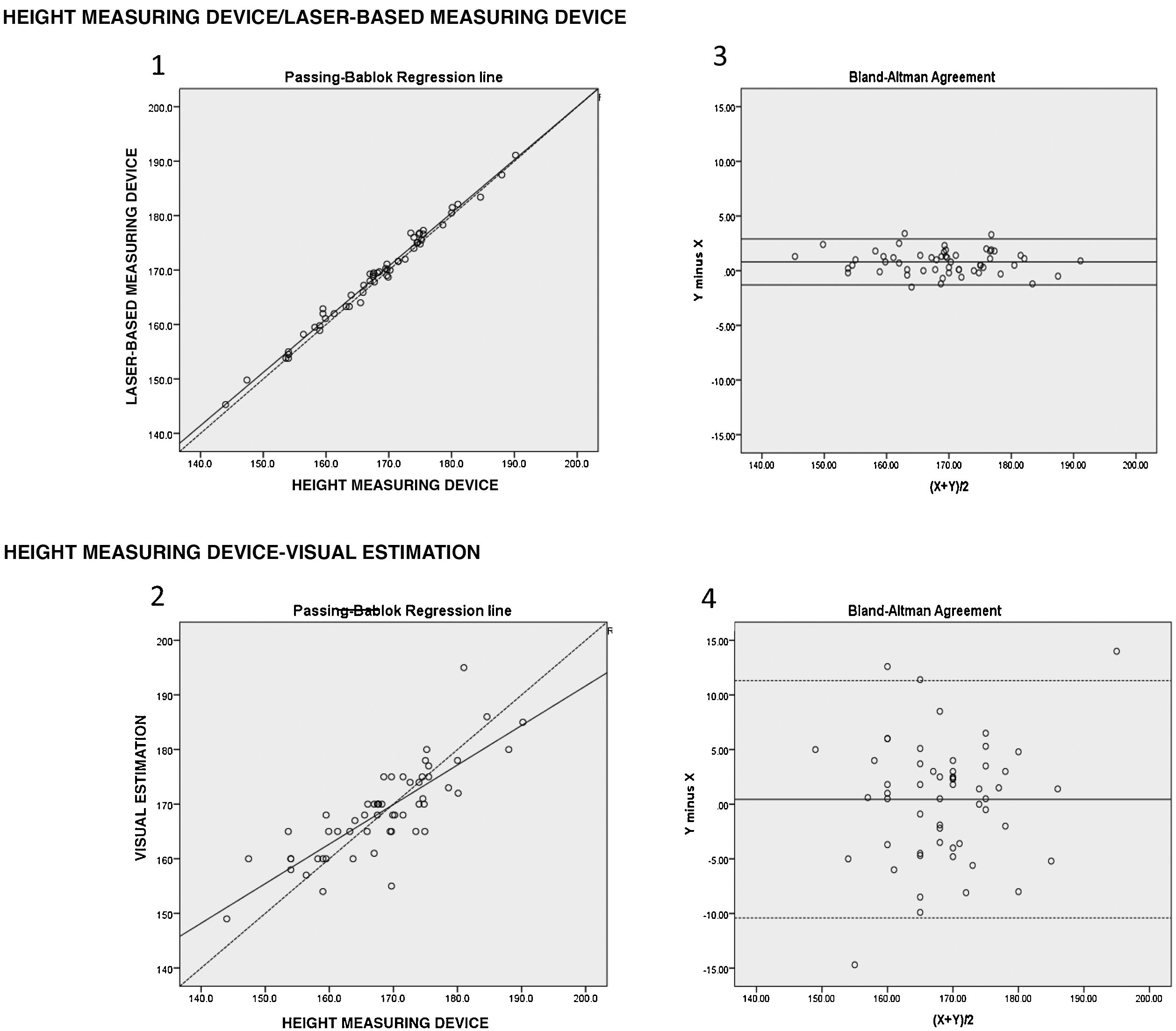
Regarding the concordance analysis and its graphic representation, the Passing-Bablok method and the Bland-Altman method were used.
Since errors were found while trying to determine the patient’s height–whether by excess or default–, that is, differences in both ways with respect to the mean, the results were expressed in absolute values to explain dispersion with more clarity.
A total of 55 patients were recruited—85.5% males—with a mean age of 62.7 years (SD = 11.9), and an average stay of 3.7 days (SD = 2).
Regarding height measurement, a mean difference was found between the height measuring device and the laser of 1 cm (SD = 0.8). Also, between the height measuring device and the visual method of 4.3 cm (SD = 3.4), P < .001. Fig. 1 shows the concordance charts. Laser-based measurements revealed a nearly perfect concordance with the height measuring device (chart 1). Discrepancies were seen between the values obtained with the height measuring device and those estimated by the nurse that were greater in the extreme values of both ends (chart 2). Due to the bias reported, patients were divided into 2 subgroups based on a median of height of 168 cm. Thanks to this subdivision, it was reported that patients with heights > 168 cm were measured 2 cm (P25 = 1.7-P75 = 5) shorter compared to their actual height while patients with heights ≤ 168 cm were measured 2.5 cm (P25 = 0.6-P75 = 5) taller compared to their actual height. Bias was reported between the height measuring device and the laser of 0.8 cm (95%CI, −1.3 to 2.9). Also, between the height measuring device and the visual method of 0.4 cm (95%CI, −10.4 to 11.3). However, this last bias with a much higher concordance range that involved less accuracy in the visual method (charts 3 and 4).
Regarding the measurement of the IW, the greater discrepancy found between the laser and the height measuring device was 6% (equivalent to 3 kg). In the visual estimation, 11 patients (20%) showed weight differences > 10% equivalent to 5 kg to 13 kg.
Finally, after checking the TV estimated using the height obtained with the laser-based measuring device compared to the height obtained with the height measuring device, the greatest difference was 5%, which would have been equalent to 19 mL. However, using the IW based on the height estimated by the nurse in 11 patients (20%), the TV would have been > 10% (equivalent to values between 44 mL to 80 mL).
The findings of this study suggest that establishing a patient’s height with a laser-based measuring device is an accurate method that is very close to the gold standard. As a matter of fact, it could be a reliable, safe, and easy solution during the management of critically ill patients. However, it can be limited in patients in whom it is contraindicated or when the supine position is not possible.
We wish to thank Dr. Josep Trenado for his ideas and Luis Prieto for his artistic skills.
Please cite this article as: Valls-Matarín J, del Cotillo-Fuente M, Miranda-Ramírez M, Parera-Pous AM. Medidor láser, una alternativa para la determinación de la altura en el paciente crítico. Estudio de concordancia. Med Intensiva. 2021;45:e62–e64.